| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 15, Number 6, June 2023, pages 292-299
Outcomes of Telestroke Inter-Hospital Transfers Among Intervention and Non-Intervention Patients
Adalia H. Jun-O’Connella, c, Shravan Sivakumara, Nils Henningera, Brian Silvera, Meghna Trivedib, Mehdi Ghasemia, Rakhee R. Lallaa, Kimiyoshi J. Kobayashib
aDepartment of Neurology, University of Massachusetts Chan Medical School, Worcester, MA 01655, USA
bDepartment of Medicine, University of Massachusetts Chan Medical School, Worcester, MA 01655, USA
cCorresponding Author: Adalia H. Jun-O’Connell, Department of Neurology, University of Massachusetts Chan Medical School, Worcester, MA 01655, USA
Manuscript submitted May 11, 2023, accepted June 10, 2023, published online June 29, 2023
Short title: Telestroke Transfers and Outcome
doi: https://doi.org/10.14740/jocmr4945
| Abstract | ▴Top |
Background: Telestroke is an established telemedicine method of delivering emergency stroke care. However, not all neurological patients utilizing telestroke service require emergency interventions or transfer to a comprehensive stroke center. To develop an understanding of the appropriateness of inter-hospital neurological transfers utilizing the telemedicine, our study aimed to assess the differences in outcomes of inter-hospital transfers utilizing the service in relation to the need for neurological interventions.
Methods: The pragmatic, retrospective analysis included 181 consecutive patients, who were emergently transferred from telestroke-affiliated regional medical centers between October 3, 2021, and May 3, 2022. In this exploratory study investigating the outcomes of telestroke-referred patients, patients receiving interventions were compared to those that did not following transfer to our tertiary center. Neurological interventions included mechanical thrombectomy (MT) and/or tissue plasminogen activator (tPA), craniectomy, electroencephalography (EEG), or external ventricular drain (EVD). Transfer mortality rate, discharge functional status defined by modified Rankin scale (mRS), neurological status defined by National Institutes of Health Stroke Scale (NIHSS), 30-day unpreventable readmission rate, 90-day clinical major adverse cardiovascular events (MACE), and 90-day mRS, and NIHSS were studied. We used χ2 or Fisher exact tests to evaluate the association between the intervention and categorical or dichotomous variables. Continuous or ordinal measures were compared using Wilcoxon rank-sum tests. All tests of statistical significance were considered to be significant at P < 0.05.
Results: Among the 181 transferred patients, 114 (63%) received neuro-intervention and 67 (37%) did not. The death rate during the index admission was not statistically significant between the intervention and non-intervention groups (P = 0.196). The discharge NIHSS and mRS were worse in the intervention compared to the non-intervention (P < 0.05 each, respectively). The 90-day mortality and cardiovascular event rates were similar between intervention and non-intervention groups (P > 0.05 each, respectively). The 30-day readmission rates were also similar between the two groups (14% intervention vs. 13.4% non-intervention, P = 0.910). The 90-day mRS were not significantly different between intervention and non-intervention groups (median 3 (IQR: 1 - 6) vs. 2 (IQR: 0 - 6), P = 0.109). However, 90-day NIHSS was worse in the intervention compared to non-intervention group (median 2 (IQR: 0 - 11) vs. 0 (IQR: 0 - 3), P = 0.004).
Conclusions: Telestroke is a valuable resource that expedites emergent neurological care via referral to a stroke center. However, not all transferred patients benefit from the transfer process. Future multicenter studies are warranted to study the effects or appropriateness of telestroke networks, and to better understand the patient characteristics, resources allocation, and transferring institutions to improve telestroke care.
