| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 11, November 2022, pages 458-465
Relationship Between Body Mass Index and Outcomes in Acute Myocardial Infarction
Laith Alhuneafata, Ahmad Jabrib, j, Yazan Abu Omarc, Bryan Margariad, Ahmad Al-abdouhe, Mohammed Mhannaf, Zaid Shahrorig, Nour Hammadh, Abdallah Rayyani, Farhan Nasserb, Meera Kondapanenib, Aisha Sirajb
aDepartment of Medicine, Allegheny Health Network, Pittsburgh, PA, USA
bHeart and Vascular Center, MetroHealth Medical Center, Cleveland, OH, USA
cDepartment of Medicine, Cleveland Clinic, Cleveland, OH, USA
dDepartment of Medicine, MetroHealth Medical Center, Cleveland, OH, USA
eDivision of hospital medicine, University of Kentucky, Lexington, KY, USA
fDepartment of Internal Medicine, University of Toledo, Toledo, OH, USA
gDepartment of Medicine, Hashemite University Amman, Jordan
hDepartment of Nephrology, University Hospitals Cleveland Medical Center, Cleveland, OH, USA
iDepartment of Medicine, University of Jordan School of Medicine, Amman, Jordan
jCorresponding Author: Ahmad Jabri, Heart and Vascular Institute, MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH 44109, USA
Manuscript submitted September 1, 2022, accepted October 31, 2022, published online November 29, 2022
Short title: BMI and Outcomes in AMI
doi: https://doi.org/10.14740/jocmr4818
| Abstract | ▴Top |
Background: The prevalence of obesity in the United States is high. Obesity is one of the leading risk factors in the development of acute myocardial infarction (AMI). Nevertheless, how obesity impacts AMI in-hospital outcomes remains controversial.
Methods: Using National Inpatient Sample (NIS) database, we identified patients diagnosed with AMI from the year 2015 to 2018. We divided these patients into five subgroups based on their body mass index (BMI). We compared outcomes such as mortality, length of inpatient stay, and inpatient complications between our subgroups. Statistical analysis was done using the program STATA. Our nationally representative analysis included 561,535 patients who had an AMI event across various weight classes.
Results: Most of our sample was obese (BMI > 30 kg/m2) and male. Obese patients were significantly younger than the rest. Length of stay (LOS) for AMI was highest for those with a BMI of less than 24 kg/m2. In-hospital mortality is highest for those with a BMI of < 30 kg/m2 and lowest for those with a BMI of 30 - 40 kg/m2. Inpatient complications are highest in the lower BMI population (BMI < 24 kg/m2).
Conclusion: The current analysis of a nationally representative sample showed the clinical implications of BMI in patients with AMI. Patients with a BMI of 30 - 40 kg/m2 had more favorable LOS, inpatient complications, and in-hospital mortality when compared to those with an ideal body weight. Hence, this supports and expands on the concept of the “obesity paradox”. Further studies are needed to further investigate the possible mechanism behind this.
Keywords: Myocardial infarction; BMI; Obesity paradox
| Introduction | ▴Top |
Acute myocardial infarction (AMI) is one of the most prominent complications of cardiac disease [1]. It can present with cardiac arrest, shock, and multiple organ dysfunction [1]. The treatment of AMI usually requires inpatient hospitalization and close monitoring, which places a substantial financial burden not only on the patient but also on the healthcare system as a whole [2]. AMI has been linked with many conditions including obesity [3]. What is not as well understood is the relationship between obesity and outcomes once the AMI has already occurred.
Obesity has been on the rise in the United States over the past decades with its prevalence increasing from 6.2% to 32.7% between 1976 - 1980 and 2017 - 2018 [4]. Obese patients have been shown to incur higher medical costs and burdens which makes it vital to study this risk [5, 6]. The correlation between body mass index (BMI) and cardiac conditions has been well established, yet there remains controversy on whether it is an independent risk factor or not [3, 7, 8]. Obesity is associated with a higher prevalence of co-morbidities, including diabetes, insulin resistance, hyperlipidemia, and hypertension, all of which can be the drivers of this cardiovascular risk [7, 8]. Interesting trends are seen in cardiovascular mortality with obesity. Most recently, a high BMI (> 27.5 kg/m2) has been associated with a protective effect on mortality across all patients that experience an AMI [9, 10].
