| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Review
Volume 10, Number 10, October 2018, pages 737-742
Type 2 Diabetes and Glycemic Variability: Various Parameters in Clinical Practice
Masaya Sakamoto
Division of Diabetes, Metabolism and Endocrinology, Department of Internal Medicine, Jikei University School of Medicine, 3-25-8, Nishi-Shinbashi, Minato-ku, Tokyo, 105-8461, Japan
Manuscript submitted August 1, 2018, accepted August 14, 2018
Short title: Type 2 Diabetes and Glycemic Variability
doi: https://doi.org/10.14740/jocmr3556w
- Abstract
- Introduction
- Glycemic Variability
- Short-Term Glycemic Variability
- Intermediate-Term Glycemic Variability
- Long-Term Glycemic Variability
- Glycemic Variability and Prognosis of Type 2 Diabetes
- Conclusions
- References
| Abstract | ▴Top |
It has become possible to measure blood glucose levels continuously from 24 h to approximately 2 weeks due to the recent development of relevant devices such as continuous glucose monitoring and flash glucose monitoring systems. This has enabled not only medical professionals but also patients to monitor details of glycemic variability (GV) which was not possible in the past. Details of GV for both short and intermediate periods can now be obtained, and it is important in patient care to appropriately evaluate the data obtained. Types of GV in terms of time frame vary from short-term to long-term. Several studies reported that long-term GV was related to micro- and macro-angiopathies in patients with type 2 diabetes mellitus (T2DM). However, there are still unknown aspects regarding the relationships of various durations of GV with prognosis. Further clinical trials are required to examine the mechanism of GV and to evaluate whether GV can be a valuable therapeutic target in treatment of patients with T2DM.
Keywords: Glycemic variability; Short-term glycemic variability; Mean of daily difference; Long-term glycemic variability; Visit-to-visit HbA1c variability; Continuous glucose monitoring; Type 2 diabetes mellitus
| Introduction | ▴Top |
The importance of controlling blood glucose levels to prevent cardiovascular events in patients with type 2 diabetes is not a new concept [1, 2]. On the other hand, mortality rates were not decreased in recent clinical trials that set strict HbA1c control targets or, contrary to expectation, the mortality rate was reported to be higher in an intensive-therapy group than in a standard-therapy group [3-5]. One of the causes was attributed to hypoglycemia from short-term treatment intensification. It was also found that hypoglycemia can induce hyperglycemia associated with activation of sympathetic nerve activity, namely, increasing glycemic variability (GV), and adversely affect the cardiovascular (CV) system [6]. Suppression of GV, primarily related to postprandial hyperglycemia, has been considered to be clinically important since postprandial hyperglycemia is involved in the onset of CV events [7, 8]. In recent years, however, because of the availability of a variety of anti-diabetes drugs, it is now easier to decrease blood glucose levels than previously. As a result, hypoglycemia is triggered more frequently; therefore, the importance of suppressing GV, including reactive hyperglycemia as mentioned above, is growing. However, the conventional method for evaluating GV required the collection of blood samples at each clinic visit, which was cumbersome. However, blood glucose levels can now be measured continuously from 24 h to approximately 2 weeks due to the recent development of relevant devices [9, 10]. This has enabled not only medical professionals but also patients to monitor details of GV that could not be monitored in the past. This development resulted in obtaining details of GV for both short and intermediate periods, and it is important to appropriately evaluate the data obtained. Meanwhile, many aspects of GV are still unknown, including the definitions of those parameters related to GV and their relationships with each other and with the patients’ prognosis. We describe the current situations related to GV in this review.
