| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 6, June 2022, pages 237-243
Association of Severe Obesity and Chronic Obstructive Pulmonary Disease With Pneumonia Following Non-Cardiac Surgery
Kwaku Owusu-Bediakoa, Kayla Pfaffa, b, c, Nguyen K. Trama, David L. Stahld, Joseph D. Tobiasa, d, Olubukola O. Nafiua, d, Christian Mpodya, d, e
aDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
bHeritage College of Osteopathic Medicine - Dublin Campus, Dublin, OH, USA
cOhio University Athens, Athens, OH, USA
dDepartment of Anesthesiology & Pain Medicine, The Ohio State University, Columbus, OH, USA
eCorresponding Author: Christian Mpody, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 42305, USA
Manuscript submitted May 10, 2022, accepted June 13, 2022, published online June 27, 2022
Short title: Obesity and COPD in Postoperative Pneumonia
doi: https://doi.org/10.14740/jocmr4741
| Abstract | ▴Top |
Background: Pneumonia is the third most common surgical complication after urinary tract infection and wound infections. In addition to increased mortality, patients who develop postoperative pneumonia have a higher risk of prolonged hospital stay, intensive care unit (ICU) admissions, and higher healthcare costs. Obesity and chronic obstructive pulmonary disease (COPD) are both independent risk factors for the development and severity of postoperative pneumonia, although the combined effect of these comorbidities is unknown. Therefore, we evaluated whether the combination of severe obesity and COPD is associated with an increased risk of postoperative pneumonia.
Methods: We performed a multicenter retrospective cohort study of 365,273 patients aged 18 - 64 years who were either severely obese (body mass index (BMI) ≥ 40 kg/m2) or normal-weight (BMI between 18.6 and 24.9 kg/m2) and underwent general surgery, orthopedic surgery, neurosurgery, otolaryngology surgery, urology surgery, and vascular surgery in the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) participating hospitals from 2014 to 2018. We evaluated the combined effect of COPD and severe obesity on the risk for postoperative pneumonia, unplanned tracheal reintubation, and extended length of stay.
Results: The co-occurrence of severe obesity and COPD appeared to have a protective effect on the risk of postoperative pneumonia. In the presence of COPD, patients with severe obesity were 14% less likely to develop pneumonia compared to their normal-weight counterparts (2.9% vs. 4.4%; adjusted relative risk (RR): 0.76; 95% confidence interval (CI): 0.60, 0.95). In addition, in the presence of COPD, severe obesity conferred a lower risk for requiring an extended length of stay (37.6% vs. 47.9%; adjusted RR: 0.83; 95% CI: 0.78, 0.89).
Conclusions: Counterintuitively, the co-occurrence of severe obesity with COPD appeared to buffer the negative impact of COPD on postoperative pneumonia, unplanned tracheal reintubation, and prolonged hospital stay after noncardiac surgery. These findings are consistent with the obesity paradox and warrant further investigations.
Keywords: Severe obesity; COPD; Postoperative pneumonia; Unplanned tracheal reintubation
| Introduction | ▴Top |
Pneumonia is the third most common surgical complication after urinary tract infections and wound infections and is associated with significant perioperative morbidity [1, 2]. Patients who develop postoperative pneumonia have longer hospital stays, are more likely to be admitted to the intensive care unit (ICU) and are at a higher risk of early postoperative mortality [3-5]. The morbidity of pneumonia accounts for an additional 6 - 9 hospital days resulting in approximately $46,000 - $52,466 in hospital costs per patient after abdominal surgery [6]. In addition, under the Patient Protection and Affordable Care Act, hospitals with a high rate of 30-day readmissions for Medicare patients incur financial penalties [7]. Therefore, an improved understanding of complex risk factors associated with postoperative pneumonia may help identify these at-risk patients for targeted postoperative monitoring and rehabilitation.