Several studies have attempted to delve deeper into the correlation between BMI and AMI. A recent meta-analysis of five primary studies showed a clear correlation between obesity and risk for AMI [11]. In addition, underweight patients have been shown to have a higher risk of cardiovascular events including cerebrovascular accidents and AMI [9, 10].
The effect of BMI on morbidity and mortality in AMI is undeniable and further insight into these trends is crucial. This study aims to be the largest retrospective analysis of its kind to break down AMI by BMI, and then also other outcomes such as inpatient complications, mortality, and socioeconomic data.
| Materials and Methods | ▴Top |
This study used data from the NIS database from October 2015 to 2018. The NIS is one of several databases managed by the Agency for Healthcare Research and Quality through a Federal-State-Industry partnership called the Healthcare Cost and Utilization Project (HCUP). The NIS contains administrative claims data from 7 million in-patient hospitalizations annually in 47 participating states plus the District of Columbia, representing 97% of the United States population. Because NIS data are compiled annually, the data can be used for the analysis of disease trends over time using trend weights compiled by the HCUP.
Institutional Review Board approval and informed consent were not required for this study because NIS data are de-identified and publicly available. The research qualifies as no risk or minimal risk to subjects and our institution does not require ethical approval for NIS database studies. We identified hospitalizations for AMI with the International Classification of Diseases, Tenth Revision (ICD-10). We included hospitalizations with a primary diagnosis of AMI and those with a secondary diagnosis of AMI if the primary diagnosis was either percutaneous coronary intervention (PCI) (Z9861 and PCS codes: 0271, 0272, 0273) or coronary artery bypass graft (CABG) surgery (PCS codes: 0211, 0212, 0213) or thrombolytics (3E05017, 3E05317, 3E04017, 5A0935B, 5A09457, 5A09458, 3E04317, 3E05017, 3E05317) or atrial fibrillation (I48.1, I48.2, I48.91) or ventricular tachycardia (I47.2) or ventricular fibrillation (I49.01) or heart failure (I50).
We also identified patients whose BMI codes were collected and divided into five BMI groups: underweight (< 20 kg/m2), normal weight (20 - 24.9 kg/m2), overweight (25 - 30 kg/m2), obese class I and II (31 - 39.9 kg/m2), and obese class III (≥ 40 kg/m2). ICD codes used were Z68.1, Z68.2, Z68.3, and Z68.4. The included population in our analysis were patients aged above 18, who we identified as presenting with an MI as described above and had BMI codes identifying their obesity status.
Descriptive statistics were presented as frequencies with percentages for categorical variables and as means with standard deviations and medians with interquartile ranges for continuous variables. Baseline characteristics were compared using a Pearson Chi-square test, Fisher’s exact test for categorical variables, and the Student’s t-test and Mann-Whitney U test for continuous variables. Multivariate regression analysis was done to adjust for possible confounders while calculating in-hospital mortality. The patient and hospital characteristics, as well as comorbidities, were obtained from the literature review. A univariate screen was done to further confirm these factors. Variables with P < 0.2 on a univariate screen were included in the multivariable regression model. A P-value of 0.05 was set as the threshold for statistical significance in the multivariate regression analysis. All analyses were conducted by weighting samples for national estimates in conjunction with the HCUP regulations for using the NIS database. Statistical analyses were performed using STATA version 17 for Windows and RStudio 2022.02.0.
| Results | ▴Top |
From October 2015 to 2018, 561,520 estimated weighted admissions with AMI were identified. Table 1 shows the baseline characteristics of our AMI hospitalization cohort. Average age was 63 ± 13 years, with gender less likely to be female (n = 233,115 (42%)). The majority of those presenting with AMI were white (397,085 (73%)) and had Medicare insurance (n = 284,825 (51%)). The breakdown according to BMI groups is as detailed in tables.
