| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Case Report
Volume 15, Number 5, May 2023, pages 274-278
A Case of Non-Tachycardic Atrial Fibrillation Whose Left Ventricular Systolic Dysfunction Improved After Catheter Ablation
Asami Yamashitaa, Shunsuke Kiuchib, c, Takanori Ikedab
aDivision of Cardiovascular Medicine, Department of Internal Medicine, Toho University Faculty of Medicine, Ota-ku, Tokyo 143-8541, Japan
bDepartment of Cardiovascular Medicine, Toho University Graduate School of Medicine, Ota-ku, Tokyo 143-8541, Japan
cCorresponding Author: Shunsuke Kiuchi, Department of Cardiovascular Medicine, Toho University Graduate School of Medicine, Ota-ku, Tokyo 143-8541, Japan
Manuscript submitted March 15, 2023, accepted April 29, 2023, published online May 31, 2023
Short title: Improved LVEF in a Non-Tachycardic AF by CA
doi: https://doi.org/10.14740/jocmr4908
| Abstract | ▴Top |
It is difficult to identify the causes and optimal treatment of heart failure (HF) in patients with atrial fibrillation (AF) and HF with reduced ejection fraction (EF) (HFrEF). Tachyarrhythmia can cause left ventricular (LV) systolic dysfunction called tachycardia-induced cardiomyopathy (TIC). In patients with TIC, conversion to sinus rhythm may lead to improvement in LV systolic dysfunction. However, it is unclear whether we should try to convert patients with AF without tachycardia to sinus rhythm. A 46-year-old man with chronic AF and HFrEF came to our hospital. His New York Heart Association (NYHA) classification was class II. The blood test showed a brain natriuretic peptide of 105 pg/mL. Electrocardiogram (ECG) and 24-h ECG showed AF without tachycardia. Transthoracic echocardiography (TTE) showed left atrial (LA) dilatation, LV dilatation, and diffuse LV hypokinesis (EF was 40%). Although he was optimized medically, NYHA classification II persisted. Therefore, he underwent direct current cardioversion and catheter ablation. After his AF converted to a sinus rhythm of heart rate (HR) 60 - 70 beats per minute (bpm), TTE showed improvement in LV systolic dysfunction. We gradually reduced oral medications for arrhythmia and HF. We subsequently succeeded in discontinuing all medications 1 year after catheter ablation. TTE performed between 1 and 2 years after catheter ablation showed normal LV function and normal cardiac size. During the 3 years of follow-up, there was no recurrence of AF, and he was not readmitted to the hospital. This patient showed the effectiveness of converting AF to sinus rhythm in patients without tachycardia.
Keywords: Heart failure; Ejection fraction; Atrial fibrillation; Tachycardia-induced cardiomyopathy; Catheter ablation
| Introduction | ▴Top |
In patients with atrial fibrillation (AF) and heart failure (HF) with reduced ejection fraction (EF) (HFrEF), it is hard to pinpoint the cause of HF and to choose an optimal treatment. It is known that tachycardia causes left ventricular (LV) dysfunction and HF. In particular, tachyarrhythmia can cause LV systolic dysfunction called tachycardia-induced cardiomyopathy (TIC). On the other hand, LV systolic dysfunction may improve in TIC with appropriate treatment such as catheter ablation and/or medication [1]. Therefore, it is important to properly diagnose and treat LV systolic dysfunction caused by TIC. AF is the most common cause of TIC [2]. In patients with HFrEF and tachycardia from AF, conversion to sinus rhythm may lead to improvement in LV systolic dysfunction. However, it is unclear whether patients with AF without tachycardia should be converted to sinus rhythm. We herein report the case of an AF patient without tachycardia whose LV systolic dysfunction improved after catheter ablation.
| Case Report | ▴Top |
The patient was a 46-year-old man with HFrEF and chronic AF. Two years before he came to our hospital, he was hospitalized elsewhere secondary to a first presentation of HF. He was diagnosed with dilated cardiomyopathy based on examinations, including coronary angiography. AF was indicated at that time, and it continued for approximately 2 years. He started taking warfarin at that time and it was continued for 2 years. He has no family history of heart disease, and hyperuricemia indicated anamnesis. He has a history of smoking for 25 years and drinking alcohol only occasionally. At the time of transfer to our hospital, he had been treated with the following medications: azosemide 30 mg, eplerenone 25 mg, bisoprolol 2.5 mg, febuxostat 20 mg, rivaroxaban 15 mg, and amiodarone 200 mg/day.
