| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 11, Number 9, September 2019, pages 629-634
Relation Between Central Venous, Peripheral Venous and Arterial Lactate Levels in Patients With Sepsis in the Emergency Department
Dimitrios Velissarisa, b, Vasileios Karamouzosc, Nikolaos Dimitrios Pantzarisd, Ourania Kyriakopouloub, Charalampos Gogosa, Menelaos Karanikolase, f
aInternal Medicine Department, University Hospital of Patras, Greece
bEmergency Department, University Hospital of Patras, Greece
cDepartment of Intensive Care Unit, University Hospital of Patras, Greece
dYork Teaching Hospital NHS Foundation Trust, York, UK
eDepartment of Anesthesiology, Washington University School of Medicine, St. Louis, MO, USA
fCorresponding Author: Menelaos Karanikolas, Department of Anesthesiology, Washington University School of Medicine, 660 S. Euclid Ave, Campus Box 8054, St. Louis, MO 63110, USA
Manuscript submitted June 11, 2019, accepted July 16, 2019
Short title: Arterial, Peripheral and Central Venous Lactate
doi: https://doi.org/10.14740/jocmr3897
| Abstract | ▴Top |
Background: Sepsis and multi-organ failure remain a major clinical problem with high morbidity and mortality worldwide. Lactate measurement remains part of the initial assessment and management of patients with sepsis. Although arterial blood is most commonly used for lactate measurement, there is increasing use of peripheral venous lactate for initial assessment and for monitoring of response to treatment in patients with sepsis. The aim of this study was to evaluate the relation between lactate levels measured from central line, peripheral vein and arterial line in patients treated for sepsis in the emergency department (ED).
Methods: This prospective study enrolled 31 patients with diagnosis of sepsis who were evaluated and treated in the ED of a university hospital. During initial resuscitation, blood samples from the artery, peripheral vein and central vein (when available) were collected and lactate concentrations were measured. Correlation between lactate values from the three different locations was assessed using Pearson correlation. Bland-Altman plots were used to evaluate agreement between lactate measurements in different sampling locations. All patients were eventually admitted to the Internal Medicine Department ward or to the intensive care unit (ICU) for further treatment.
Results: Our data showed strong, highly significant correlation between arterial and peripheral venous lactate levels (r = 0.880, P < 0.0001), between arterial and central venous blood lactate (r = 0.898, P < 0.0001) and between central and peripheral venous blood lactate (r = 0.941, P < 0.0001).
Conclusions: In this study we observed strong correlation between arterial, central vein and peripheral vein lactate concentrations in 31 patients assessed and treated for sepsis. We suggest that lactate measurement in peripheral venous blood could be used for screening and for monitoring response to therapy in sepsis patients. However, because this is a small study in only 31 patients and published data are limited, larger studies are needed in order to confirm the validity of our findings.
Keywords: Sepsis; Arterial lactate; Peripheral venous lactate; Central venous lactate; Monitoring; Resuscitation
| Introduction | ▴Top |
Sepsis and the resulting multi-organ failure are still associated with high morbidity and mortality rates [1]. The management of patients with sepsis should begin in the emergency department (ED) in accordance with the international guidelines of the Surviving Sepsis Campaign [2]. Serial lactate concentration measurements are helpful in evaluating the progression of sepsis and can guide decision-making by clinicians.
Most clinicians use arterial blood samples to measure lactate levels. However, in the ED setting and especially in conscious patients, arterial puncture causes patient discomfort and also has a small risk of arterial injury or other complications, including thrombosis and ischemia [3]. As an alternative to arterial sampling, clinicians sometimes use repeated lactate measurements via peripheral or central veins when available, and peripheral venous lactate sampling has been used as part of routine blood testing in some cases [4, 5]. However, only a few studies have evaluated the role of venous blood lactate measurements as alternative to arterial blood sampling. The aim of this study is to evaluate the interchangeability of the arterial blood lactate with the peripheral venous lactate and the central venous lactate (CV-lactate) in patients with sepsis treated in the ED.
| Materials and Methods | ▴Top |
This prospective study was conducted in the Emergency Department of the University Hospital of Patras, in Western Greece, between November 2017 and May 2018 and enrolled 31 patients. Inclusion criteria were age > 18 years and diagnosis of sepsis of any origin confirmed by clinical examination, laboratory tests, radiographic findings (e.g. chest X-ray) or any other intervention performed in the ED.