Obesity and chronic obstructive pulmonary disease (COPD) are both independent risk factors for the development and severity of postoperative pneumonia [8-13]. Postoperative infections are highest among severely obese patients, potentially due to impaired immune function [14-17]. Severely obese patients may be at higher risk for aspiration because of their susceptibility to gastroesophageal reflux and hiatal hernia [18]. Furthermore, anatomical changes, including excess adipose tissue in pharyngeal walls, increased intraabdominal pressure, and decreased chest wall compliance, may predispose patients with obesity to upper airway obstruction, reduced lung volume, airway collapse, atelectasis, and postoperative respiratory failure [18, 19]. In patients with COPD, increased susceptibility to pulmonary infection has been attributed to several factors, including impaired gas exchange and reduced mucociliary clearance, inflammation from airway instrumentation, preoperative airway bacterial colonization, and surgery-induced immunosuppression [20-22].
Therefore, it is reasonable to assume that the combined effect of obesity and COPD could potentiate the risk of postoperative pneumonia. Unfortunately, research examining both comorbidities in relation to postoperative pneumonia is currently unavailable. Therefore, this study evaluated whether the joint presence of obesity and COPD in patients increases their risk of postoperative pneumonia among a cohort of patients who underwent inpatient surgical procedures.
| Materials and Methods | ▴Top |
Data source
We analyzed a multicenter retrospective dataset from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database from 2014 to 2018. The NSQIP is a multi-institutional surgical risk-adjusted, outcomes-based program that collects over 135 pre, intra, and postoperative clinical variables, including demographics, comorbidities, laboratory values, and tracks patient outcomes for up to 90 days postoperatively from > 600 participating hospitals [23]. In addition, trained surgical clinical reviewers identify data by current procedural terminology, collect, record data, and periodically perform random audits to ensure data accuracy and fidelity [23]. Our Institutional Review Board waived informed consent because our study was not considered human subjects research. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Study design and population
We performed a retrospective cohort study of patients aged between 18 and 64 years who were either severely obese (body mass index (BMI) ≥ 40 kg/m2) or normal-weight (BMI between 18.6 and 24.9 kg/m2) [24] and underwent general surgery, orthopedic surgery, neurosurgery, otolaryngology surgery, urology surgery, and vascular surgery. We excluded patients who had a history of dyspnea prior to surgery, required mechanical ventilation in the 48 h prior to surgery, were diagnosed with sepsis preoperatively, or who were admitted for emergency surgery.
Outcome of interest
The outcome of interest was postoperative pneumonia, diagnosed when predefined standardized criteria (clinical, radiological, or laboratory) are met. The radiological criteria consist of a chest radiological examination that demonstrates either an infiltrate, a consolidation, a cavitation, or a pleural effusion. The clinical (or laboratory) criteria include meeting one of two sections: 1) New onset of purulent sputum, or change in the character of sputum, or increased respiratory secretions, or increased suctioning requirements; new onset or worsening cough, dyspnea, or tachypnea; rales or rhonchi, worsening gas exchange; 2) Microscopic evidence of bacterial pneumonia. The clinical, radiologic, and microbiologic criteria used in the NSQIP were summarized here (Supplementary Material 1, www.jocmr.org). Our secondary outcome was unplanned tracheal reintubation within 30 days following surgery. We also explored the risk of extended length of postoperative hospital stay, defined as length of stay (LOS) longer than the 75th percentile of the study cohort.
Statistical analysis
We summarized categorical variables as frequencies and column percentages. Non-continuous variables were summarized as median (interquartile range (IQR)). We evaluated the risk of pneumonia in the presence or absence of COPD and according to whether patients were severely obese or normal-weight. To this end, we first divided the study population into four mutually exclusive groups: 1) Normal-weight patients without COPD (doubly unexposed); 2) Normal-weight patients with COPD; 3) Severely obese patients without COPD; and 4) Severely obese patients with COPD (doubly exposed). We then used log-binomial regression models to estimate the relative risk (RR) and its 95% confidence intervals (CIs) adjusting for covariates, selected a priori, based on our hypothesis of confounding the association between COPD and postoperative pneumonia: gender (female vs. male), current smoking status (within 1 year of surgery), American Society of Anesthesiologists (ASA) physical classification (≥ 3 vs. < 3), diabetes (noninsulin-dependent or insulin-dependent diabetes mellitus: yes vs. no), dyspnea (at rest or moderate exertion: yes vs. no), functional health status within 30 days of surgery (dependent vs. independent), history of chronic heart failure within 30 days of surgery (yes vs. no), hypertension (yes vs. no), corticosteroid use for a chronic condition (yes vs. no), and surgical specialty. We considered being statistically significant a P value of < 0.05. All analyses were performed with STATA 16 (StataCorp).