 Click to view | Table 1. Patient and Hospital Characteristics by Body Mass Index |
Table 2 demonstrates the difference in comorbidities between different groups; most of our cohort had hypertension (n = 486,270 (87%)), with the highest percentage in patients with BMI > 40 kg/m2 (89%, P < 0.001). Diabetes mellitus was also highest in patients with BMI > 40 kg/m2 with an incremental increase in percentage with elevated BMI (21%, 35%, 48%, 54%, and 61%). The presence of chronic kidney disease was higher at both extremes of BMI groups (both at 28%, P < 0.001). Heart failure as a comorbidity was notably higher in lower BMI groups (BMI < 24 (50%, P < 0.001)). Similarly, atrial fibrillation history was higher in those with BMI < 25 kg/m2 (P < 0.001). Stroke and transient ischemic attacks were higher in both BMI groups below 25 kg/m2 (P < 0.001). Charleston comorbidity index was higher in both BMI groups below 25 kg/m2 (P < 0.001).
 Click to view | Table 2. Patient Baseline Comorbidities by Body Mass Index |
Table 3 shows the distribution of the clinical presentation and course, as well as revascularization therapy utilization during hospitalization. Presentation with ST-elevation MI in 21%, non-ST-elevation MI in 71%, and other presentations besides STEMI and NSTEMI were in 3.1% of hospitalizations. Ventricular tachycardia was notable in 6.6% of the cohort, without differences between groups. Ventricular fibrillation was more likely in BMI groups (25 - 29 and > 40 kg/m2) with 3.5% and 3.3% respectively (P < 0.001). PCI was performed in 46% of patients, most commonly in the BMI 30 - 40 kg/m2 group with 51% (P < 0.001). CABG was performed in 13% of all patients, but mostly in BMI > 20 - 29 kg/m2 and BMI 30 - 40 kg/m2 groups with 15% for both (P < 0.001). Systemic thrombolysis was only administered in 1.8% of hospitalizations and more commonly in the lowest BMI group < 20 kg/m2 with 3.9% (P < 0.001).
 Click to view | Table 3. Distribution of Clinical Course and Utilization of Revascularization Procedures by Body Mass Index |