Exclusion criteria were known liver or renal failure, and metformin use. The diagnosis of sepsis was established according to the recently published Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) definitions criteria [6]. All patients were assessed and treated in the resuscitation room of the ED in accordance with the initial resuscitation guidelines of the Surviving Sepsis Campaign [2].
A central line was inserted in patients with poor peripheral access and in patients who required support with continuous infusion of vasopressors for resuscitation purposes. Three separate blood samples were simultaneously obtained from central and peripheral veins and arterial sampling for lactate analysis. All blood samples were immediately analyzed in a point of care blood gas analyzer (Stat Profile pHOx Ultra TM/CCXTMLactate Membrane Kit, NOVA BIOMEDICAL, Waltham, MA, USA).
The study was conducted in compliance with the ethical standards of the responsible institution on human subjects and with the Helsinki Declaration. The study protocol was approved by the Institutional Review Board of the University Hospital. All patients (or their legal guardian) gave written informed consent before enrolling in the study. Data collected for the study were anonymized and stored in an encrypted electronic database. The medical team involved in the study included University of Patras faculty, resident physicians rotating through the ED and outside consultants.
Statistical analysis
All patient data were anonymized, entered in a secure electronic database and stored in a secure, encrypted personal computer. Data were analyzed using the MedCalc Statistical Software version 18.11.6 (MedCalc Software bvba, Ostend, Belgium; https://www.medcalc.org; 2019). Normality of data distribution was assessed using the Kolgomorov-Smirnov test. Repeated measures analysis of variance (ANOVA) was used to compare lactate levels in arterial blood versus peripheral vein versus central vein samples, and paired t-test was used for post hoc analysis when indicated.
Correlation between lactate values from the three different locations was assessed using Pearson correlation. When correlations were significant, linear regression analysis was conducted in order to assess how well the values of one variable (on the X axis) can predict the values of the other variable (on the Y axis). Data are presented as mean ± standard deviation (SD) or as median (min, max) as appropriate. P < 0.05 was considered statistically significant for all analysis. Bland-Altman plots were generated to evaluate agreement in lactate measurements between the three different sampling locations.