| Glycemic Variability | ▴Top |
GV can be evaluated according to various time frames such as short-term, intermediate-term, and long-term periods, although currently there is no clear definition of each. The oral glucose tolerance test (OGTT) that is used to diagnose diabetes can also evaluate the GV within a period of 2 h. This test could be considered to reveal short-term GV. However, in routine clinical practice, clinical data on GV are often reported according to the following: short-term GV, approximately 24 to 72 h (3 days) [11, 12]; intermediate-term GV, 3 days to 1 month, especially day-to-day variations [13-15]; and long-term GV, 1 month to several years, especially referring to HbA1c variations determined at routine clinic visits [16-18]. Furthermore, long-term GV includes seasonal variations [19-21]. Currently, there are few reports on long-term GV that is assessed for longer than 10 years. There is a wide range of indicators of GV based on various viewpoints even for short-term GV alone. In this article, we discuss indicators that are widely used in clinical practice and that have abundant supporting evidence.
| Short-Term Glycemic Variability | ▴Top |
Since the continuous glucose monitoring (CGM) system [9] has been popularized, its versatility in daily clinical practice has increased remarkably. Representative usages for the results are the standard deviation (SD) and coefficient of variation (CV) based on mean blood glucose levels measured continuously for 24 h and the mean amplitude of glycemic excursions (MAGE), which reflects postprandial blood glucose [22, 23]. Among these, a number of reports related to factors such as oxidative stress and inflammatory markers have been made for MAGE [24, 25]. In recent years, drugs in various categories have been developed. Although previously it was difficult to clarify at which point within a 24-h time frame the effects of such drugs were exerted, this information has become clear with the advent of the CGM system. This system allows greater ease in determining the effects of existing drugs and the effect of additional administration of other anti-diabetes drugs [26, 27]. Furthermore, detection of hypoglycemia related to CV events has become possible [10, 28, 29]. Specifically, in patients with impaired awareness of the presence of hypoglycemia, the CGM system can determine the frequency of nocturnal hypoglycemia, which was impossible otherwise [30]. In addition, the relationship between the clinical state, such as an improvement in insulin resistance and GV, has been gradually elucidated, although results are only based on a short-term effect. We also reported the negative correlation between short-term GV evaluated in a 24-h period and baroreflex sensitivity (BRS), which is a sensitive measure of cardiovascular autonomic neuropathy [31]. Above all, the CGM system is considered to be particularly useful from the viewpoint of comprehension of dietary habits and GV among individual patients. Presumably short-term GV may change significantly depending on dietary and exercise amounts. Therefore, in daily clinical practice the CGM is suitable for assessment of variability in individual patients, but it may not be well suited for determining the association with long-term prognosis when considering issues of reproducibility and maintenance of continuity. Strictly speaking, CGM measures glucose levels in interstitial tissues; thus there may be a potential for discrepancies between CGM measurements and blood glucose levels [32, 33]. Moreover, this examination is invasive, even though mildly. There is also some room for improvement in terms of cost effectiveness.
| Intermediate-Term Glycemic Variability | ▴Top |
Intermediate-term variability represented by day-to-day variability or the mean of daily difference (MODD) is difficult to evaluate, particularly in clinical practice. This is because, for example, people do not regularly ingest the same amount of food at the same time, especially those engaged in the modern life style. For that reason, there are few clinical reports on intermediate-term GV compared to short-term GV and long-term GV. However, patients with irregular dietary habits may be likely to have a large intermediate-term GV. A report by Xu et al on diabetic microangiopathy noted that in patients with large day-to-day dietary variations there was an association with diabetic neuropathy [34]. Niskanen et al reported that patients with large day-to-day GV during fasting are at high risk for hypoglycemia [35]. Moreover, there has been a report on the relationship between improvement in the day-to-day GV and oxidative stresses [15], which may imply a relationship between the intermediate-term GV and macro-angiopathy. The results from these reports suggest that the day-to-day GV, i.e., intermediate-term GV, may correlate with long-term GV to some extent. In addition, we have also routinely observed intermediate-term GV caused by differences in the duration of drug actions due to differences in half-life and other factors. We also reported such differences in our clinical trials using insulin [36]. Intermediate-term GV is also useful in determining the effects of the duration of action of medications and other factors.