| Results | ▴Top |
Demographic and clinical characteristics
We analyzed a total of 365,273 patients who met inclusion criteria during the 5-year study period spanning between 2014 and 2018, of whom 9,329 (2.6%) had COPD (Table 1). Among patients without COPD, 50.4% (n = 179,451) were normal-weight, and 49.6% (n = 176,493) were severely obese. Among patients with COPD, 54.6% (n = 5,095) were normal-weight, and 45.4% (n = 4,234) were severely obese. In the absence of COPD, severely obese patients were more likely to be female (70.1% vs. 54.8%), to have an ASA class ≥ 3 (72.1% vs. 39.9%), to have diabetes (23.6% vs. 7.2%), to have hypertension requiring medication (47.0% vs. 22.7%); but less likely to have smoked within 1 year of surgery (14.3% vs. 28.5%) and use steroid for a chronic condition (3.1% vs. 7.0%). Similar differences were observed between normal-weight and severely obese patients in the presence of COPD.
 Click to view | Table 1. Baseline Characteristics of the Study Population (NSQIP 2014 - 2018) |
Combined effects of obesity and COPD
Out of the 365,273 total patients, 3,554 developed pneumonia (1.0%), 2,443 required unplanned tracheal reintubation following surgery (0.7%), and 100,785 required an extended length of hospital stay (27.6%). Overall, patients with COPD were more likely to develop pneumonia following surgery (3.7% vs. 0.9%; adjusted RR: 2.07; 95% CI: 1.84, 2.33). In addition, COPD conferred a higher risk of unplanned tracheal reintubation (2.4% vs. 0.6%; adjusted RR: 1.80; 95% CI: 1.56, 2.08) and extended LOS (43.2% vs. 27.2%; adjusted RR:1.12; 95% CI: 1.08, 1.15) (Fig. 1).
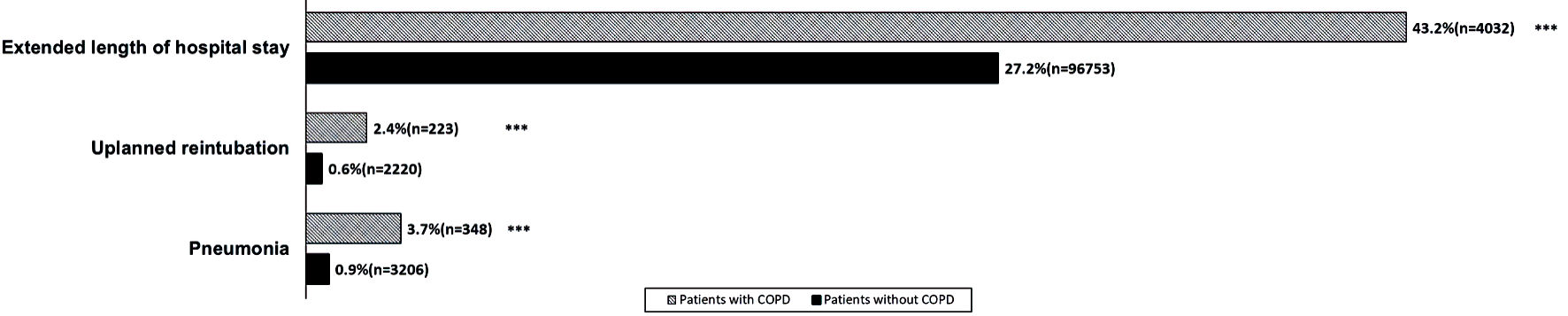 Click for large image | Figure 1. Thirty-day cumulative incidence of postoperative pneumonia, unplanned reintubation, and requirement for an extended postoperative LOS among 450,405 patients undergoing general surgery. Patients with COPD were more likely to develop postoperative pneumonia (adjusted RR: 2.07; 95% CI: 1.84, 2.33), require unplanned reintubation (adjusted RR: 1.80; 95% CI: 1.56, 2.08) and extended LOS (adjusted RR:1.12; 95% CI: 1.08, 1.15), after adjusting for gender, current smoking status, American Society of Anesthesiologists (ASA) physical classification, diabetes, functional health status within 30 days of surgery, history of chronic heart failure within 30 days of surgery, hypertension, corticosteroid use for a chronic condition, surgical specialty, and year of surgery. LOS: length of stay; COPD: chronic obstructive pulmonary disease; RR: relative risk; CI: confidence interval. |
The co-occurrence of severe obesity and COPD appeared to have a protective effect on the risk of postoperative pneumonia. Specifically, in the presence of COPD, patients with severe obesity were 14% less likely to develop pneumonia compared to their normal-weight counterparts (2.9% vs. 4.4%; adjusted RR: 0.76; 95% CI: 0.60, 0.95). The protective effect of severe obesity was also observed for the requirement of extended LOS (37.6% vs. 47.9%; adjusted RR: 0.83; 95% CI: 0.78, 0.89). In the presence of COPD, severe obesity conferred a lower risk of unplanned tracheal reintubation relative to normal weight, however, the statistical significance was lost after adjusting for baseline covariates (2.0% vs. 2.7%; adjusted RR: 0.79%; 95% CI: 0.60, 1.05) (Table 2).