Keywords: Telestroke; Thrombectomy; Thrombolytic therapy; Quality improvement; Outcomes
| Introduction | ▴Top |
Telestroke is an established method of delivering emergency stroke care within stroke systems of care [1]. Telestroke services play a critical role in the delivery of timely reperfusion therapies, intravenous tissue plasminogen activator (tPA) and mechanical thrombectomy (MT) by early identification of stroke symptoms and facilitation of transfer to a tertiary-care center when deemed necessary [2-5]. In addition, it can be used to effectively trigger multidisciplinary care team activations at the receiving hospital [6]. Telestroke has several advantages, including increased rates of utilization of tPA, better accessibility in geographically underserved locations, and decreased inequities in acute stroke care [7]. Accuracy of stroke diagnosis and improved time-based stroke treatment metrics have been established with implementation of telestroke programs [8].
In parallel, there has been an increase in inter-hospital transfer rates of neurological patients [9]. It is important to note that telestroke services are increasingly used for non-tPA and non-thrombectomy neurological cases [10]. This is important as telestroke services are now viewed as emergent neurological triaging or emergent teleneurology support to facilitate transfers to tertiary centers for intensive care unit (ICU) care and additional diagnostic workup [5]. However, not all patients who are transferred to tertiary centers receive additional emergency interventions or other higher complexity care [11]. This raises the question of whether some proportions of transfers are futile.
Futile transfers can increase health care costs and produce capacity issues in tertiary centers [12, 13]. Futile inter-hospital transfers have been described in ischemic strokes and MT, in which 45% of transferred patients did not require thrombectomy due to clinical improvement, delay in transfer time, or increase in infarct volume [14]. However, the factors and outcomes associated with futile transfers among more general emergent neurologic transfers have not been well-defined through telestroke program. The 90-day clinical outcomes are also unknown for those patients emergently transferred but who do not require acute interventions.
Our study is an exploratory study investigating the outcomes between two groups of neurological patients that received neurological interventions and those who did not among patients who were transferred through telestroke services. Neurological interventions included MT and/or tPA, craniectomy, electroencephalography (EEG) or external ventricular drain (EVD). Our primary outcome of interest was mortality rate during the index admission following the transfer, discharge functional status defined by modified Rankin scale (mRS) and neurological status defined by National Institutes of Health Stroke Scale (NIHSS). Our secondary outcomes of interests were 30-day unpreventable readmission rate, 90-day major adverse cardiovascular events (MACEs) of death and cardiovascular events, and 90-day functional status and neurological status.
| Materials and Methods | ▴Top |
Study cohort
The study was approved by the Institutional Review Board at UMass Chan Medical School, and the Health Insurance Portability and Accountability Act (HIPPA) waiver of informed consent was granted. We prepared our manuscript according to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines [15]. We retrospectively studied consecutive adult patients (greater than age 18 years) transferred to the University of Massachusetts Memorial Medical Center (UMMMC) in Worcester, Massachusetts, from telestroke-affiliated regional medical centers between October 3, 2021, and May 3, 2022, due to an acute neurological diagnosis. This study was conducted in compliance with the ethical standards of the responsible institutional human subjects as well as with the Helsinki Declaration.
Telestroke consultation was defined as a consultation utilizing audiovisual communication systems addressing the treatment of stroke as well as identifying common stroke mimics and offering recommendations [5]. Transfer decisions were determined by physicians involved in the initial patient care. The standard process for the transfer was that treating physicians reach out to the telestroke physician at the medical center. The accepting physician accepted the patient for transfer if patients were deemed to require services offered at the tertiary medical center, including neuro-intensive level of care, specialized consultations not available through telemedicine (e.g., neurosurgery), or potential need for surgeries or interventions not offered by the referring hospital. We excluded patients who were not transferred for an acute neurological issue. The study population was split into two groups for the purpose of our analyses: 1) patients that had neurological interventions including MT and/or tPA, craniectomy, EEG, or EVD; 2) those patients that did not receive any of these interventions.
Data collection
All diagnoses were first established by the treating board-certified neurologist and confirmed by an abstracting physician (SS). Medical records of the included patients (n = 181) were reviewed. Conflicting diagnoses were resolved by consensus after adjudication by a board-certified vascular neurologist (AJO).