| Long-Term Glycemic Variability | ▴Top |
Long-term GV is an index that has been frequently reported in recent years. This index can reflect changes in habits, with an orderly lifestyle reflected in slight GV. Long-term GV is often based on visit-to-visit GV in many cases. However, HbA1c in type 2 diabetic patients has often been shown to vary from season to season. In these reports, high values and low values are generally observed in winter and summer, respectively [19, 21, 37]. It has been reported that younger age, high body mass index, and amounts of dietary intake and exercise are involved in this seasonal phenomenon [16, 38]. Therefore, HbA1c evaluated on a visit-to-visit basis may be underestimated or overestimated depending on the timing of blood sampling. To evaluate the long-term GV more accurately, HbA1c should be assessed at the same time period and at the same frequency whenever possible. Moreover, it is desirable to compare HbA1c levels among patients whose clinical status matches to some extent, including the duration of disease.
In patients with large long-term GV, a variety of effects have been reported including involvement of micro-angiopathy such as an increase in CV events [17, 18, 39-42], onset of retinopathy [43], and onset of diabetic neuropathy [44]. Also noted have been vascular endothelial dysfunction [45] and healing time of foot ulcers [46]; development of chronic obstructive pulmonary disease (COPD) [47]; and development of Alzheimer’s disease (AD) [48]. However, many of these were retrospective studies, and there are many uncertainties as to what conditions those patients had and which factors caused the increased long-term GV. A growing number of studies have reported that long-term GV was increased in the elderly and patients using insulin [49].
Few studies have directly compared short-term GV and long-term GV. However, in a sub-analysis in the Diabetes Control and Complications study of type 1 diabetic patients it was demonstrated that visit-to-visit HbA1c variability and average blood glucose levels had the largest impacts on the HbA1c level, and daily blood sugar fluctuations (SD) also had some impact on HbA1c, but the effect was approximately 1/10 of the long-term HbA1c variation and 1/14 of the average blood glucose levels [50]. In addition, in our study, we investigated whether short-term GV evaluated by CGM or long-term GV evaluated by visit-to-visit HbA1c variability affected a decrease in BRS, which is also a marker of the onset of CV events. Results showed no significant difference, but there was a tendency for long-term GV to influence the decrease in BRS [51].
| Glycemic Variability and Prognosis of Type 2 Diabetes | ▴Top |
Increased GV has already been considered to be a risk factor for the development of CV events. There are few prospective trials comparing groups with large GV and small GV due to ethical concerns. It was reported that short-term GV was related to prolongation of hospital stays and prognosis of patients [52]; however, such studies are scarce. This may be because it is unknown whether the variation measured during a particular time period is maintained thereafter and because the continuation of increased blood glucose variations for a long period is rare since interventions are often implemented. To our knowledge, there has been no report on the day-to-day GV. In recent years, there has been an increasing number of reports on long-term GV [17, 18, 39, 42, 53-56], and a sub-analysis of the ADVANCE trial [52] reported that outpatient blood glucose variations and HbA1c variations are involved in diabetic complications and mortality rates. Summary of the possible explanations of the factors affecting the glycemic variability is illustrated in Figure 1. However, a method to measure long-term GV has not been established, and measurement frequencies vary from once to 12 times per year. Although many studies conducted those measurements once every 3 months, additional studies would be required to assess whether accurate fluctuations are observed because of seasonal fluctuations in HbA1c. In addition, that there are various factors involved in the GV is problematic, such as drug changes during the observation period, whose effects cannot be excluded in practice, making interpretation of the results difficult. Moreover, due to lack of a clear definition of long-term GV, the observation period in these studies on long-term GV varied considerably, ranging from 1 to 10 years, and most of the studies were from 2 to 3 years. Furthermore, when evaluating long-term GV, a longer observation period may not always be better for evaluation because the possibility of deterioration of the patient’s condition due to the disease progression and hospitalization may increase. In addition, differences in the contribution to the prognosis between long-term GV and the mean HbA1c value are still unknown, which also needs to be investigated.