Table 4 shows inpatient complications and resource utilization during the hospital stay. Length of stay (LOS) was longest in the 20 - 24 kg/m2 BMI group with an average stay of 6.7 ± 7 days (P < 0.001). Total admission charges were least for BMI < 20 kg/m2 group with an average of $89,245 per admission. Respiratory failure requiring mechanical ventilation was highest in BMI < 20 kg/m2 group with 7.2% (P < 0.001). Multiple in-hospital complications were highest for 20 - 24 kg/m2 BMI group including upper gastrointestinal (GI) bleeding (4.1%, P < 0.001), acute kidney injury (31%, P < 0.001), circulatory shock (7.7%, P < 0.001), and requiring packed red blood cell (PRBC) transfusion (9.7%, P < 0.001). However, in-hospital mortality was highest in BMI < 20 kg/m2 group with 9.3% (P < 0.001) (Fig. 1) [12].
 Click to view | Table 4. Patient Complications and Resource Utilization by Body Mass Index |
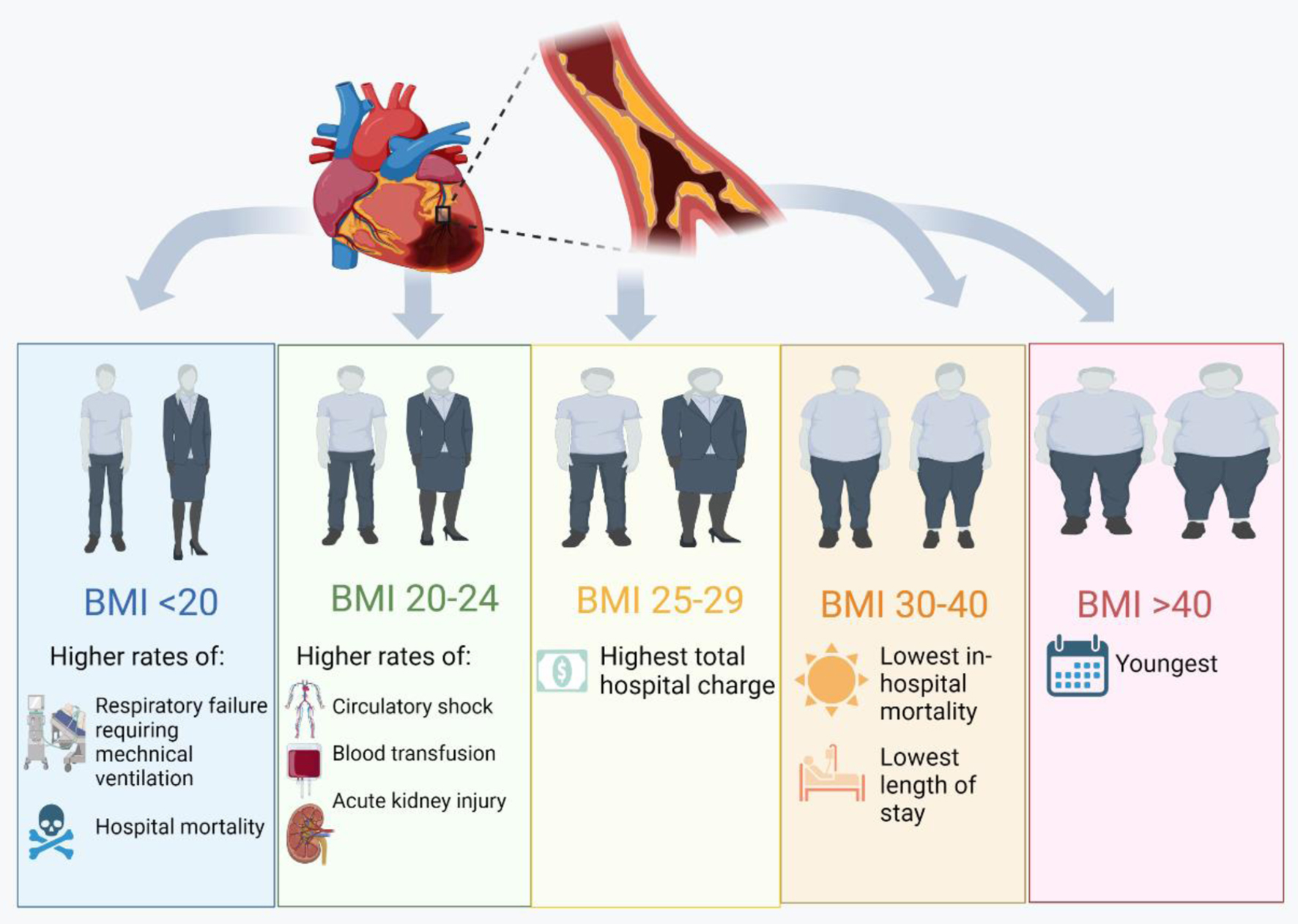 Click for large image | Figure 1. Differences in patient characteristics, resource utilization and in-hospital outcomes among those admitted for acute myocardial infarction based on body mass index [12]. |
Table 5 shows a univariate and multivariate logistic model for risk factors for mortality. Using BMI group < 20 kg/m2 as a baseline, we noticed that higher BMI predicted lower in-patient mortality in AMI patients with the lowest being in the 30 - 40 kg/m2 BMI group. The difference was still maintained even when adjusting for age, gender, and comorbidities. Other variables were assessed; the female gender was found to be protective with odds ratio (OR) 0.88 (95% confidence interval (CI) 0.82 - 0.94, P < 0.001). Atrial fibrillation and heart failure predicted mortality with OR 1.26 (95% CI 1.17 - 1.36, P < 0.001) and OR 2.03 (95% CI 1.89 - 2.18, P < 0.001), respectively.
 Click to view | Table 5. Regression Model for Predictors of Mortality |
| Discussion | ▴Top |
This study is a nationally representative cohort of 561,535 patients who had an AMI event across various weight classes. This analysis examined the relationship between BMI and in-hospital outcomes of patients with AMI. To our knowledge, this is the largest study to explore this relationship. The primary findings were as follows: 1) The majority of our sample was obese (BMI > 30 kg/m2) and male. 2) Obese patients were significantly younger than the rest. 3) LOS for AMI was highest for those with a BMI less than 24 kg/m2. 4) In-hospital mortality is highest in those with a BMI < 25 kg/m2 and lowest for those with a BMI of 30 - 40 kg/m2. 5) Inpatient complications are significantly higher in the lower BMI population.