| Results | ▴Top |
In total, 31 patients were included in the study. Data were collected from 31 patients, 13 men and 18 women. Patient age was 75.1 ± 9.7 for men versus 79.1 ± 14 for women, and there were no significant differences between men and women. Lactate levels were measured in arterial blood in 26 patients, in central venous blood in 16 patients and in peripheral venous blood in 29 patients. As a result, we could compare and correlate arterial versus peripheral vein samples in 26 patients, but we had data from all three sources in only 13 patients.
Comparison between variables using repeated measures ANOVA showed that there was no significant difference between lactate levels in arterial (3.08 ± 1.56) versus peripheral venous (3.1 ± 1.78) versus central venous blood (3.22 ± 1.92, P > 0.8, Fig. 1).
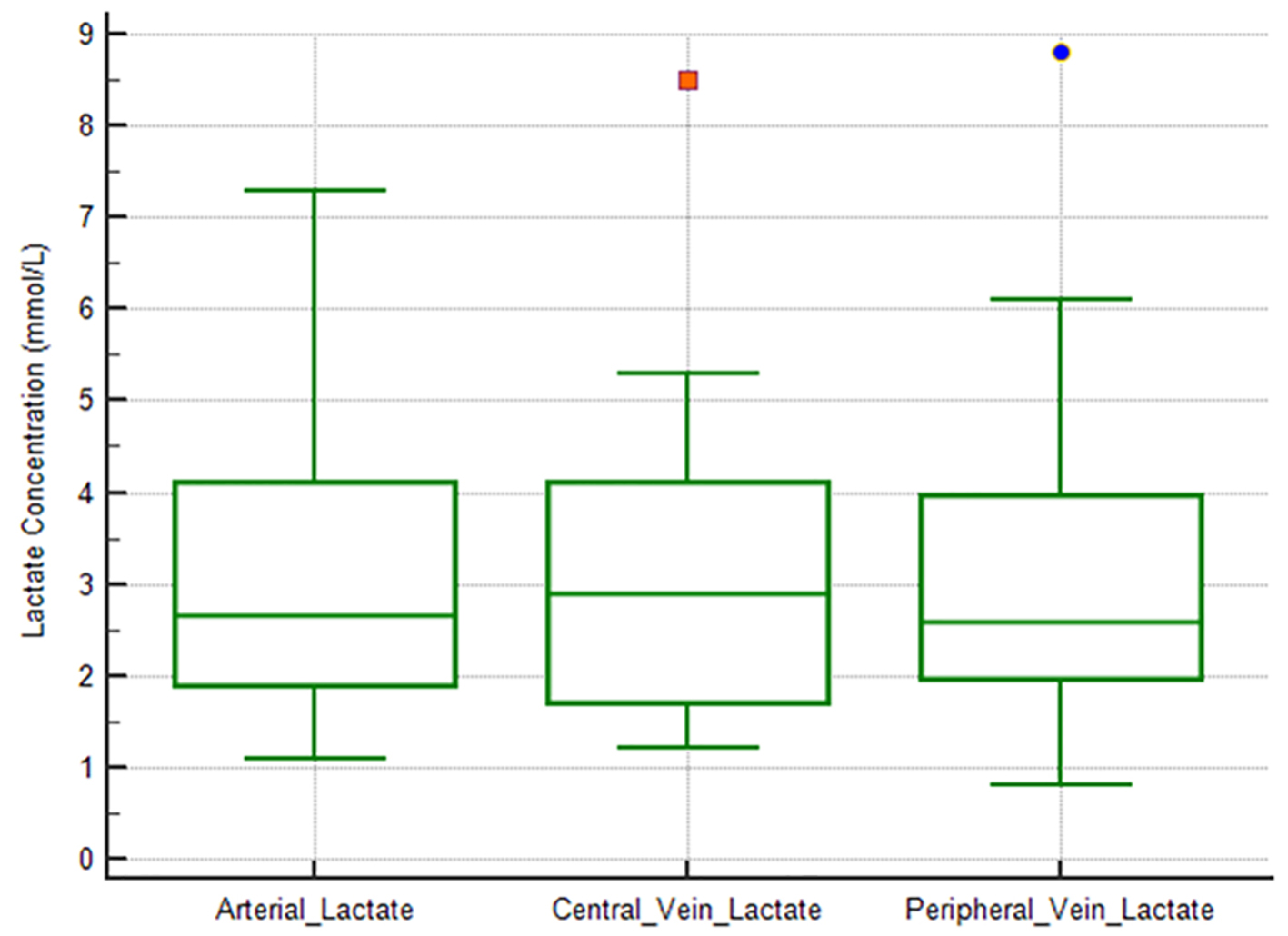 Click for large image | Figure 1. Box-plot diagrams comparing arterial versus central vein versus peripheral vein lactate levels. There are no significant differences between the three sample sites. |
There was very strong, highly significant correlation between arterial and peripheral venous lactate levels (Pearson’s r = 0.880, P < 0.0001), between arterial and central venous blood (Pearson’s r = 0.898, P < 0.0001) and between central and peripheral venous blood (Pearson’s r = 0.941, P < 0.0001). Results of correlation analysis for lactate concentrations in different samples are summarized in Table 1.
 Click to view | Table 1. Correlations Between Arterial, Peripheral Vein and Ventral Vein Lactate Values |
Regression analysis showed that lactate concentration in peripheral vein blood is a strong, highly significant but imperfect predictor of lactate concentration in arterial blood (r = 0.88, P < 0.001, Fig. 2a) and in central venous blood (r = 0.94, P < 0.001, Fig. 2b). Regression analysis also showed that lactate concentration in central vein blood is a strong, highly significant but imperfect predictor of lactate concentration in arterial blood (r = 0.90, P < 0.001, Fig. 2c).