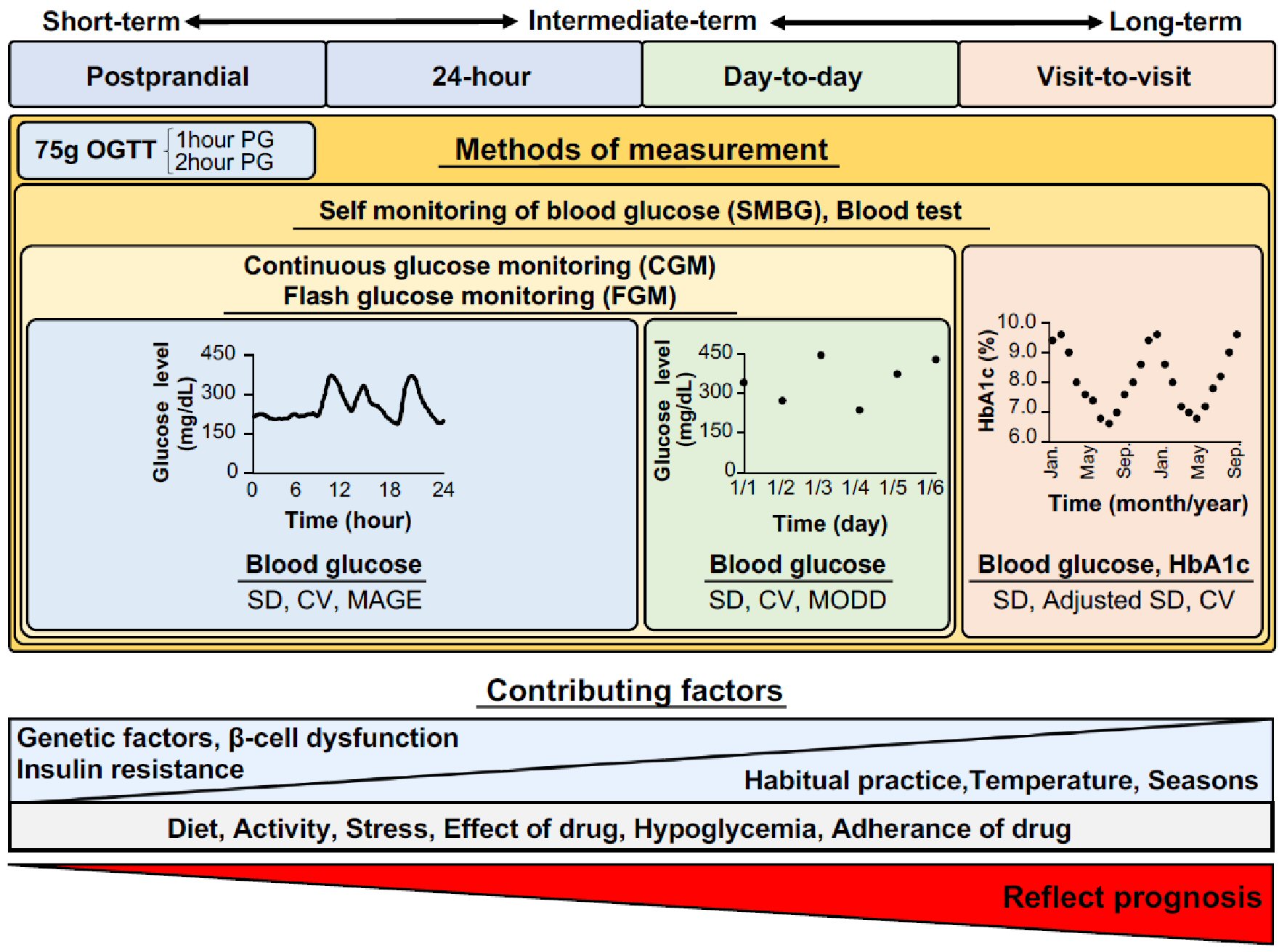 Click for large image | Figure 1. Factors affecting the glycemic variability. OGTT: oral glucose tolerance test; PG: plasma glucose; SD: standard deviation; CV: coefficient of variation; MAGE: mean amplitude of glucose excursion; MODD: mean of daily difference. |
| Conclusions | ▴Top |
Types of GV in terms of time frame vary from short-term to long-term. Several studies reported that long-term GV was related to micro- and macro-angiopathies in patients with type 2 diabetes mellitus (T2DM). However, there are still unknown aspects regarding the relationships of various durations of GV with prognosis. Further clinical trials are required that focus on the mechanism of GV and that evaluate whether GV can be a valuable therapeutic target for patients with T2DM.