It is well established that risk factors for having AMI include being obese and male [3, 7]. This study supports these findings as the majority of our sample were male and obese. Despite the male gender being a predictor of decreased mortality in our multivariate analysis, female patients made up most patients who were underweight which is consistent with the literature [13]. Obese patients were more likely to be younger when presenting with AMI, which could be related to obesity being a risk factor for coronary artery disease (CAD). A total of 111,847 patients were involved in a retrospective analysis comparing NSTEMI frequency and risk factors, revealing that excess adipose tissue is a primary risk factor for a premature cardiac event [13, 14]. Obese patients were more likely to have diabetes mellitus and hypertension, as it is well established that obese patients have higher rates of metabolic disease [4, 14, 15]. The higher prevalence of these two additional CAD risk factors in obese patients may also contribute to them presenting at a younger age with AMI than in lower BMI groups [14, 16]. Although these patients’ young age may contribute to the decreased mortality rate in those with class I and II obesity, when we adjusted for age and other patient characteristics, they continued to have lower inpatient mortality rates.
It is well established that patients with STEMI have higher rates of mortality than those with NSTEMI [17-20]. Interestingly despite the two lower BMI groups (< 25 kg/m2) having fewer rates of STEMI, they experienced higher mortality rates. The higher rates of STEMI in class I and II obesity likely also contributed to these patients receiving higher rates of coronary revascularization through PCI and CABG.
When patients who have higher BMI have more favorable outcomes than those with ideal body weight it is often referred to as the “obesity paradox”. This was described in multiple large observational studies in patients presenting with acute coronary syndrome (ACS) [10, 15, 16]. A Swedish registry study of 64,436 ACS patients demonstrated the highest survival rates in those who are overweight in slight contrast to our study which showed that class I and II obesity had the lowest mortality rates [13]. Like our study, Angeras et al showed the highest rate of mortality in the underweight group [13]. A European meta-analysis in 2014 of 218,532 people reinforced this point of significantly higher mortality with lower BMI [10]. Several other studies showed decreased survival rates once BMI went past 40 kg/m2 as also demonstrated by our study [10, 14, 21, 22].
The relationship between a higher BMI and better survival rates post-ACS is not very well understood. One concept proposed is “metabolically healthy obesity”, which indicates despite these patients having large adipose reserves some do not have classic sequela of metabolic disease [23, 24]. Several other mechanisms have been postulated such as improved nutritional and caloric reserve may hinder the metabolic effects of the disease for those who are critically ill [25-28]. Another hypothesis includes the idea that lower weight may represent a severe cardiovascular disease state like cardiac cachexia in heart failure patients [29, 30]. Other studies challenge the use of BMI as a surrogate for excess body fat as it represents both the sum of the fat-mass index and fat-free mass index (skeletal muscle mass, bone, and organs) [31]. They argue that markers of obesity such as waist circumference and waist-to-hip ratio have correlated better with CAD [28].
We examined hospital LOS as it offers information regarding resource utilization and health economics. Patients who had an ideal body weight or were underweight had a higher LOS. LOS was lowest in those with class I and II obesity. A possible mechanism for this would be that higher caloric reserve and improved nutritional status allow for superior healing rates and therefore shorter hospital stays [25].
Limitations
NIS allows for large-scale, real-world, and nationally representative data analysis of hundreds of clinical and non-clinical variables. Despite this, the findings of this study should be interpreted with the following limitations in mind. Firstly, limitations are inherent to the observational nature of this study. Secondly, this study is subject to suboptimal coding or coding errors which could lead to bias. Thirdly, NIS data are limited to in-hospital outcomes, and therefore important information such as 30-day readmission and 30-day mortality is not possible to extract. Fourthly, patients identified with NSTEMI may include a portion of the population with a type 2 MI secondary to myocardial ischemia from mismatched myocardial oxygen supply and demand that is not related to unstable CAD. Moreover, residual confounding due to unmeasured confounders could have influenced the observed results. Due to limitations in our database, we were unable to further define patients’ clinical status with information regarding frailty. Finally, the use of BMI as a surrogate for excess body fat without information regarding waist-to-hip ratio and percent body fat. Unfortunately, the NIS database does not contain these measures of excess body fat.
Conclusion
The current analysis of a nationally representative sample demonstrated the clinical implications of BMI in patients with AMI. Patients with a BMI of 30 - 40 kg/m2 had more favorable LOS, inpatient complications, and in-hospital mortality when compared to those with ideal body weight. Hence, this supports and expands on the concept of the “obesity paradox”. Further studies are needed to further investigate the possible mechanism behind this.
Acknowledgments
Thank you to the MetroHealth medical center research department.
Financial Disclosure
None to declare.