 Click to view | Table 2. Associations of COPD, Stratified by Obesity Status, With Pneumonia, Unplanned Reintubation, and Extended LOS |
| Discussion | ▴Top |
Although obesity and COPD are known factors for the development of postoperative pneumonia, we are unaware of a previous study exploring their combined effects on the risk of postoperative pneumonia. Consistent with previous studies, we found that COPD conferred a higher risk of postoperative pneumonia with or without the presence of severe obesity [20, 25, 26]. However, counterintuitively, the presence of COPD carried a poorer prognosis in normal-weight patients relative to patients with severe obesity. Such a paradoxical relationship of severe obesity and COPD with postoperative pneumonia mirrors previous studies describing the perceived protection of obesity against some chronic debilitating diseases and post-surgical pulmonary complications [27-32]. Results from a retrospective cohort study on patients with COPD who used tobacco found that obesity was associated with a lower risk for mortality compared to normal weight [33]. Similarly, in another retrospective study of patients with pulmonary hypertension undergoing right-sided heart catheterization, patients with obesity had a lower risk of mortality compared to normal weight patients [34]. Our study findings together with data from these studies support and contribute to the growing body of evidence for the “obesity paradox”.
Several theories related to patient characteristics and provider behavior may explain why obesity appears to modify the association between COPD and postoperative pneumonia. One distinctive pathophysiologic feature of COPD is lung hyperinflation due to loss of normal lung elastase and limited expiratory flow [35, 36]. These changes decrease vital capacity and tidal volume and limit the ability to respond to increased minute ventilation needs, as seen after surgery [37-40]. Obesity decreases chest wall compliance (due to increasing mass), decreasing the expiratory reserve volume and, therefore, functional residual capacity. This results in increased atelectasis which may predispose to hypoxemia following general anesthesia. Thus, each condition has unique pathophysiologic reasons to increase the risk of pneumonia postoperatively. However, almost 40 years ago, Ora et al demonstrated that obesity protected against both static and dynamic lung hyperinflation producing favorable pulmonary mechanics which were protective against dyspnea [40]. Thus, it is likely that pulmonary mechanical challenges of obesity and COPD offset one another to normalize the risk of postoperative pneumonia.
Due to increased muscle mass, obese patients may have a greater nutritional and metabolic reserve, particularly of amino acids [41]. This increased reserve may better resist the catabolic effects of COPD and the initial infectious process than healthy-weight counterparts [42, 43]. Furthermore, the increased nutritional reserves may help obese patients to withstand the alteration in metabolic and inflammatory stress that follows surgery [15, 44]. In support of this assertion, Windsor and colleagues, in their study of risk factors for postoperative pneumonia, reported that patients with preoperative protein depletion were significantly more likely to develop pneumonia following abdominal surgery [45].
The comorbidity of COPD and severe obesity may trigger heightened monitoring from clinicians, thus reducing the risk of preventable complications, including pneumonia. In addition to increased monitoring, there may be heightened awareness among clinicians for intervening at the earliest sign of a respiratory issue in these patients, thereby preventing the development and progression of postoperative pneumonia [35]. Alternatively, in an effort to prevent perioperative complications, surgical patient selection may have biased toward “healthy” obese patients in this non-bariatric surgical cohort.
