| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 11, Number 9, September 2019, pages 623-628
“Yubi-wakka” (Finger-Ring) Test: A Tool to Detect Prefrailty in Elderly Populations, a Pilot Study
Hitomi Fujiia, e, Eitaro Kodanib, Tomohiro Kanekoc, Hiroyuki Nakamurad, Hajime Sasabed, Yutaka Tamurad
aInternal Medicine, Tama-Center Mirai Clinic, 206-0033 1-38 Ochiai Tama City, Tokyo, Japan
bDepartment of Internal Medicine and Cardiology, Nippon Medical School Tama-Nagayama Hospital, Tokyo, Japan
cDepartment of Nephrology, Nippon Medical School Tama-Nagayama Hospital, Tokyo, Japan
dTAMA CITY Medical Association, Tokyo, Japan
eCorresponding Author: Hitomi Fujii, Internal Medicine, Tama-Center Mirai Clinic, 206-0033 1-38 Ochiai Tama City, Tokyo, Japan
Manuscript submitted June 26, 2019, accepted July 23, 2019
Short title: “Yubi-wakka” Test in Checkup
doi: https://doi.org/10.14740/jocmr3917
| Abstract | ▴Top |
Background: Preventing frailty of elderly is an urgent issue in Japan. The “Yubi-wakka” (finger-ring) test was developed and validated as a predictor of sarcopenia, disability and even mortality. To clarify the prevalence of “frailty” defined by this test and the relationship between other indexes cross-sectionally and prospectively, we conducted this study.
Methods: Five thousand four hundred and five subjects who were 65 to 74 years old participated in this study. In a sitting position, the subjects surrounded their calf using their own finger-ring, and whether the calf was larger, just fit, or smaller than the finger-ring was determined. We analyzed these “Yubi-wakka” (finger-ring) test results and other clinical indexes. We used Student’s t-tests and the Chi-squared tests to compare the data between the groups, and logistic regression tests to adjust for multiple variables.
Results: In total, 38.8% of the subjects’ calves were judged as being “larger”, 45.6% as “just fit” and 15.6% as “smaller”, which was the positive test result. The positive rate differed among medical facilities without any known different characteristics. The comparison between the “larger” and “smaller” groups revealed that body weight, red blood cell count, serum lipids, uric acid and liver enzymes were significantly different between the groups. Metabolic syndrome was more common in the “larger” group. In multiple analysis, low body mass index was an independent risk factor in both sexes. Positive urinary glucose, higher aspartate aminotransferase, systolic blood pressure and low alanine transaminase were risk factors for positive test results for males. Smoking, high hemoglobin and old age were risk factors for positive test results in females.
Conclusions: The test was simple and feasible enough for the primary care setting, without the requirement of any devices. However, the positive rate varied among the clinics. The subjects’ age was limited to under 75 years, and the test possibly detected individuals without metabolic syndrome and fatty liver. We are also planning to increase the subjects’ age range and collect data prospectively.
Keywords: Bone/musculoskeletal frailty; Geriatric medicine; Metabolism; Clinical nutrition; Sarcopenia
| Introduction | ▴Top |
In a rapidly aging society such as Japan, detecting the risk of frailty at an earlier stage, preventing its progression and prolonging independent healthy life is crucial. Local governments are trying to reduce these burdens through the implementation of lifestyle modifications and interventions. In Tama City, a western suburb of Tokyo, the doctors’ association (TAMA CITY Medical Association) decided to participate in the study by implementing the “Yubi-wakka” (finger-ring) test along with the annual checkup in the 2017 fiscal year. The test needs to be validated to be feasible enough for primary care providers in ordinary practice and sensitive enough to detect current sarcopenia and the likelihood of frailty in the future.
“Yubi-wakka” (finger-ring) test was developed as a “practical and cost-saving” self-check method by Professor Iijima et al [1] and was validated for its ability to identify the risk of sarcopenia, disability and mortality in the future.
| Materials and Methods | ▴Top |
Study design of TAMA MED project-frail
The TAMA MED projects (project atrial fibrillation [2], chronic kidney disease and frail) by the TAMA CITY Medical Association (local doctors’ association) have been conducted to analyze the annual national insurance checkup data from consecutive years as a retrospective cohort study. Project-frail was just initiated by this pilot study, and prospective and financial studies are planned in the future. All authors have contributed significantly and that all authors are in agreement with the content of the manuscript.
Ethical consideration
Since our research is based on the results of the annual checkup of national insurance in Tama City, and Tama City and TAMA CITY Medical Association opted out as informed consent for examinees that this checkup data would be possibly used for the researches, anonymously analyzed and published, and they had the right to refuse. Our study was conducted in accordance with the Declaration of Helsinki (as revised in Brazil 2013). We obtained the IRB approval of Tama-Center Mirai Clinic and Nippon Medical School Tama-Nagayama Hospital.