Baseline patient characteristics included gender, age, underlying neurological diagnosis, comorbidities, length of stay (LOS), and pertinent stroke prevention medication lists. Reasons for transfer were also studied. Clinical severity of illness was determined through use of NIHSS at presentation, and the presenting functional status was defined by pre-admission mRS. If the NIHSS was not documented, an NIHSS was constructed using a standard, validated process based on the initial physical examination [16]. Code status, discharge NIHSS and discharge mRS were also obtained.
Outcomes
Our primary outcome of interest was mortality during the index admission, discharge functional status defined by mRS and neurological status defined by NIHSS. Our secondary outcomes were 30-day unpreventable readmission rate, 90-day MACEs of death and cardiovascular events, and 90-day functional status and neurological status.
Statistical analysis
Descriptive statistics of demographic/clinical characteristics associated with transfer status were generated using contingency tables. Frequencies and proportions were reported for categorical/dichotomous variables, and interquartile range (25th, 75th) are reportedly for ordinal measures. We used χ2 or Fisher exact tests to evaluate the association between the intervention and categorical or dichotomous variables. Continuous or ordinal measures were compared using Wilcoxon rank-sum tests. All tests of statistical significance were two-tailed and considered to be significant at P < 0.05. All statistical analyses were performed using SAS 9.4 software.
| Results | ▴Top |
Study participants, prevalence of telestroke transfer, and clinical characteristics
Figure 1 describes the study flow. Of 1,935 telestroke consultations during the study period, there were 181 (9.4%) neurological transfers. One hundred thirteen (62%) of the transferred patients had stroke as their final diagnosis. Among transferred patients, 114 (63%) received neuro-intervention and 67 (37%) did not. Table 1 describes the demographic and patient characteristics of the two groups.
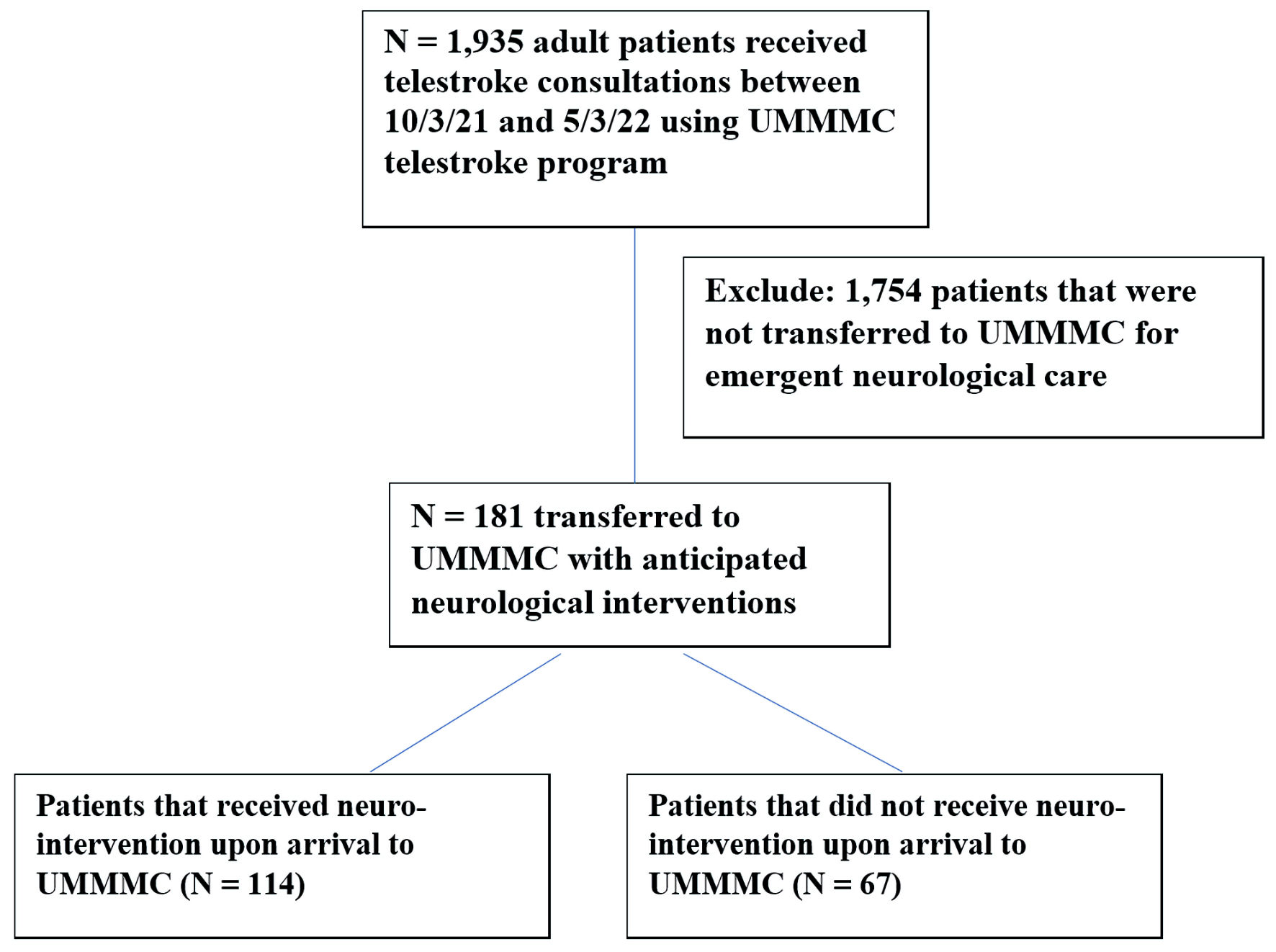 Click for large image | Figure 1. Patient flow. UMMMC: University of Massachusetts Memorial Medical Center. |