Our findings should be interpreted with the limitations inherent in a retrospective cohort study design, including the possibility of errors as can be seen in any large dataset. First, we did not separate the diagnostic subtypes of postoperative pneumonia, expressly ventilator-associated (VAP) vs. hospital-acquired, which may have different risk profiles in the obese and COPD population. Second, we did not examine the type and extent of surgery in the study cohort. Evidence suggests that the likelihood of developing post-surgical nosocomial infections ranges between 1.5% and 57% depending on the type and extent of surgery [6]. It may be possible that the severely obese COPD patients in our dataset were more likely to have minor surgeries than the healthy-weight COPD cohort, thereby reducing their potential risk of pneumonia. Third, it is plausible that postoperative pneumonia diagnosis could be misclassified by overlapping diagnoses such as aspiration pneumonia, pulmonary edema, and pulmonary embolism. Even so, we have no reason to believe that such misclassification bias will skew towards a particular weight group, and it is unlikely to be widespread enough to explain away our findings. Fourth, we did not explore the other possible causes of unintended tracheal reintubation such as anesthetic or surgical complications, nor did we explore other postoperative complications such as wound or urinary tract infections, and deep vein thrombosis (DVT), which may confound our findings on extended length of hospital stay. Finally, we could not determine from the NSQIP database, the severity of COPD among the study subjects based on the GOLD/ABCD classification. Given the information included in the database, we were unable to determine if chronic corticosteroid use was in place for the treatment of COPD.
Our retrospective study of a multi-institutional dataset revealed that the co-occurrence of severe obesity and COPD was associated with a lower rate of postoperative pneumonia. While various surgical complications are associated with COPD, its combination with severe obesity was counterintuitively associated with lower rates of extended hospital stay. However, we caution against interpreting this perceived protective effect of severe obesity in the presence of COPD to promote obesity or suggest excess weight gain in patients with COPD undergoing surgery. Although the underlying mechanism explaining the obesity paradox may differ across different health outcomes, our study provides additional evidence of the pulmonary mechanical consequences of the obesity paradox and warrant further research.
| Supplementary Material | ▴Top |
Suppl 1. NSQIP definition of pneumonia.
Acknowledgments
None to declare.
Financial Disclosure
The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest
The authors have no conflict of interest relevant to this article to disclose.
Informed Consent
Our Institutional Review Board waived informed consent because our study was not considered human subjects research.
Author Contributions
Kwaku Owusu-Bediako helped with study design/conduction, data interpretation, manuscript preparation and editing. Kayla Pfaff helped with manuscript preparation and editing. Nguyen K. Tram helped with data interpretation, manuscript preparation and editing. David L. Stahl helped with data interpretation, manuscript preparation and editing. Joseph D. Tobias helped with study design/conduction, statistical analysis, data interpretation, manuscript preparation and editing. Olubukola O. Nafiu and Christian Mpody helped with study design/conduct, statistical analysis, data interpretation, manuscript preparation and editing.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Chughtai M, Gwam CU, Mohamed N, Khlopas A, Newman JM, Khan R, Nadhim A, et al. The Epidemiology and Risk Factors for Postoperative Pneumonia. J Clin Med Res. 2017;9(6):466-475.
doi pubmed - Wren SM, Martin M, Yoon JK, Bech F. Postoperative pneumonia-prevention program for the inpatient surgical ward. J Am Coll Surg. 2010;210(4):491-495.
doi pubmed - Kazaure HS, Martin M, Yoon JK, Wren SM. Long-term results of a postoperative pneumonia prevention program for the inpatient surgical ward. JAMA Surg. 2014;149(9):914-918.
doi pubmed - Walder B, Story DA. Postoperative pneumonia: Can this important complication be predicted and anticipated? Eur J Anaesthesiol. 2019;36(2):87-89.
doi pubmed - Xu J, Hu J, Yu P, Wang W, Hu X, Hou J, Fang S, et al. Perioperative risk factors for postoperative pneumonia after major oral cancer surgery: A retrospective analysis of 331 cases. PLoS One. 2017;12(11):e0188167.