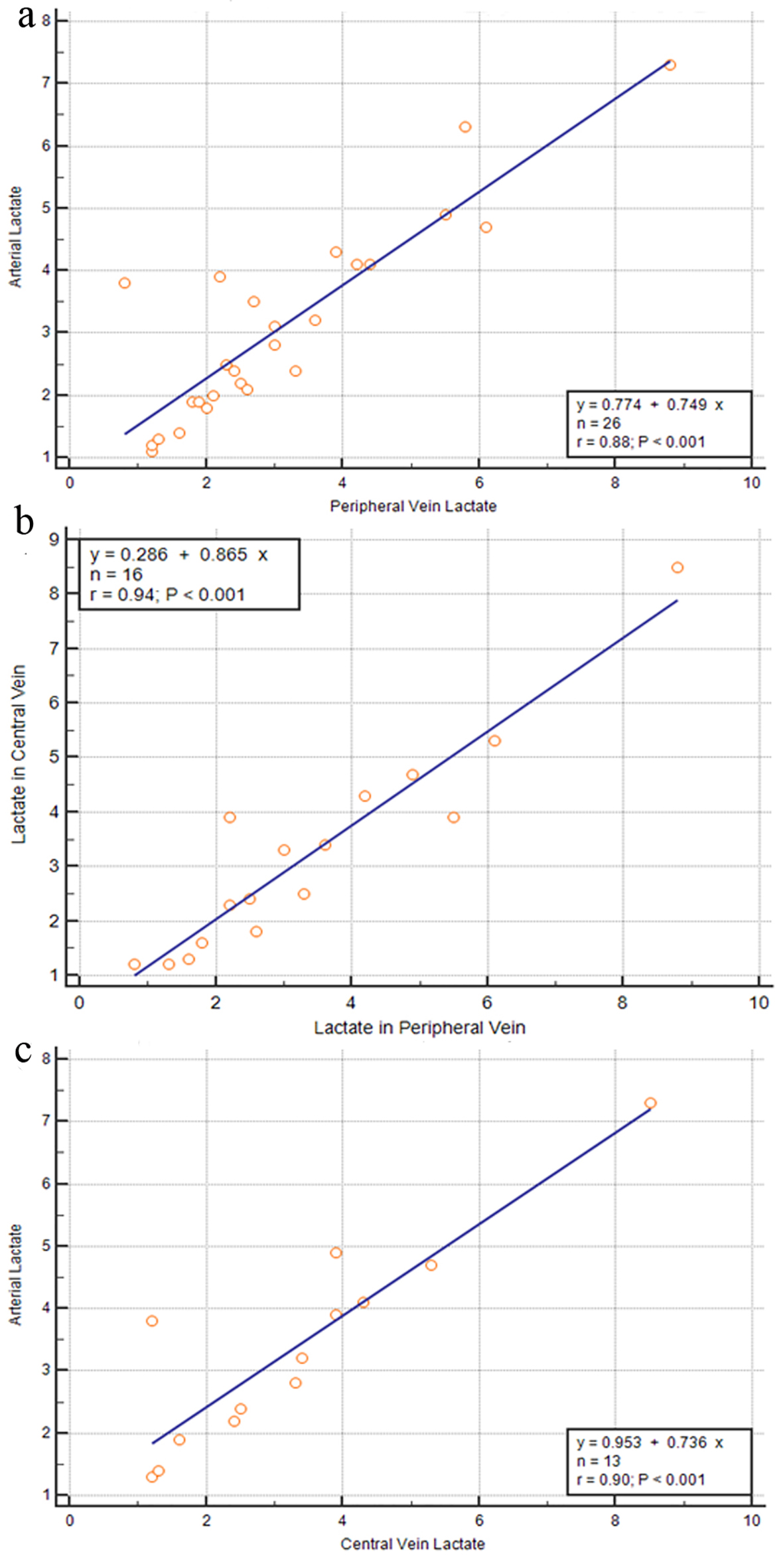 Click for large image | Figure 2. Linear regression analysis: peripheral blood lactate is a strong, highly significant but imperfect predictor of arterial blood lactate (r = 0.88, P < 0.001) (a), peripheral vein lactate is a strong, highly significant but imperfect predictor of central vein lactate (r = 0.94, P < 0.001) (b), and central vein lactate is a strong, highly significant but imperfect predictor of arterial blood lactate (r = 0.90, P < 0.001) (c). |
Bland-Altman plot analysis showed good agreement between lactate concentration in central vein and that in peripheral vein (Fig. 3a), between lactate concentration in central vein and that in arterial blood (Fig. 3b), and between lactate concentration in peripheral vein and that in arterial blood (Fig. 3c).