 Click to view | Table 1. Demographic and Characteristic Information of Patients With and Without Intervention |
Overall, patient characteristics were similar between the groups (P > 0.05) except for higher acuity of care (P < 0.001), more ischemic stroke (P = 0.003), less non-stroke neurological diagnosis (P = 0.002), more frequent tPA usage and thrombectomy (P < 0.05, each), more frequent craniectomy, EVD, and EEG utilizations (P < 0.05, each), more hypertension (P = 0.031) and atrial fibrillation (P = 0.040) in the intervention versus non-intervention group.
Compared to the non-intervention group, the intervention group also had higher presenting NIHSS (median 11 (IQR: 3 - 22) vs. 1 (IQR: 0 - 3), P < 0.001). Furthermore, only a small number of patients (2.8%) utilizing telestroke service had documented clear goals of care prior to the transfer.
Immediate outcomes of mortality, LOS, discharge functional status and neurological status
Table 2 describes mortality rate, LOS, discharge functional status, and discharge neurological status stratified by the intervention status. Overall, mortality was not significantly different between intervention and non-intervention groups (17.5% vs. 10.4%, P = 0.196). However, the intervention group had worse discharge NIHSS (median 4 (IQR: 1 - 14) vs. 0 (IQR: 0 - 3), P < 0.001), worse discharge mRS (median 4 (IQR: 2 - 4) vs. 2 (IQR: 1 - 4), P = 0.001), and a longer median LOS (median 6 (IQR: 3 - 10) vs. 3 (IQR: 1 - 5), P < 0.001) compared to the non-intervention group.
 Click to view | Table 2. Immediate Outcomes of Mortality, LOS, Discharge Functional Status, and Neurological Status Following the Inter-Hospital Transfer |
30-day readmission rate and 90-day outcome events
The 30-day readmission rate and 90-day MACEs were shown on Table 3. The 30-day readmission rates were also similar between the two groups (14% intervention vs. 13.4% non-intervention, P = 0.910). The overall 90-day mortality was 22% (40/181), and the 30-day readmissions rate was 14% (25/181) for transferred patients. The 90-day mortality and cardiovascular event rates were similar between intervention and non-intervention groups (23% vs. 21%, P = 0.765; 3.5% vs. 4.5%, P = 0.711, respectively).