Conflict of Interest
The authors of this manuscript have the following competing interests: M.S. has participated in speaker’s bureaus/advisory panels for Sanofi, Daiichi-Sankyo, Astellas, and Tanabe-Mitsubishi.
Abbreviations
GV: glycemic variability; CGM: continuous glucose monitoring; MAGE: mean amplitude of glycemic excursions; MODD: mean of daily difference; OGTT: oral glucose tolerance test; BRS: baroreflex sensitivity; T2DM: type 2 diabetes mellitus
| References | ▴Top |
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837-853.
doi - Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348(5):383-393.
doi pubmed - Action to Control Cardiovascular Risk in Diabetes Study G, Gerstein HC, Miller ME, Byington RP, Goff DC, Jr., Bigger JT, Buse JB, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545-2559.
doi pubmed - Advance Collaborative Group, Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560-2572.
doi pubmed - Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360(2):129-139.
doi pubmed - Desouza CV, Bolli GB, Fonseca V. Hypoglycemia, diabetes, and cardiovascular events. Diabetes Care. 2010;33(6):1389-1394.
doi pubmed - Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M, The STOP-NIDDM Trial Research Group. Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet. 2002;359(9323):2072-2077.
doi - Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M, The STOP-NIDDM Trial Research Group. Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA. 2003;290(4):486-494.
doi pubmed - Yogev Y, Ben-Haroush A, Chen R, Kaplan B, Phillip M, Hod M. Continuous glucose monitoring for treatment adjustment in diabetic pregnancies - a pilot study. Diabet Med. 2003;20(7):558-562.
doi pubmed - Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kroger J, Weitgasser R. Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet. 2016;388(10057):2254-2263.
doi - Rodbard D. New and improved methods to characterize glycemic variability using continuous glucose monitoring. Diabetes Technol Ther. 2009;11(9):551-565.
doi pubmed - Czerwoniuk D, Fendler W, Walenciak L, Mlynarski W. GlyCulator: a glycemic variability calculation tool for continuous glucose monitoring data. J Diabetes Sci Technol. 2011;5(2):447-451.
doi pubmed - Molnar GD, Taylor WF, Ho MM. Day-to-day variation of continuously monitored glycaemia: a further measure of diabetic instability. Diabetologia. 1972;8(5):342-348.
doi pubmed - Choleau C, Aubert C, Cahane M, Reach G. High day-to-day glucose variability: a frequent phenomenon in children and adolescents with type 1 diabetes attending summer camp. Diabetes Metab. 2008;34(1):46-51.
doi pubmed - Ohara M, Fukui T, Ouchi M, Watanabe K, Suzuki T, Yamamoto S, Yamamoto T, et al. Relationship between daily and day-to-day glycemic variability and increased oxidative stress in type 2 diabetes. Diabetes Res Clin Pract. 2016;122:62-70.
doi pubmed - Noyes JD, Soto-Pedre E, Donnelly LA, Pearson ER. Characteristics of people with high visit-to-visit glycaemic variability in Type 2 diabetes. Diabet Med. 2018;35(2):262-269.
doi pubmed - Prentice JC, Pizer SD, Conlin PR. Identifying the independent effect of HbA1c variability on adverse health outcomes in patients with Type 2 diabetes. Diabet Med. 2016;33(12):1640-1648.