His HF class according to the New York Heart Association (NYHA) classification was II.
Physical examination revealed a pulse rate of 74 beats per minute (bpm) and arterial blood pressure (BP) of 96/68 mm Hg. His body mass index was 30.5 kg/m2. Blood test showed a brain natriuretic peptide (BNP) of 105 pg/mL. No other remarkable laboratory data, such as renal and thyroid dysfunction, abnormal levels of aldosterone and catecholamine were shown. Chest X-ray (Fig. 1) revealed expansion of the cardiothoracic ratio to 57%, while electrocardiogram (ECG) revealed AF with a heart rate (HR) of 74 bpm and no specific change in ST-T wave (Fig. 2). Transthoracic echocardiography (TTE) showed left atrial (LA) dilatation (52 × 38 mm from apical four-chamber view), LV dilatation (LV end-diastolic diameter of 57 mm from parasternal long-axis view), and diffuse LV hypokinesis without particular valve disease (EF of 40% from the Teichholz method with M-mode, average of measurements taken at multiple heartbeats) (Fig. 3). Holter ECG monitoring showed a total HR of 104,114 beats/day and an average HR of 76 bpm with all-day AF. During outpatient visits, he underwent ECG and Holter ECG several times and tachycardia was not observed in any of these examinations.
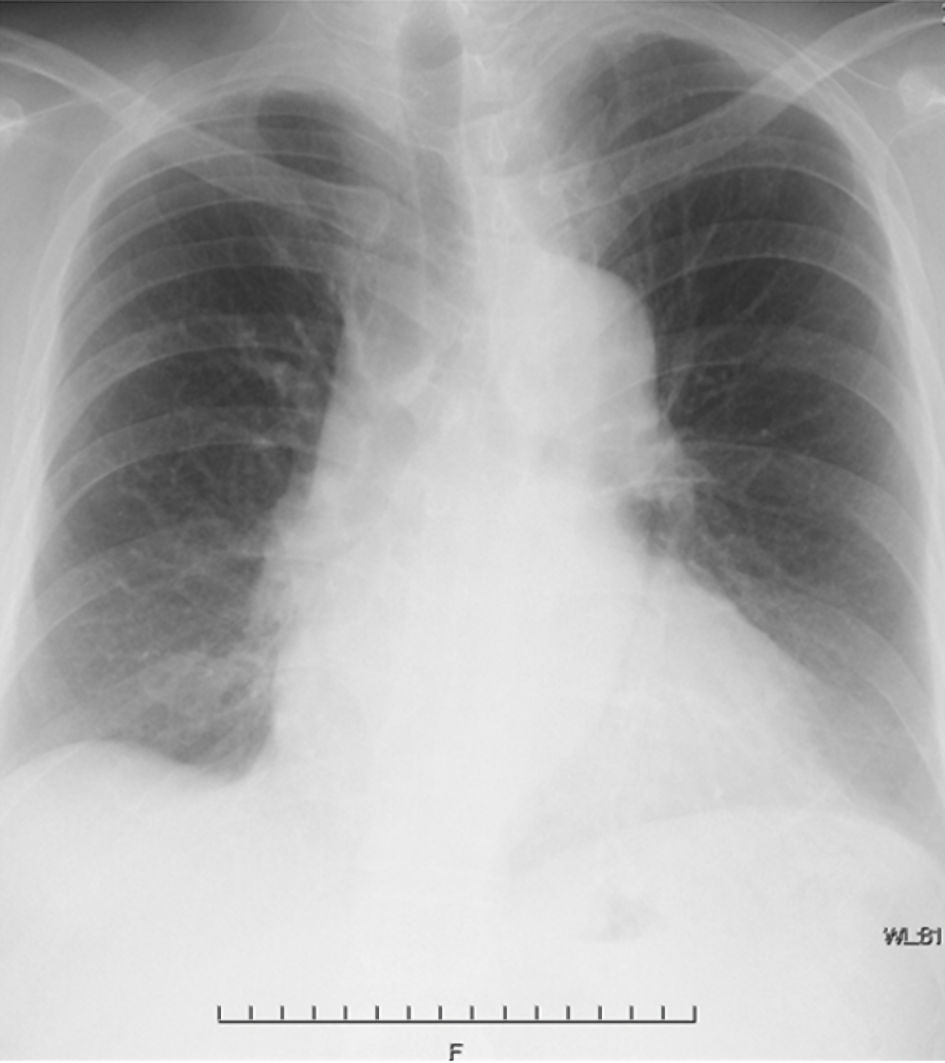 Click for large image | Figure 1. Chest X-ray on the day of first visit. Cardiothoracic ratio is 57%. |
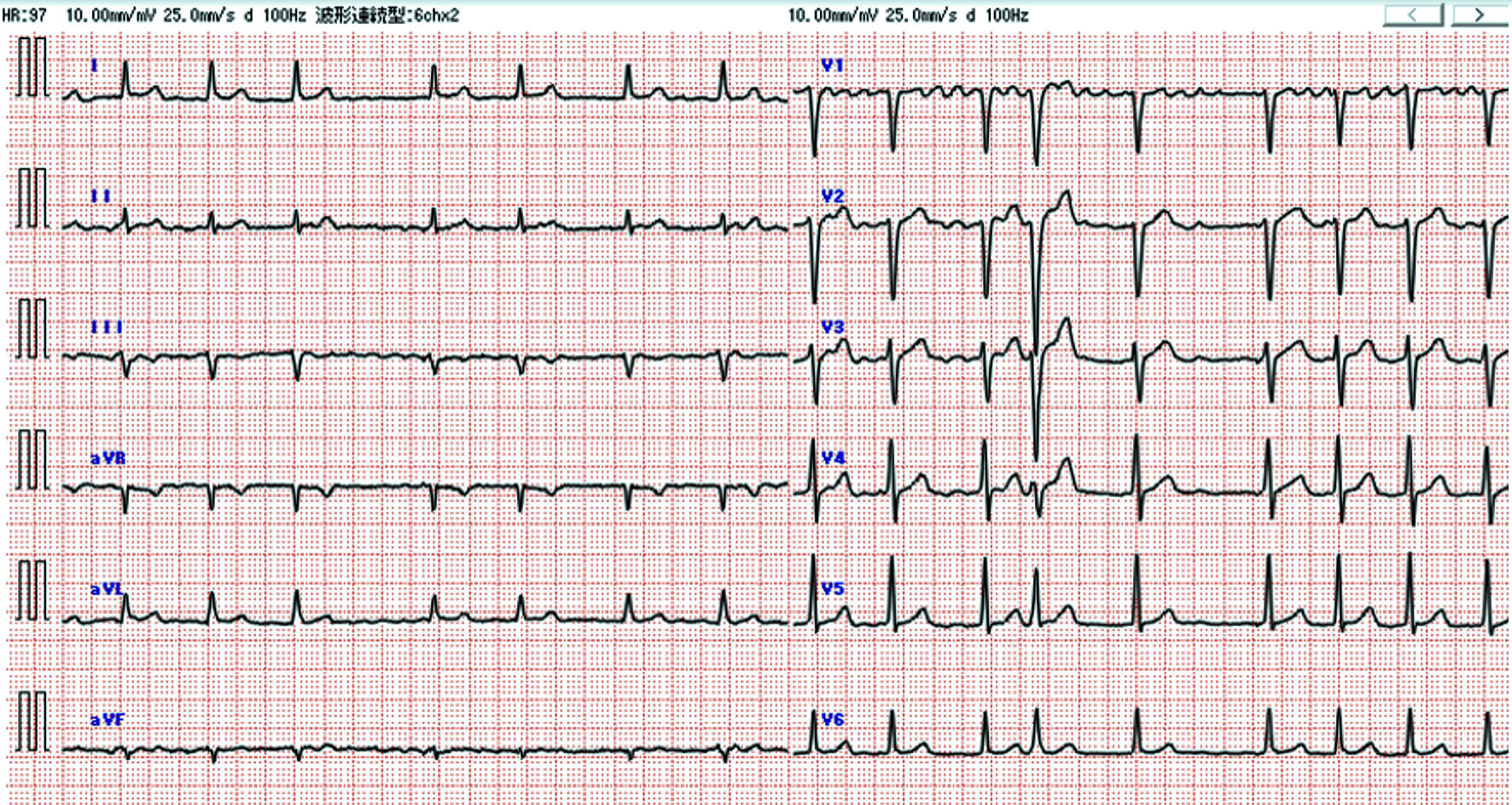 Click for large image | Figure 2. Electrocardiogram on the day of first visit: atrial fibrillation with a heart rate of 74 beats per minute (bpm) with no specific change in ST-T wave. |