 Click to view | Table 3. Thirty-Day Readmission Rate and 90-Day Outcome Events Following the Inter-Hospital Transfer |
The 90-day mRS were similar between intervention and non-intervention groups (median 3 (IQR: 1 - 6) vs. 2 (IQR: 0 - 6), P = 0.109). However, 90-day NIHSS was worse in the intervention compared to non-intervention group (median 2 (IQR: 0 - 11) vs. 0 (IQR: 0 - 3), P = 0.004).
| Discussion | ▴Top |
From our study, we observed that transfers requiring emergent neuro-interventions demonstrated higher patient complexity (as reflected by higher NIHSS), longer LOS, and higher ICU utilization compared to the transfers that did not receive intervention. However, we also observed that the non-intervention group was more likely to have a non-stroke neurological diagnosis and less likely to require ICU level of care. It is also important to note that there was no significant difference between the two groups in terms of neurosurgery consultation utilization. Among the entire study cohort, utilization of palliative care consult was low in the context of the observed mortality rate. In addition, the frequency of documented goals of care prior to the transfer was low. Taken together, these findings suggest multiple opportunities for quality improvement such as exploration of tele-neurosurgery consultation, clarification of goals of care prior to transfer, and greater use of palliative care after transfer. All of these interventions may reduce the need for transfer to a tertiary care center. Avoiding unnecessary transfers would likely enhance the patient and family experience at the end of life by avoiding a sense of false optimism as well as the disruptions associated with moving a patient out of a medical facility closer to their home.
The intervention group had worse discharge mRS and NIHSS, which likely reflect the complexities of the intervention group. However, we observed that there were no significant differences in 90-day mortality and 90-day functional status between the intervention and non-intervention groups.
Our findings are a step towards understanding patient characteristics associated with patient transfers, given the recent trend in increasing transfer rates following tele-neurology consultations [9]. Certainly, patient transfers that require necessary services (for example, an obstructive hemorrhagic stroke requiring EVD) that cannot be provided in resource-limited primary medical centers are considered appropriate transfers. However, the value is less clear for those transfers that do not require neuro-intervention, particularly in a setting where tertiary care resources are increasingly limited. In the United States, futile transfers that lead to an inpatient mortality are known to impact publicly reported mortality figures, which can have a reputational and financial impact on tertiary care centers [17]. This creates a challenge for healthcare system, in which patients’ quality care and right to receive the best chance at survival need to be balanced with a timely recognition for potential non-futile care, especially in the post coronavirus disease 2019 (COVID-19) capacity challenges. Further studies are warranted to better understand outcomes among neurological patients that utilize telestroke programs. A recent study observed that telestroke programs not only improve treatment in acute stroke, but also potentially improve the efficiency of inter-hospital networks through disposition optimization and the avoidance of unnecessary transfers [18]. Future studies are warranted to develop understanding of patient characteristics that may not require potential futile transfers.
The prevalence of hemorrhagic stroke was similar between the intervention and non-intervention groups in our study. It is well known that there are not many medical options to manage non-vascular hemorrhagic strokes, aside from blood pressure control, neurological assessments to assess for deterioration, and reversal of anticoagulation in pertinent cases [19]. Therefore, clearer guidelines regarding appropriate criteria for hemorrhagic stroke transfers in non-intervention cases, such as non-aneurysmal lobar intracerebral hemorrhages (ICH), may be of benefit. The ongoing FASTEST ICH trial focuses on ICH hematoma reduction by swift introduction of factor VIIa within 2 h of hemorrhagic stroke symptom onset [20]. Novel interventions such as this may be hampered by delays in access to the study drug given limited access to academic medical centers.