doi pubmed - Caparelli ML, Shikhman A, Jalal A, Oppelt S, Ogg C, Allamaneni S. Prevention of Postoperative Pneumonia in Noncardiac Surgical Patients: A Prospective Study Using the National Surgical Quality Improvement Program Database. Am Surg. 2019;85(1):8-14.
doi pubmed - Sweeney JF. Postoperative complications and hospital readmissions in surgical patients: an important association. Ann Surg. 2013;258(1):19-20.
doi pubmed - Simonsen DF, Sogaard M, Bozi I, Horsburgh CR, Thomsen RW. Risk factors for postoperative pneumonia after lung cancer surgery and impact of pneumonia on survival. Respir Med. 2015;109(10):1340-1346.
doi pubmed - Kornum JB, Norgaard M, Dethlefsen C, Due KM, Thomsen RW, Tjonneland A, Sorensen HT, et al. Obesity and risk of subsequent hospitalisation with pneumonia. Eur Respir J. 2010;36(6):1330-1336.
doi pubmed - Gupta H, Ramanan B, Gupta PK, Fang X, Polich A, Modrykamien A, Schuller D, et al. Impact of COPD on postoperative outcomes: results from a national database. Chest. 2013;143(6):1599-1606.
doi pubmed - Bare M, Monton C, Mora L, Redondo M, Pont M, Escobar A, Sarasqueta C, et al. COPD is a clear risk factor for increased use of resources and adverse outcomes in patients undergoing intervention for colorectal cancer: a nationwide study in Spain. Int J Chron Obstruct Pulmon Dis. 2017;12:1233-1241.
doi pubmed - Mica L, Keller C, Vomela J, Trentz O, Plecko M, Keel MJ. Obesity and overweight as a risk factor for pneumonia in polytrauma patients: a retrospective cohort study. J Trauma Acute Care Surg. 2013;75(4):693-698.
doi pubmed - Shimizu A, Tani M, Kawai M, Hirono S, Miyazawa M, Uchiyama K, Yamaue H. Influence of visceral obesity for postoperative pulmonary complications after pancreaticoduodenectomy. J Gastrointest Surg. 2011;15(8):1401-1410.
doi pubmed - Mullen JT, Moorman DW, Davenport DL. The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg. 2009;250(1):166-172.
doi pubmed - Falagas ME, Athanasoulia AP, Peppas G, Karageorgopoulos DE. Effect of body mass index on the outcome of infections: a systematic review. Obes Rev. 2009;10(3):280-289.
doi pubmed - Baik I, Curhan GC, Rimm EB, Bendich A, Willett WC, Fawzi WW. A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women. Arch Intern Med. 2000;160(20):3082-3088.
doi pubmed - Klekotka RB, Mizgala E, Krol W. The etiology of lower respiratory tract infections in people with diabetes. Pneumonol Alergol Pol. 2015;83(5):401-408.
doi pubmed - Lotia S, Bellamy MC. Anaesthesia and morbid obesity. Cont Educ Anaesth Crit Care Pain. 2008;8(5):151-156.
doi - Pedoto A. Lung physiology and obesity: anesthetic implications for thoracic procedures. Anesthesiol Res Pract. 2012;2012:154208.
doi pubmed - de Miguel-Diez J, Lopez-de-Andres A, Hernandez-Barrera V, Jimenez-Trujillo I, Mendez-Bailon M, de Miguel-Yanes JM, Jimenez-Garcia R. Postoperative pneumonia among patients with and without COPD in Spain from 2001 to 2015. Eur J Intern Med. 2018;53:66-72.
doi pubmed - Kim ES, Kim YT, Kang CH, Park IK, Bae W, Choi SM, Lee J, et al. Prevalence of and risk factors for postoperative pulmonary complications after lung cancer surgery in patients with early-stage COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:1317-1326.
doi pubmed - Gupta H, Gupta PK, Schuller D, Fang X, Miller WJ, Modrykamien A, Wichman TO, et al. Development and validation of a risk calculator for predicting postoperative pneumonia. Mayo Clin Proc. 2013;88(11):1241-1249.
doi pubmed - Kraemer K, Cohen ME, Liu Y, Barnhart DC, Rangel SJ, Saito JM, Bilimoria KY, et al. Development and evaluation of the American College of Surgeons NSQIP pediatric surgical risk calculator. J Am Coll Surg. 2016;223(5):685-693.