doi pubmed - Cardoso CRL, Leite NC, Moram CBM, Salles GF. Long-term visit-to-visit glycemic variability as predictor of micro- and macrovascular complications in patients with type 2 diabetes: The Rio de Janeiro Type 2 Diabetes Cohort Study. Cardiovasc Diabetol. 2018;17(1):33.
doi pubmed - Sakura H, Tanaka Y, Iwamoto Y. Seasonal fluctuations of glycated hemoglobin levels in Japanese diabetic patients. Diabetes Res Clin Pract. 2010;88(1):65-70.
doi pubmed - Tseng CL, Brimacombe M, Xie M, Rajan M, Wang H, Kolassa J, Crystal S, et al. Seasonal patterns in monthly hemoglobin A1c values. Am J Epidemiol. 2005;161(6):565-574.
doi pubmed - Kim YJ, Park S, Yi W, Yu KS, Kim TH, Oh TJ, Choi J, et al. Seasonal variation in hemoglobin a1c in korean patients with type 2 diabetes mellitus. J Korean Med Sci. 2014;29(4):550-555.
doi pubmed - Kohnert KD, Vogt L, Augstein P, Heinke P, Zander E, Peterson K, Freyse EJ, et al. Relationships between glucose variability and conventional measures of glycemic control in continuously monitored patients with type 2 diabetes. Horm Metab Res. 2009;41(2):137-141.
doi pubmed - Zhou J, Jia W, Bao Y, Ma X, Lu W, Li H, Hu C, et al. Glycemic variability and its responses to intensive insulin treatment in newly diagnosed type 2 diabetes. Med Sci Monit. 2008;14(11):CR552-558.
pubmed - Ohara M, Nagaike H, Goto S, Fukase A, Tanabe Y, Tomoyasu M, Yamamoto T, et al. Improvements of ambient hyperglycemia and glycemic variability are associated with reduction in oxidative stress for patients with type 2 diabetes. Diabetes Res Clin Pract. 2018;139:253-261.
doi pubmed - Costantino S, Paneni F, Battista R, Castello L, Capretti G, Chiandotto S, Tanese L, et al. Impact of Glycemic Variability on Chromatin Remodeling, Oxidative Stress, and Endothelial Dysfunction in Patients With Type 2 Diabetes and With Target HbA1c Levels. Diabetes. 2017;66(9):2472-2482.
doi pubmed - Sakamoto M, Nishimura R, Irako T, Tsujino D, Ando K, Utsunomiya K. Comparison of vildagliptin twice daily vs. sitagliptin once daily using continuous glucose monitoring (CGM): crossover pilot study (J-VICTORIA study). Cardiovasc Diabetol. 2012;11:92.
doi pubmed - Matsumura M, Nakatani Y, Tanka S, Aoki C, Sagara M, Yanagi K, Suzuki K, et al. Efficacy of additional canagliflozin administration to type 2 diabetes patients receiving insulin therapy: examination of diurnal glycemic patterns using Continuous Glucose Monitoring (CGM). Diabetes Ther. 2017;8(4):821-827.
doi pubmed - Haak T, Hanaire H, Ajjan R, Hermanns N, Riveline JP, Rayman G. Flash glucose-sensing technology as a replacement for blood glucose monitoring for the management of insulin-treated type 2 diabetes: a multicenter, open-label randomized controlled trial. Diabetes Ther. 2017;8(1):55-73.
doi pubmed - Kaufman FR, Gibson LC, Halvorson M, Carpenter S, Fisher LK, Pitukcheewanont P. A pilot study of the continuous glucose monitoring system: clinical decisions and glycemic control after its use in pediatric type 1 diabetic subjects. Diabetes Care. 2001;24(12):2030-2034.
doi pubmed - Gehlaut RR, Dogbey GY, Schwartz FL, Marling CR, Shubrook JH. Hypoglycemia in type 2 diabetes - more common than you think: a continuous glucose monitoring study. J Diabetes Sci Technol. 2015;9(5):999-1005.