The frequency of neurosurgery consultation was similar between the intervention and non-intervention groups in our study. This highlights the issue of limited access to neurosurgical consultations in regional medical centers. The feasibility of telemedicine in neurosurgery has been well described [21] and should be considered in future implementation towards comprehensive telestroke services. We also noted the frequency of neurosurgical interventions of craniectomy and/or EVD were low in our study even after patients were transferred to a tertiary care center. Creation of telemedicine consultation services for neurosurgery could avoid unnecessary transfers, similar to how telemedicine access in neurology has already been shown to avoid unnecessary transfers [18]. Finally, most telestroke transfers meet ICU level of care due to the severity of their neurological presentation which likely contributed to the need for an inter-hospital transfer. Another way to potentially solve this problem without transferring the patient is to augment ICU capabilities within regional medical centers with telemedicine services.
Our study also highlights the need to define clear goals of care prior to transferring patients. Our chart reviews indicated that only a small number of patients (2.8%) utilizing telestroke services had documented goals of care prior to the transfer. About 10% (18/181) of transferred patients changed their code status to comfort measure only status after the transfer. The low utilization of hospice services is an opportunity both for families of deceased patients who could utilize bereavement services that come with the hospice, as well as for hospitals that are held accountable for inpatient mortality performance [22, 23]. Establishment of clear goals of care is an important initiative that requires attention as disabling acute conditions, such as devastating stroke with severe deficits, are viewed as an unacceptable quality of life, worse than death [24, 25]. There is a movement towards establishing clear goals of care documentation within 48 h of admission in safety-net medical centers to align patients’ values and goals in their medical care [26]. This is particularly important for stroke patients given the high mortality and morbidity. Having this information prior to the transfer is critical to quantifying potential risks and benefits of transferring patients between hospitals. This also leads to an important question regarding how to increase palliative care involvement in stroke patients as it is known to reduce symptom burden, LOS, and improve survival after stroke [27].
The strengths of our study included the independent reassessment of the clinical diagnoses by a trained vascular neurologist and chart reviews of all cases, with further adjudication of uncertain cases by a second neurologist and resolution of the cases by group consensus. A major limitation of the study is its relatively small sample size. Furthermore, since this was a descriptive study, outcomes were not adjusted for confounders. Thus, the results need to be interpreted with caution. Other limitations of the study are its single center and retrospective design which all may have led to bias. As the intervention decisions are finalized upon the patient’s arrival at the tertiary medical center based upon the neurological assessments, there may be an introduction of bias. Furthermore, since the study was a pragmatic retrospective exploratory study comparing the outcomes of telestroke referred patients, there may be an introduction of bias when drawing direct conclusions. Although it is a single tertiary care center study, it had a well-developed telestroke program, consisting of connections with regional affiliated hospitals, which raises the importance of pragmatism in regions that require urgent neurology consultation access.
Conclusions
Telestroke is a valuable resource that expedites emergent neurological care via referral to a stroke center. However, not all patients who are transferred benefit from transfer. Future multicenter studies are warranted to study the effects or appropriateness of telestroke networks and to better understand the patient characteristics, resources allocation, and transferring institutions to improve telestroke care.
Acknowledgments
We would like to thank Joanne Petmezis, Laurieann Grenier, and Daksha Gopal for their help.
Financial Disclosure
The research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
Adalia H. Jun-O’Connell receives compensation for adjudication of stroke outcomes in the Women’s Health Initiative (WHI). Nils Henninger is supported by W81XWH-19-PRARP-RPA from the Department of Defense Congressionally Directed Medical Research Programs (CDMRP). Brian Silver receives compensation for review of medicolegal malpractice cases, for adjudication of stroke outcomes in the Women’s Health Initiative, and authorship for Ebix Medlink, Medscape. Rakhee Lalla receives compensation for adjudication of stroke outcomes in the Women’s Health Initiative (WHI). Shravan Sivakumar, Meghna Trivedi, Mehdi Ghasemi, and Kimiyoshi J. Kobayashi have no conflict of interest to declare.
Informed Consent
Informed consent was waived due to the retrospective nature of the study and was reviewed and approved by IRB.