Subjects
We selected the subjects for this first cross-sectional pilot study from the examinees undergoing a national insurance annual checkup and limited their age to between 65 and 74 years old: the upper age range of individuals participating in this checkup. The examinations were performed mainly at the primary care clinics in the private sector. The primary care doctors were asked to perform the “Yubi-wakka” (finger-ring) test, but the test was not mandatory. A total of 5,405 data points (from 72.7% of all examinees of this age range) were obtained.
Methods
“Yubi-wakka” (finger-ring) test
The detailed method of this test is explained elsewhere [1, 3]; briefly, the examinee surrounded his or her non-dominant calf using their own finger-ring (both thumbs and index fingers), while they were in a sitting position, and whether the calf was “larger”, “just fit” or “smaller” than the finger-ring was determined. At the beginning of the study, a written request for the registered local practitioners to participate in this study was delivered. The request also explained how to perform this method using pictures.
National insurance annual checkup in Tama city
Anthropologic data such as body height, weight, waist circumference and blood pressure were measured. Blood (nutritional, liver, kidney, lipids, glucose, blood cell counts, etc.) and urine samples were taken along with simple medical history questions.
Statistical analysis
We analyzed the relationships between the “Yubi-wakka” (finger-ring) test results and the other data. We excluded the intermediate, “just fit” group and compared the remaining two groups (“larger” and “smaller”). We used Student’s t-tests to compare the groups and the Chi-squared analysis to analyze prevalence. We used a logistic regression test to adjust for multiple variables. These statistical analyses were performed using SPSS version 23.0 (IBM, Armonk, NY, USA).
| Results | ▴Top |
We obtained 5,405 data points. In total, 38.8% of the subjects’ calves were judged as “larger” than their finger-ring, 45.6% of the subjects were in the “just fit” group and 15.6% were in the “smaller” group (Table 1). More than 30 clinics participated in this pilot study. The positive rate (the prevalence of the subjects who were in the “smaller” group) varied from 6.3% to 34.6% (Fig. 1). The positive rate was not related to the number of examinees, age, female sex, or diabetes.
 Click to view | Table 1. Distribution of Results of Finger-Ring Test |
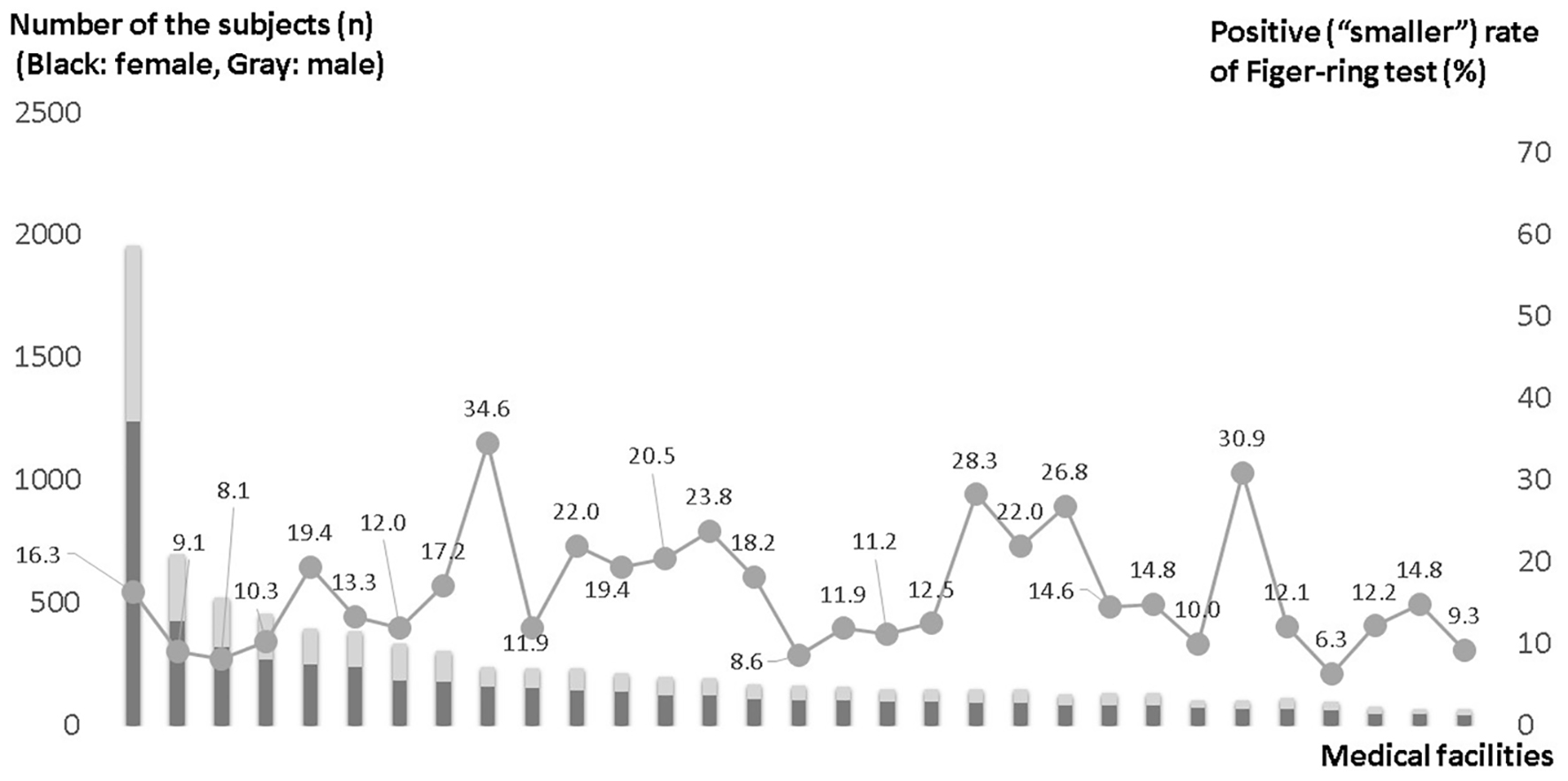 Click for large image | Figure 1. Positive rate of finger-ring test among medical facilities. |
Table 2 shows the comparison of anthropologic data between the “larger” and “smaller” groups in both sexes. Comparing the “smaller” group (positive) to the “larger” group, it was found that in the “smaller” group, the average height was higher, the average body weight was lower and they tended to lose weight in consecutive years. The blood pressure in the females was lower.
 Click to view | Table 2. Comparison of Anthropological Data Between “Larger” and “Smaller” Groups |
The average body mass index (BMI) of the “larger” group was greater than 24, and the average waist circumference was 89 cm in males.