doi pubmed - Matsutani D, Sakamoto M, Iuchi H, Minato S, Suzuki H, Kayama Y, Takeda N, et al. Glycemic variability in continuous glucose monitoring is inversely associated with baroreflex sensitivity in type 2 diabetes: a preliminary report. Cardiovasc Diabetol. 2018;17(1):36.
doi pubmed - Boyne MS, Silver DM, Kaplan J, Saudek CD. Timing of changes in interstitial and venous blood glucose measured with a continuous subcutaneous glucose sensor. Diabetes. 2003;52(11):2790-2794.
doi pubmed - Aberer F, Hajnsek M, Rumpler M, Zenz S, Baumann PM, Elsayed H, Puffing A, et al. Evaluation of subcutaneous glucose monitoring systems under routine environmental conditions in patients with type 1 diabetes. Diabetes Obes Metab. 2017;19(7):1051-1055.
doi pubmed - Xu F, Zhao LH, Su JB, Chen T, Wang XQ, Chen JF, Wu G, et al. The relationship between glycemic variability and diabetic peripheral neuropathy in type 2 diabetes with well-controlled HbA1c. Diabetol Metab Syndr. 2014;6(1):139.
doi pubmed - Niskanen L, Virkamaki A, Hansen JB, Saukkonen T. Fasting plasma glucose variability as a marker of nocturnal hypoglycemia in diabetes: evidence from the PREDICTIVE study. Diabetes Res Clin Pract. 2009;86(2):e15-18.
doi pubmed - Iuchi H, Sakamoto M, Matsutani D, Suzuki H, Horiuchi R, Utsunomiya K. The durability of basal insulin affects day-to-day glycemic variability assessed by continuous glucose monitoring in type 2 diabetes patients: a randomized crossover trial. Diabetes Technol Ther. 2017;19(8):457-462.
doi pubmed - Maguire GA, Edwards OM. Seasonal variation in glycated haemoglobin in diabetics. Ann Clin Biochem. 2001;38(Pt 1):59-60.
doi pubmed - Berglund L, Berne C, Svardsudd K, Garmo H, Melhus H, Zethelius B. Seasonal variations of insulin sensitivity from a euglycemic insulin clamp in elderly men. Ups J Med Sci. 2012;117(1):35-40.
doi pubmed - Gorst C, Kwok CS, Aslam S, Buchan I, Kontopantelis E, Myint PK, Heatlie G, et al. Long-term Glycemic Variability and Risk of Adverse Outcomes: A Systematic Review and Meta-analysis. Diabetes Care. 2015;38(12):2354-2369.
doi pubmed - Hirakawa Y, Arima H, Zoungas S, Ninomiya T, Cooper M, Hamet P, Mancia G, et al. Impact of visit-to-visit glycemic variability on the risks of macrovascular and microvascular events and all-cause mortality in type 2 diabetes: the ADVANCE trial. Diabetes Care. 2014;37(8):2359-2365.
doi pubmed - Lin CC, Yang CP, Li CI, Liu CS, Chen CC, Lin WY, Hwang KL, et al. Visit-to-visit variability of fasting plasma glucose as predictor of ischemic stroke: competing risk analysis in a national cohort of Taiwan Diabetes Study. BMC Med. 2014;12:165.
doi pubmed - Laiteerapong N, Karter AJ, Moffet HH, Cooper JM, Gibbons RD, Liu JY, Gao Y, et al. Ten-year hemoglobin A1c trajectories and outcomes in type 2 diabetes mellitus: The Diabetes & Aging Study. J Diabetes Complications. 2017;31(1):94-100.
doi pubmed - Hietala K, Waden J, Forsblom C, Harjutsalo V, Kyto J, Summanen P, Groop PH, et al. HbA1c variability is associated with an increased risk of retinopathy requiring laser treatment in type 1 diabetes. Diabetologia. 2013;56(4):737-745.