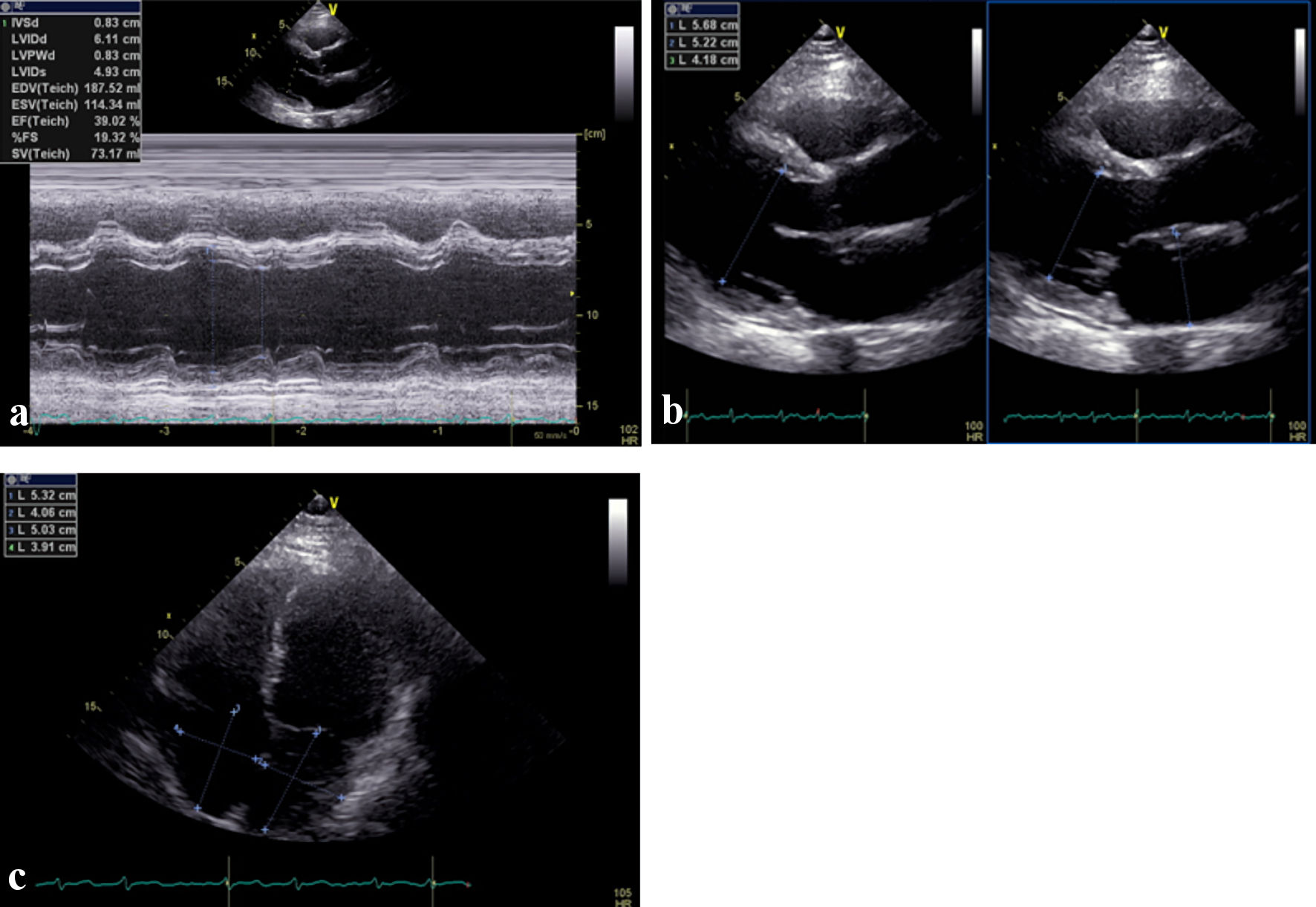 Click for large image | Figure 3. Transthoracic echocardiography on the day of first visit. (a) Diffuse left ventricular hypokinesis and ejection function of 40% from the Teichholz method with M-mode. (b) Left ventricular and left atrium dilatation. (c) Left atrium and right atrium dilatation. |
Renin-angiotensin-aldosterone system inhibitors could not be introduced because of low BP (sodium-glucose cotransporter 2 inhibitors were unavailable at that time), and NYHA classification II persisted. He therefore underwent direct current cardioversion. AF was converted to sinus rhythm with an HR of 60 bpm after direct current cardioversion. After 4 months, radiofrequency catheter ablations of the left and right, upper and lower pulmonary vein isolation, and cavotricuspid isthmus ablation were performed.