Author Contributions
Adalia H. Jun-O’Connell: study concept and design, data acquisition, interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content. Shravan Sivakumar: data acquisition, interpretation of data, and critical revision of the manuscript for important intellectual content. Nils Henninger: interpretation of data and critical revision of the manuscript for important intellectual content. Brian Silver: interpretation of data and critical revision of the manuscript for important intellectual content. Meghna Trivedi: study concept, interpretation of data, and critical revision of the manuscript for important intellectual content. Mehdi Ghasemi: interpretation of data and critical revision of the manuscript for important intellectual content. Rakhee R. Lalla: interpretation of data and critical revision of the manuscript for important intellectual content. Kimiyoshi J. Kobayashi: study concept and design, interpretation of data, and critical revision of the manuscript for important intellectual content.
Data Availability
The investigators will share anonymized data (with associated coding library) used in developing the results presented in this manuscript upon reasonable request to investigators who have received ethical clearance from their host institution.
| References | ▴Top |
- Schwamm LH, Holloway RG, Amarenco P, Audebert HJ, Bakas T, Chumbler NR, Handschu R, et al. A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2009;40(7):2616-2634.
doi pubmed - Jauch EC, Schwamm LH, Panagos PD, Barbazzeni J, Dickson R, Dunne R, Foley J, et al. Recommendations for regional stroke destination plans in rural, suburban, and urban communities from the prehospital stroke system of care consensus conference: a consensus statement from the American Academy of Neurology, American Heart Association/American Stroke Association, American Society of Neuroradiology, National Association of EMS Physicians, National Association of State EMS Officials, Society of NeuroInterventional Surgery, and Society of Vascular and Interventional Neurology: Endorsed by the Neurocritical Care Society. Stroke. 2021;52(5):e133-e152.
doi pubmed - LaMonte MP, Xiao Y, Hu PF, Gagliano DM, Bahouth MN, Gunawardane RD, MacKenzie CF, et al. Shortening time to stroke treatment using ambulance telemedicine: TeleBAT. J Stroke Cerebrovasc Dis. 2004;13(4):148-154.
doi pubmed - Nguyen-Huynh MN, Klingman JG, Avins AL, Rao VA, Eaton A, Bhopale S, Kim AC, et al. Novel telestroke program improves thrombolysis for acute stroke across 21 hospitals of an integrated healthcare system. Stroke. 2018;49(1):133-139.
doi pubmed pmc - Demaerschalk BM, Berg J, Chong BW, Gross H, Nystrom K, Adeoye O, Schwamm L, et al. American Telemedicine Association: telestroke guidelines. Telemed J E Health. 2017;23(5):376-389.
doi pubmed pmc - Dorsey ER, Glidden AM, Holloway MR, Birbeck GL, Schwamm LH. Teleneurology and mobile technologies: the future of neurological care. Nat Rev Neurol. 2018;14(5):285-297.
doi pubmed - Wechsler LR, Demaerschalk BM, Schwamm LH, Adeoye OM, Audebert HJ, Fanale CV, Hess DC, et al. Telemedicine quality and outcomes in stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017;48(1):e3-e25.
doi pubmed - Tumma A, Berzou S, Jaques K, Shah D, Smith AC, Thomas EE. Considerations for the implementation of a telestroke network: a systematic review. J Stroke Cerebrovasc Dis. 2022;31(1):106171.
doi pubmed - Zachrison KS, Onnela JP, Hernandez A, Reeves MJ, Camargo CA, Jr., Cox M, Matsouaka RA, et al. Ischemic stroke transfer patterns in the Northeast United States. J Stroke Cerebrovasc Dis. 2019;28(2):295-304.
doi pubmed - Handschu R, Wacker A, Scibor M, Sancu C, Schwab S, Erbguth F, Oschmann P, et al. Use of a telestroke service for evaluation of non-stroke neurological cases. J Neurol. 2015;262(5):1266-1270.
doi pubmed - De Los Rios La Rosa F. Connecting telestroke with transfers: do we have a clear picture? Neurology. 2022;98(16):651-652.