doi pubmed - Virk SA, Donaghue KC, Cho YH, Benitez-Aguirre P, Hing S, Pryke A, Chan A, et al. Association between HbA1c variability and risk of microvascular complications in adolescents with type 1 diabetes. J Clin Endocrinol Metab. 2016;101(9):3257-3263.
doi pubmed - Wei F, Sun X, Zhao Y, Zhang H, Diao Y, Liu Z. Excessive visit-to-visit glycemic variability independently deteriorates the progression of endothelial and renal dysfunction in patients with type 2 diabetes mellitus. BMC Nephrol. 2016;17(1):67.
doi pubmed - Dhatariya KK, Li Ping Wah-Pun Sin E, Cheng JOS, Li FYN, Yue AWY, Gooday C, Nunney I. The impact of glycaemic variability on wound healing in the diabetic foot - A retrospective study of new ulcers presenting to a specialist multidisciplinary foot clinic. Diabetes Res Clin Pract. 2018;135:23-29.
doi pubmed - Chiu HT, Li TC, Li CI, Liu CS, Lin WY, Lin CC. Visit-to-visit glycemic variability is a strong predictor of chronic obstructive pulmonary disease in patients with type 2 diabetes mellitus: Competing risk analysis using a national cohort from the Taiwan diabetes study. PLoS One. 2017;12(5):e0177184.
doi pubmed - Li TC, Yang CP, Tseng ST, Li CI, Liu CS, Lin WY, Hwang KL, et al. Visit-to-visit variations in fasting plasma glucose and HbA1c associated with an increased risk of Alzheimer disease: Taiwan diabetes study. Diabetes Care. 2017;40(9):1210-1217.
doi pubmed - Ryu OH, Lee S, Yoo HJ, Choi MG. Seasonal variations in glycemic control of type 2 diabetes in Korean women. J Endocrinol Invest. 2014;37(6):575-581.
doi pubmed - McCarter RJ, Hempe JM, Chalew SA. Mean blood glucose and biological variation have greater influence on HbA1c levels than glucose instability: an analysis of data from the Diabetes Control and Complications Trial. Diabetes Care. 2006;29(2):352-355.
doi pubmed - Matsutani D, Sakamoto M, Minato S, Kayama Y, Takeda N, Horiuchi R, Utsunomiya K. Visit-to-visit HbA1c variability is inversely related to baroreflex sensitivity independently of HbA1c value in type 2 diabetes. Cardiovasc Diabetol. 2018;17(1):100.
doi pubmed - Mendez CE, Mok KT, Ata A, Tanenberg RJ, Calles-Escandon J, Umpierrez GE. Increased glycemic variability is independently associated with length of stay and mortality in noncritically ill hospitalized patients. Diabetes Care. 2013;36(12):4091-4097.
doi pubmed - Muggeo M, Zoppini G, Bonora E, Brun E, Bonadonna RC, Moghetti P, Verlato G. Fasting plasma glucose variability predicts 10-year survival of type 2 diabetic patients: the Verona Diabetes Study. Diabetes Care. 2000;23(1):45-50.
doi pubmed - Bonke FC, Donnachie E, Schneider A, Mehring M. Association of the average rate of change in HbA1c with severe adverse events: a longitudinal evaluation of audit data from the Bavarian Disease Management Program for patients with type 2 diabetes mellitus. Diabetologia. 2016;59(2):286-293.
doi pubmed - Wan EY, Fung CS, Fong DY, Lam CL. Association of variability in hemoglobin A1c with cardiovascular diseases and mortality in Chinese patients with type 2 diabetes mellitus - A retrospective population-based cohort study. J Diabetes Complications. 2016;30(7):1240-1247.
doi pubmed - Su JB, Yang XH, Zhang XL, Cai HL, Huang HY, Zhao LH, Xu F, et al. The association of long-term glycaemic variability versus sustained chronic hyperglycaemia with heart rate-corrected QT interval in patients with type 2 diabetes. PLoS One. 2017;12(8):e0183055.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.