Conflict of Interest
The authors do not have any conflict of interest to disclose.
Informed Consent
Informed consent was not required for this study because NIS data are de-identified and publicly available.
Author Contributions
Laith Alhuneafat: manuscript writing, literature review, editing and review, and submission; Ahmad Jabri: hypothesis, data analysis, manuscript writing, editing and review; Yazan Abu Omar: manuscript editing and data analysis; Bryan Margaria: manuscript writing and editing; Farhan Nasser: data collection, manuscript writing and literature review; Mohammed Mhanna, Ahmad Al Abdouh, Nour Hammad, Farhan Nasser, and Abdallah Rayyan: manuscript writing; Meera Kondapaneni and Aisha Siraj: project supervision and review.
Data Availability
The National Inpatient Sample is the largest publicly available all-payer inpatient care database in the United States, containing data on more than seven million hospital stays. Healthcare Cost and Utilization Project Agency for Healthcare Research and Quality (HCUP AHRQ) has restrictions on data sharing based on a Data Use Agreement any questions should be directed to them.
| References | ▴Top |
- Laslett LJ, Alagona P, Jr., Clark BA, 3rd, Drozda JP, Jr., Saldivar F, Wilson SR, Poe C, et al. The worldwide environment of cardiovascular disease: prevalence, diagnosis, therapy, and policy issues: a report from the American College of Cardiology. J Am Coll Cardiol. 2012;60(25 Suppl):S1-49.
doi pubmed - Nicholson G, Gandra SR, Halbert RJ, Richhariya A, Nordyke RJ. Patient-level costs of major cardiovascular conditions: a review of the international literature. Clinicoecon Outcomes Res. 2016;8:495-506.
doi pubmed - Kim DW, Her SH, Park HW, Park MW, Chang K, Chung WS, Seung KB, et al. Association between body mass index and 1-year outcome after acute myocardial infarction. PLoS One. 2019;14(6):e0217525.
doi pubmed - Ellison-Barnes A, Johnson S, Gudzune K. Trends in obesity prevalence among adults aged 18 through 25 years, 1976-2018. JAMA. 2021;326(20):2073-2074.
doi pubmed - Abramowitz MK, Hall CB, Amodu A, Sharma D, Androga L, Hawkins M. Correction: Muscle mass, BMI, and mortality among adults in the United States: A population-based cohort study. PLoS One. 2018;13(5):e0198318.
doi pubmed - Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood). 2009;28(5):w822-831.
doi pubmed - Matinrazm S, Ladejobi A, Pasupula DK, Javed A, Durrani A, Ahmad S, Munir MB, et al. Effect of body mass index on survival after sudden cardiac arrest. Clin Cardiol. 2018;41(1):46-50.
doi pubmed - Aune D, Schlesinger S, Norat T, Riboli E. Body mass index, abdominal fatness, and the risk of sudden cardiac death: a systematic review and dose-response meta-analysis of prospective studies. Eur J Epidemiol. 2018;33(8):711-722.
doi pubmed - Bucholz EM, Rathore SS, Reid KJ, Jones PG, Chan PS, Rich MW, Spertus JA, et al. Body mass index and mortality in acute myocardial infarction patients. Am J Med. 2012;125(8):796-803.
doi pubmed - Niedziela J, Hudzik B, Niedziela N, Gasior M, Gierlotka M, Wasilewski J, Myrda K, et al. The obesity paradox in acute coronary syndrome: a meta-analysis. Eur J Epidemiol. 2014;29(11):801-812.
doi pubmed - Zhu J, Su X, Li G, Chen J, Tang B, Yang Y. The incidence of acute myocardial infarction in relation to overweight and obesity: a meta-analysis. Arch Med Sci. 2014;10(5):855-862.
doi pubmed - www.biorender.com.