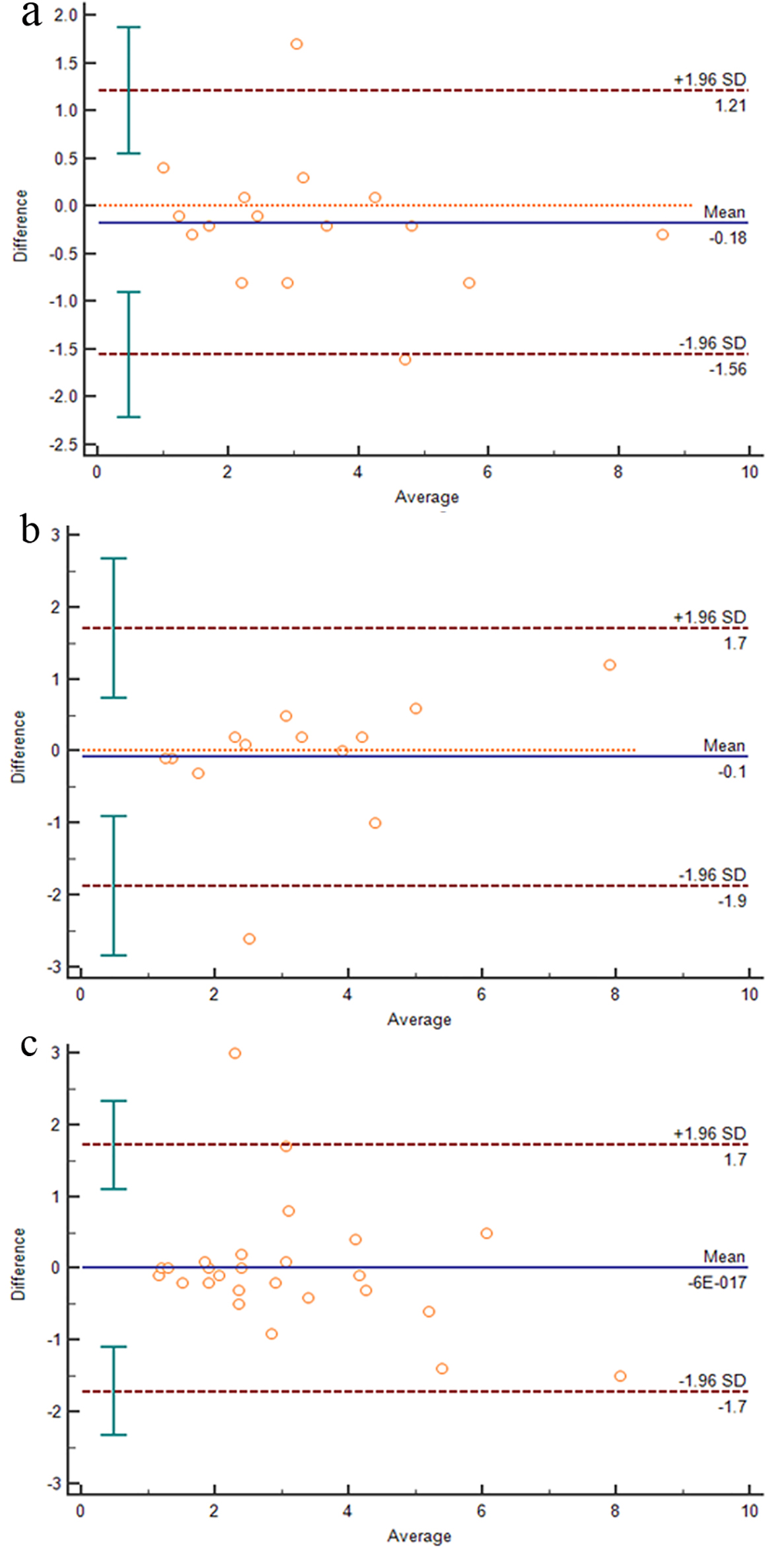 Click for large image | Figure 3. Bland-Altman plot shows good agreement between central vein lactate and peripheral vein lactate (a), between central vein lactate and arterial blood lactate (b) and between arterial blood lactate and peripheral vein lactate (c). |
| Discussion | ▴Top |
The sepsis syndrome has complex underlying pathophysiology with severe cellular and metabolic abnormalities leading to cellular metabolism imbalance resulting in increased lactate production [7]. When tissue hypoxia exists, lactate is overproduced due to increased anaerobic glycolysis, while lactate clearance occurs mostly in the liver (60%), followed by the kidney (30%). The lactate clearance cannot overcome the increased lactate production during the critically ill status. Because liver dysfunction and kidney injury elevate lactate levels due to decreased lactate clearance, we exclude patients with these underlying conditions from our study.
Blood lactate levels can be used as marker for systemic tissue hypoperfusion and disease severity in sepsis: in one large retrospective study from the Netherlands, a 24-h mean lactate > 2 mmol/L was a strong predictor of intensive care unit (ICU) mortality [8], and the range of lactate values reported in this study were quite similar to the lactate values reported in our study.