ECG performed after catheter ablation persistently showed sinus rhythm of HR 60 - 70 bpm. TEE performed 1 month after catheter ablation showed improvement in LV systolic dysfunction (EF of 58% from the Teichholz modified Simpson method with M-mode apical four-chamber view). His BNP which was 105 pg/mL at the time of first visit changed as 162 pg/mL at the time of direct current cardioversion, 110 pg/mL at the time of catheter ablation, 63 pg/mL after 2 months from catheter ablation and 4.5 pg/mL after 1 year from catheter ablation.
After catheter ablation, there was no AF recurrence, and we could stop antiarrhythmic and anticoagulant drugs. Also, as EF recovered, we gradually decrease cardioprotective medicines. Cardiac function continued to be maintained and finally no medication was required 1 year after catheter ablation.
We succeeded in discontinuing all medications 1 year after catheter ablation. TTE performed between 1 and 2 years after catheter ablation showed normal LV function with an EF of 68-74% and normal cardiac size. During the 3 years of follow-up, there was no recurrence of AF, and he was not rehospitalized.
| Discussion | ▴Top |
It is important but sometimes difficult to identify the cause of LV dysfunction and HF in the treatment of HFrEF. When LV dysfunction and dilatation are observed and there is no ischemic heart disease, patients tend to be diagnosed easily, as with this patient with dilated cardiomyopathy. However, we need to consider the possibility of cardiomyopathy caused by arrhythmia even when the HR is properly controlled. In AF and HFrEF patients, it is difficult to decide whether we should convert AF to sinus rhythm by catheter ablation, especially when there is no tachycardia [3].
Although tachycardia was not observed in this patient, he was presenting with HF symptoms. It is reported that AF may lead to systolic dysfunction even there was no tachycardia. Irregular ventricular activity, the loss of atrial contraction, activation of neurohormonal and pro-fibrotic pathways would contribute to reduced cardiac output [4]. These factors could have been the cause of HF in this patient.
It has been reported that a rhythm control therapy using antiarrhythmic drugs did not reduce the mortality and death rate from cardiovascular causes, compared with a rate control therapy [5, 6]. These results were the same in studies targeting both patients with and without HF.
In contrast, it has been reported that there are also some studies on HFrEF comparing rhythm control using catheter ablation and rate control. These studies indicated that catheter ablation was associated with an 8.5-14% increase in left ventricular ejection fraction (LVEF), but rate control did not improve LVEF [4, 7]. Also combined with this effect is the fact that the death rates from any cause, cardiovascular causes, and hospitalization for worsening HF in the AF and HFrEF patients who underwent catheter ablation were significantly lower than those of patients who underwent oral medical therapy [8]. Additionally, catheter ablation increased the maintenance rate of sinus rhythm, and exercise performance was significantly improved [9, 10]. Catheter ablation is also beneficial for maintaining the quality of life for AF and HF patients.
In patients with both AF and HF, it is difficult to determine whether HF was caused by AF or whether HF was accompanied by AF. The former often presents with cardiomyopathy called TIC, in which patients have AF with tachycardia. The European Society of Cardiology (ESC) guidelines provide class I catheter ablation to reverse LV dysfunction in AF patients when TIC is highly probable because sinus rhythm maintenance by catheter ablation is considered to be particularly effective for TIC [11]. In the latter, catheter ablation is of class IIa indication in some AF patients with HFrEF for the purpose of improving survival and reducing the hospitalization for HF according to ESC guidelines, because, as the severity of HF increases, the complication of AF increases [12]. However, atrial fibrosis is also involved in the development of AF, and it has also been reported that fibrosis differs depending on the underlying heart disease [13]. We think that the abovementioned reports included many details about the former patient; however, it is difficult to identify patients in whom catheter ablation is effective among the latter cases. It was recently reported that death from cardiovascular causes, stroke, and hospitalization with worsening of HF or acute coronary syndrome occurred less often in patients treated by early rhythm control therapy (including catheter ablation and medical therapy) [14]. In this report, early sinus rhythm control was effective in this patient. As catheter ablation is an invasive treatment and has various complications, whether catheter ablation or medical rhythm control therapy is employed should be decided based on the patient’s background, especially in institutions where catheter ablation cannot be performed. It is also useful to consider the pros and cons of catheter ablation at institutions where it can be performed. In both therapies, converting to sinus rhythm in the early period might be effective as in this patient.