The positive group had lower HbA1c levels and lower red blood cell counts in both sexes; higher high-density lipoprotein cholesterol (HDL-C) levels and lower triglyceride, alanine transaminase (ALT) and uric acid levels were also observed. Creatinine was not significantly different, but creatinine kinase and albumin levels were lower in males (Table 3).
 Click to view | Table 3. Comparison of Serological Data Between “Larger” and “Smaller” Groups |
The Japanese definition of metabolic syndrome (MetS) is the presence of central obesity combination with any two of the following conditions: elevated triglycerides (≥ 150 mg/dL); lowered HDL-C (< 40 mg/dL); elevated blood pressure (systolic blood pressure ≥ 130 mm Hg and/or diastolic blood pressure ≥ 85 mm Hg); and raised fasting glucose (≥ 110 mg/dL). Cutoff level used for the waist circumference to define central obesity is 85 cm for male and 90 cm for female [4]. Pre-MetS was defined as central obesity with one positive among other conditions. The prevalence of MetS and pre-MetS was significantly higher in the “larger” group (Table 4).
 Click to view | Table 4. Distribution of the Metabolic Syndrome (%; Chi-Squared Test) and Pre-MetS in “Lager” and “Smaller” Groups |
A logistic regression test was performed (Table 5). Low BMI was an independent risk factor in both sexes. Positive urinary glucose, higher aspartate aminotransferase (AST) and systolic blood pressure and low ALT were risk factors for positive test results for males. Smoking, high hemoglobin and old age were risk factors for positive test results in females.
 Click to view | Table 5. Multiple Logistic Regression Analysis of the Positive Results of the Finger-Ring Test |
| Discussion | ▴Top |
Although the “Yubi-wakka” (finger-ring) test was described in the original paper [1] as a self-screening tool, it was expected to be performed in a half-self-screened manner under the observation of medical staff in an ordinary primary care setting. However, the medical staff only read the explanation and were not trained for the test.
Compared to the description in the original paper [1], the average age was similar at 70 years, and the positive rate, judged as “smaller”, seemed to be the same in males but higher in females (17% vs. 15%) in our population. Additionally, the proportion of those in the “larger” group was lower (39% vs. 53%), and the proportion of participants in the “just fit” group was larger in our population (46% vs. 33%). We considered that one of the reasons for these differences was a difference in the subject characteristics. In the original paper [1], subjects were invited to the cohort study, so there was likely a participant bias. On the other hand, annual checkup examinees are relatively health-conscious, but more than 60% of them visit clinics regularly because of chronic diseases, such as hypertension, hyperlipidemia and diabetes. Additionally, the positive rate differed from 6.3% to 34.6% among clinics. We could not find differences in the examinees’ backgrounds; however, an older clinic might attend patients with a longer duration of illness. Additionally, there might have been unknown methodological differences in some clinics.