Serum lactate concentration is included in the criteria for septic shock defined in Sepsis-3 [6]. Lactate level > 2 mmol/L (18 mg/dL) after adequate fluid resuscitation and the need for vasopressor therapy in order to maintain mean arterial pressure > 65 mm Hg characterize septic shock [6, 9]. Most published research has focused on lactate level measurements using arterial blood sampling in ED patients with sepsis. However, in the newer definition of septic shock, venous blood lactate levels seem to accurately reflect the abnormal cell-based metabolism and lactate levels can be considered as emerging vital signs [10].
In this prospective observational single center study, we saw a strong, clinically relevant and statistically highly significant correlation between lactate levels measured in the peripheral artery, central and peripheral veins during initial resuscitation in patients with sepsis. These results are in agreement with the findings of a prospective observational study published by Datta et al in 2018, which demonstrated good agreement between arterial lactate and peripheral lactate levels when lactate levels were > 2 mmol/L in 304 patients with sepsis [11]. Strengths of our study include prospective study design and biologically plausible, highly significant, clinically relevant results. Limitations of our study include the small sample size and the fact that we did not categorize patients based on a specific threshold for lactate concentrations.
Early goal-directed resuscitation protocols used for treatment of patients with sepsis and septic shock aim at reducing mortality [12]. Clinicians often use serial blood lactate level measurements in order to assess disease progression, and arterial puncture samples are most commonly used for lactate level measurement in the blood gas analyzer. However, repeated arterial punctures cause patient discomfort or pain and are associated with small risk of complications, including damage of the artery, bleeding and arterial thrombosis with hand ischemia. Peripheral venous and central venous blood samples can easily be obtained by healthcare professionals with various degrees of skill and experience, have lower risk of complications and sampling is less painful for patients. In cases where placement of a central line is necessary, there are more risks during central line insertion, but fewer disadvantages afterwards.
Based on earlier publications that have demonstrated strong but imperfect agreement between arterial and venous lactate levels [6], use of peripheral vein lactate has been recommended for screening in patients with sepsis [11]. However, we did not identify any publications evaluating the agreement between arterial, venous and central venous lactate levels in patients with sepsis.
In conclusion, based on the strong agreement between venous, arterial and central venous lactate values in our data, it may be reasonable to use peripheral venous or central venous blood samples for measuring lactate levels in order to monitor disease progression and response to therapy in patients with sepsis. However, because this is a small, single center study, additional larger studies are needed to confirm or disprove the validity of our findings.
Acknowledgments
None to declare.
Financial Disclosure
This clinical research project was supported solely by department funds, without any support by industry.
Conflict of Interest
All authors state that they have no conflict of interest to report.
Informed Consent
All patients (or their legal guardian) gave written informed consent before enrolling in the study.
Author Contributions
DV treated patients, collected data, did literature review and wrote the manuscript; VK treated patients, did statistical analysis and revised the manuscript; NDP collected data and did literature review; OK collected data and did literature review; CG supervised the study and revised the manuscript; MK did literature review, analyzed data and revised the manuscript
| References | ▴Top |
- Stevenson EK, Rubenstein AR, Radin GT, Wiener RS, Walkey AJ. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis*. Crit Care Med. 2014;42(3):625-631.
doi pubmed - Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36(1):296-327.
doi pubmed - Giner J, Casan P, Belda J, Gonzalez M, Miralda RM, Sanchis J. Pain during arterial puncture. Chest. 1996;110(6):1443-1445.
doi pubmed - Gallagher EJ, Rodriguez K, Touger M. Agreement between peripheral venous and arterial lactate levels. Ann Emerg Med. 1997;29(4):479-483.
doi - Younger JG, Falk JL, Rothrock SG. Relationship between arterial and peripheral venous lactate levels. Acad Emerg Med. 1996;3(7):730-734.
doi pubmed - Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801-810.
doi pubmed - Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. 2003;348(2):138-150.
doi pubmed - Houwink AP, Rijkenberg S, Bosman RJ, van der Voort PH. The association between lactate, mean arterial pressure, central venous oxygen saturation and peripheral temperature and mortality in severe sepsis: a retrospective cohort analysis. Crit Care. 2016;20:56.
doi pubmed - Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369(18):1726-1734.
doi pubmed - Lee SM, An WS. New clinical criteria for septic shock: serum lactate level as new emerging vital sign. J Thorac Dis. 2016;8(7):1388-1390.
doi pubmed - Datta D, Grahamslaw J, Gray AJ, Graham C, Walker CA. Lactate - Arterial and Venous Agreement in Sepsis: a prospective observational study. Eur J Emerg Med. 2018;25(2):85-91.
- Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368-1377.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