- Angeras O, Albertsson P, Karason K, Ramunddal T, Matejka G, James S, Lagerqvist B, et al. Evidence for obesity paradox in patients with acute coronary syndromes: a report from the Swedish Coronary Angiography and Angioplasty Registry. Eur Heart J. 2013;34(5):345-353.
doi pubmed - Madala MC, Franklin BA, Chen AY, Berman AD, Roe MT, Peterson ED, Ohman EM, et al. Obesity and age of first non-ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2008;52(12):979-985.
doi pubmed - Das D, Asher A, Ghosh AK. Cancer and coronary artery disease: common associations, diagnosis and management challenges. Curr Treat Options Oncol. 2019;20(6):46.
doi pubmed - Oreopoulos A, McAlister FA, Kalantar-Zadeh K, Padwal R, Ezekowitz JA, Sharma AM, Kovesdy CP, et al. The relationship between body mass index, treatment, and mortality in patients with established coronary artery disease: a report from APPROACH. Eur Heart J. 2009;30(21):2584-2592.
doi pubmed - Bouisset F, Ruidavets JB, Dallongeville J, Moitry M, Montaye M, Biasch K, Ferrieres J. Comparison of short- and long-term prognosis between ST-elevation and non-ST-elevation myocardial infarction. J Clin Med. 2021;10(2):180.
doi pubmed - Fokkema ML, James SK, Albertsson P, Aasa M, Akerblom A, Calais F, Eriksson P, et al. Outcome after percutaneous coronary intervention for different indications: long-term results from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). EuroIntervention. 2016;12(3):303-311.
doi pubmed - Chan MY, Sun JL, Newby LK, Shaw LK, Lin M, Peterson ED, Califf RM, et al. Long-term mortality of patients undergoing cardiac catheterization for ST-elevation and non-ST-elevation myocardial infarction. Circulation. 2009;119(24):3110-3117.
doi pubmed - Ren L, Ye H, Wang P, Cui Y, Cao S, Lv S. Comparison of long-term mortality of acute ST-segment elevation myocardial infarction and non-ST-segment elevation acute coronary syndrome patients after percutaneous coronary intervention. Int J Clin Exp Med. 2014;7(12):5588-5592.
- Das SR, Alexander KP, Chen AY, Powell-Wiley TM, Diercks DB, Peterson ED, Roe MT, et al. Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with ST-Segment elevation myocardial infarction results from the NCDR (National Cardiovascular Data Registry). J Am Coll Cardiol. 2011;58(25):2642-2650.
doi pubmed - Neeland IJ, Das SR, Simon DN, Diercks DB, Alexander KP, Wang TY, de Lemos JA. The obesity paradox, extreme obesity, and long-term outcomes in older adults with ST-segment elevation myocardial infarction: results from the NCDR. Eur Heart J Qual Care Clin Outcomes. 2017;3(3):183-191.
doi pubmed - Elagizi A, Kachur S, Lavie CJ, Carbone S, Pandey A, Ortega FB, Milani RV. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2018;61(2):142-150.
doi pubmed - Lavie CJ, Laddu D, Arena R, Ortega FB, Alpert MA, Kushner RF. Healthy weight and obesity prevention: JACC health promotion series. J Am Coll Cardiol. 2018;72(13):1506-1531.
doi pubmed - Oliveros H, Villamor E. Obesity and mortality in critically ill adults: a systematic review and meta-analysis. Obesity (Silver Spring). 2008;16(3):515-521.
doi pubmed - Kalantar-Zadeh K, Horwich TB, Oreopoulos A, Kovesdy CP, Younessi H, Anker SD, Morley JE. Risk factor paradox in wasting diseases. Curr Opin Clin Nutr Metab Care. 2007;10(4):433-442.
doi pubmed - Habbu A, Lakkis NM, Dokainish H. The obesity paradox: fact or fiction? Am J Cardiol. 2006;98(7):944-948.
doi pubmed - Casas-Vara A, Santolaria F, Fernandez-Bereciartua A, Gonzalez-Reimers E, Garcia-Ochoa A, Martinez-Riera A. The obesity paradox in elderly patients with heart failure: analysis of nutritional status. Nutrition. 2012;28(6):616-622.
doi pubmed - Kenchaiah S, Pocock SJ, Wang D, Finn PV, Zornoff LA, Skali H, Pfeffer MA, et al. Body mass index and prognosis in patients with chronic heart failure: insights from the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) program. Circulation. 2007;116(6):627-636.
doi pubmed - Berry C, Clark AL. Catabolism in chronic heart failure. Eur Heart J. 2000;21(7):521-532.
doi pubmed - Donini LM, Pinto A, Giusti AM, Lenzi A, Poggiogalle E. Obesity or BMI paradox? Beneath the tip of the iceberg. Front Nutr. 2020;7:53.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