doi pubmed - Fuentes B, Alonso de Lecinana M, Ximenez-Carrillo A, Martinez-Sanchez P, Cruz-Culebras A, Zapata-Wainberg G, Ruiz-Ares G, et al. Futile interhospital transfer for endovascular treatment in acute ischemic stroke: the madrid stroke network experience. Stroke. 2015;46(8):2156-2161.
doi pubmed - Sonig A, Lin N, Krishna C, Natarajan SK, Mokin M, Hopkins LN, Snyder KV, et al. Impact of transfer status on hospitalization cost and discharge disposition for acute ischemic stroke across the US. J Neurosurg. 2016;124(5):1228-1237.
doi pubmed - Sablot D, Dumitrana A, Leibinger F, Khlifa K, Fadat B, Farouil G, Allou T, et al. Futile inter-hospital transfer for mechanical thrombectomy in a semi-rural context: analysis of a 6-year prospective registry. J Neurointerv Surg. 2019;11(6):539-544.
doi pubmed - http://www.strobe-statement.org.
- Williams LS, Yilmaz EY, Lopez-Yunez AM. Retrospective assessment of initial stroke severity with the NIH Stroke Scale. Stroke. 2000;31(4):858-862.
doi pubmed - Brooten JK, Buckenheimer AS, Hallmark JK, Grey CR, Cline DM, Breznau CJ, McQueen TS, et al. Risky behavior: hospital transfers associated with early mortality and rates of goals of care discussions. West J Emerg Med. 2020;21(4):935-942.
doi pubmed pmc - Lyerly MJ, Daggy J, LaPradd M, Martin H, Edwards B, Graham G, Martini S, et al. Impact of telestroke implementation on emergency department transfer rate. Neurology. 2022;98(16):e1617-e1625.
doi pubmed - Broderick JP, Grotta JC, Naidech AM, Steiner T, Sprigg N, Toyoda K, Dowlatshahi D, et al. The story of intracerebral hemorrhage: from recalcitrant to treatable disease. Stroke. 2021;52(5):1905-1914.
doi pubmed pmc - Naidech AM, Grotta J, Elm J, Janis S, Dowlatshahi D, Toyoda K, Steiner T, et al. Recombinant factor VIIa for hemorrhagic stroke treatment at earliest possible time (FASTEST): Protocol for a phase III, double-blind, randomized, placebo-controlled trial. Int J Stroke. 2022;17(7):806-809.
doi pubmed pmc - Eichberg DG, Basil GW, Di L, Shah AH, Luther EM, Lu VM, Perez-Dickens M, et al. Telemedicine in neurosurgery: lessons learned from a systematic review of the literature for the COVID-19 era and beyond. Neurosurgery. 2020;88(1):E1-E12.
doi pubmed pmc - Schorr CA, Angelo M, John G, LeCompte K, Dellinger RP. The association of increasing hospice use with decreasing hospital mortality: an analysis of the national inpatient sample. J Healthc Manag. 2020;65(2):107-120.
doi pubmed - Services CfMM. Hospice. 2022. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Hospice.
- Rubin EB, Buehler AE, Halpern SD. States worse than death among hospitalized patients with serious illnesses. JAMA Intern Med. 2016;176(10):1557-1559.
doi pubmed pmc - Hwang F, Boardingham C, Walther S, Jacob M, Hidalgo A, Gandhi CD, Mosenthal AC, et al. Establishing goals of care for patients with stroke and feeding problems: an interdisciplinary trigger-based continuous quality improvement project. J Pain Symptom Manage. 2018;56(4):588-593.
doi pubmed - Reidy J, Savageau JA, Sullivan K, Nagpal V. Assessing goals-of-care documentation during the COVID-19 patient surge in an academic safety-net medical center. J Palliat Med. 2022;25(2):282-290.
doi pubmed - Steigleder T, Kollmar R, Ostgathe C. Palliative care for stroke patients and their families: barriers for implementation. Front Neurol. 2019;10:164.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