Conclusions
This case report indicated the efficacy of catheter ablation for HFrEF and AF patients without tachycardia. Identifying the cause of HFrEF and providing optimal treatment are important. Identification of HFrEF and AF patients without tachycardia in whom catheter ablation is effective should be the target of future studies.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained.
Author Contributions
AY and SK contributed to the concept of this manuscript and the acquisition and evaluation of the data. AY drafted the manuscript. All authors provided critical revision of the manuscript and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
CA: catheter ablation; HF: heart failure; AF: atrial fibrillation; EF: ejection fraction; HFrEF: heart failure with reduced ejection fraction; LV: left ventricular; TIC: tachycardia-induced cardiomyopathy; NYHA: New York Heart Association; ECG: electrocardiogram; TTE: transthoracic echocardiography; LA: left atrial; BP: blood pressure; BNP: brain natriuretic peptide; HR: heart rate; ESC: European Society of Cardiology
| References | ▴Top |
- Gopinathannair R, Etheridge SP, Marchlinski FE, Spinale FG, Lakkireddy D, Olshansky B. Arrhythmia-induced cardiomyopathies: mechanisms, recognition, and management. J Am Coll Cardiol. 2015;66(15):1714-1728.
doi pubmed pmc - Fujino T, Yamashita T, Suzuki S, Sugiyma H, Sagara K, Sawada H, Aizawa T, et al. Characteristics of congestive heart failure accompanied by atrial fibrillation with special reference to tachycardia-induced cardiomyopathy. Circ J. 2007;71(6):936-940.
doi pubmed - Carlisle MA, Fudim M, DeVore AD, Piccini JP. Heart failure and atrial fibrillation, like fire and fury. JACC Heart Fail. 2019;7(6):447-456.
doi pubmed - Prabhu S, Taylor AJ, Costello BT, Kaye DM, McLellan AJA, Voskoboinik A, Sugumar H, et al. Catheter ablation versus medical rate control in atrial fibrillation and systolic dysfunction: the CAMERA-MRI study. J Am Coll Cardiol. 2017;70(16):1949-1961.
doi pubmed - Wyse DG, Waldo AL, DiMarco JP, Domanski MJ, Rosenberg Y, Schron EB, Kellen JC, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347(23):1825-1833.
doi pubmed - Roy D, Talajic M, Nattel S, Wyse DG, Dorian P, Lee KL, Bourassa MG, et al. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med. 2008;358(25):2667-2677.
doi pubmed - Al Halabi S, Qintar M, Hussein A, Alraies MC, Jones DG, Wong T, MacDonald MR, et al. Catheter ablation for atrial fibrillation in heart failure patients: a meta-analysis of randomized controlled trials. JACC Clin Electrophysiol. 2015;1(3):200-209.
doi pubmed pmc - Marrouche NF, Brachmann J, Andresen D, Siebels J, Boersma L, Jordaens L, Merkely B, et al. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med. 2018;378(5):417-427.
doi pubmed - Jones DG, Haldar SK, Hussain W, Sharma R, Francis DP, Rahman-Haley SL, McDonagh TA, et al. A randomized trial to assess catheter ablation versus rate control in the management of persistent atrial fibrillation in heart failure. J Am Coll Cardiol. 2013;61(18):1894-1903.
doi pubmed - Chen S, Purerfellner H, Meyer C, Acou WJ, Schratter A, Ling Z, Liu S, et al. Rhythm control for patients with atrial fibrillation complicated with heart failure in the contemporary era of catheter ablation: a stratified pooled analysis of randomized data. Eur Heart J. 2020;41(30):2863-2873.
doi pubmed - Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomstrom-Lundqvist C, Boriani G, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373-498.
doi pubmed - Maisel WH, Stevenson LW. Atrial fibrillation in heart failure: epidemiology, pathophysiology, and rationale for therapy. Am J Cardiol. 2003;91(6A):2D-8D.
doi pubmed - Ohtani K, Yutani C, Nagata S, Koretsune Y, Hori M, Kamada T. High prevalence of atrial fibrosis in patients with dilated cardiomyopathy. J Am Coll Cardiol. 1995;25(5):1162-1169.
doi pubmed - Kirchhof P, Camm AJ, Goette A, Brandes A, Eckardt L, Elvan A, Fetsch T, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med. 2020;383(14):1305-1316.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