Because of the uncertainty of the methodology, we excluded the intermediate “just fit” group and selected the “larger” and “smaller” groups for comparison.
“Yubi-wakka” (finger-ring) is considered to be a method to adjust for body size differences by using the finger-ring of the individual being examined; however, taller people have relatively larger finger-ring circumferences, so they tended to be classified as “smaller”.
Because of the age limitation of the national insurance checkups, the age range of 65 to 75 years might be too young to detect frailty. In fact, the “larger” group accounted for 40% of all subjects, and their average BMI and waist circumference were the same as the criteria for obese and MetS. Creatinine kinase and AST could be markers of muscle mass, and ALT might be related to fatty liver. Almost 40% of all patients would benefit from the modifying multiple risk factors, such as obesity, high blood pressure, high plasma glucose, elevated lipids and fatty liver, rather than undergoing an intervention for the prevention of frailty.
From the results of multiple regression analysis, the relationship between low body weight and the existence of urinary glucose was understandable. Liver function may be related to fatty liver and/or alcohol consumption. The reason for the positive relationship between systolic blood pressure and hemoglobin in the “smaller” group is also unknown. Because this study was cross-sectional, we could not explain the causal relationship, but atherosclerosis, chronic inflammation, kidney function, etc. can be comorbidities of sarcopenia.
An intervention for the “smaller” group to prevent frailty could be useful because many of the individuals in the “smaller” group already had a comorbidity, and the risk of frailty in the future was proven in a previous study [1].
Changing the definition of old age [5] from 65 to 75 has been considered. The health status of elderly individuals has generally improved. The problem of frailty and disability has not disappeared but has carried over to older generations.
The health status of older generations varies, and individual problems should be carefully evaluated.
Although the “Yubi-wakka” (finger-ring) test is simple enough for us to perform and saves both time and cost, it does not directly measure muscle strength or muscle mass, and it also cannot identify “sarcopenic obesity”.
We are planning to continue this test in annual checkups on occasion prospectively and to expand to the older generation to evaluate the suitability of this test for implementation as a city policy.
Acknowledgments
We would like to thank Prof. Katsuya Iijima, who developed the “Yubi-wakka” test, for giving advice and permission to use the test. We also thank Mr. Junichi Murata for the statistical analysis and the medical association members, the examinees and the local government of Tama City.
Financial Disclosure
The TAMA MED project-frail is supported by the TAMA CITY Medical Association. The sponsors had no role in the design and conduct of the study; in the collection, analysis and interpretation of data; in the preparation of the manuscript; or in the review or approval of the manuscript.
Conflict of Interest
EK received remuneration from Daiichi-Sankyo, Bristol-Myers Squibb and Ono Pharmaceutical.
Informed Consent
Not applicable.
Author Contributions
HF performed research including data collection, analysis and wrote the paper. HN, HS and YT performed research including data collection, and participated discussion. HT and EK designed research, study and provided expert clinical knowledge to revise critically.
| References | ▴Top |
- Tanaka T, Takahashi K, Akishita M, Tsuji T, Iijima K. "Yubi-wakka" (finger-ring) test: A practical self-screening method for sarcopenia, and a predictor of disability and mortality among Japanese community-dwelling older adults. Geriatr Gerontol Int. 2018;18(2):224-232.
doi pubmed - Kodani E, Kaneko T, Fujii H, Nakamura H, Sasabe H, Tamura Y, Shimizu W. Prevalence and incidence of atrial fibrillation in the general population based on National Health Insurance Special Health Checkups- TAMA MED Project-AF. Circ J. 2019;83(3):524-531.
doi pubmed - Hiraoka A, Izumoto H, Ueki H, Yoshino T, Aibiki T, Okudaira T, Yamago H, et al. Easy surveillance of muscle volume decline in chronic liver disease patients using finger-circle (yubi-wakka) test. J Cachexia Sarcopenia Muscle. 2019;10(2):347-354.
doi pubmed - Matsuzawa Y. Metabolic syndrome - definition and diagnostic criteria in Japan. J Atheroscler Thromb. 2005;12(6):301.
doi pubmed - Ouchi Y, Rakugi H, Arai H, Akishita M, Ito H, Toba K, Kai I, et al. Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr Gerontol Int. 2017;17(7):1045-1047.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