doi pubmed - Blackwell J. Identification, evaluation, and treatment of overweight and obese adults. J Am Acad Nurse Pract. 2002;14(5):196-198.
doi pubmed - Lee R, Lee D, Mamidi IS, Probasco WV, Heyer JH, Pandarinath R. Patients with chronic obstructive pulmonary disease are at higher risk for pneumonia, septic shock, and blood transfusions after total shoulder arthroplasty. Clin Orthop Relat Res. 2019;477(2):416-423.
doi pubmed - Liao KM, Tseng CJ, Chen YC, Wang JJ, Ho CH. Outcomes of laparoscopic cholecystectomy in patients with and without COPD. Int J Chron Obstruct Pulmon Dis. 2019;14:1159-1165.
doi pubmed - Yang CK, Teng A, Lee DY, Rose K. Pulmonary complications after major abdominal surgery: National Surgical Quality Improvement Program analysis. J Surg Res. 2015;198(2):441-449.
doi pubmed - Corrales-Medina VF, Valayam J, Serpa JA, Rueda AM, Musher DM. The obesity paradox in community-acquired bacterial pneumonia. Int J Infect Dis. 2011;15(1):e54-57.
doi pubmed - Lavie CJ, Alpert MA, Arena R, Mehra MR, Milani RV, Ventura HO. Impact of obesity and the obesity paradox on prevalence and prognosis in heart failure. JACC Heart Fail. 2013;1(2):93-102.
doi pubmed - Kalantar-Zadeh K, Abbott KC, Salahudeen AK, Kilpatrick RD, Horwich TB. Survival advantages of obesity in dialysis patients. Am J Clin Nutr. 2005;81(3):543-554.
doi pubmed - Curtis JP, Selter JG, Wang Y, Rathore SS, Jovin IS, Jadbabaie F, Kosiborod M, et al. The obesity paradox: body mass index and outcomes in patients with heart failure. Arch Intern Med. 2005;165(1):55-61.
doi pubmed - Thomas PA, Berbis J, Falcoz PE, Le Pimpec-Barthes F, Bernard A, Jougon J, Porte H, et al. National perioperative outcomes of pulmonary lobectomy for cancer: the influence of nutritional status. Eur J Cardiothorac Surg. 2014;45(4):652-659; discussion 659.
- Brigham EP, Anderson JA, Brook RD, Calverley PMA, Celli BR, Cowans NJ, Crim C, et al. Challenging the obesity paradox: extreme obesity and COPD mortality in the SUMMIT trial. ERJ Open Res. 2021;7(3).
doi pubmed - Tong C, Li T, Shen Y, Zhu H, Zheng J, Wu J. Obesity does not increase perioperative outcomes in older patients undergoing thoracoscopic anatomic lung cancer surgery. Front Oncol. 2022;12:881467.
doi pubmed - Galesanu RG, Bernard S, Marquis K, Lacasse Y, Poirier P, Bourbeau J, Maltais F. Obesity in chronic obstructive pulmonary disease: is fatter really better? Can Respir J. 2014;21(5):297-301.
doi pubmed - Ferguson GT. Why does the lung hyperinflate? Proc Am Thorac Soc. 2006;3(2):176-179.
doi pubmed - Drummond G. Surgery and respiratory muscles. Thorax. 1999;54(12):1140-1141.
doi pubmed - O'Donnell DE, Aaron S, Bourbeau J, Hernandez P, Marciniuk DD, Balter M, Ford G, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease - 2007 update. Can Respir J. 2007;14(Suppl B):5B-32B.
doi pubmed - Ora J, Laveneziana P, Ofir D, Deesomchok A, Webb KA, O'Donnell DE. Combined effects of obesity and chronic obstructive pulmonary disease on dyspnea and exercise tolerance. Am J Respir Crit Care Med. 2009;180(10):964-971.
doi pubmed - Ora J, Laveneziana P, Wadell K, Preston M, Webb KA, O'Donnell DE. Effect of obesity on respiratory mechanics during rest and exercise in COPD. J Appl Physiol (1985). 2011;111(1):10-19.
doi pubmed - Poulain M, Doucet M, Drapeau V, Fournier G, Tremblay A, Poirier P, Maltais F. Metabolic and inflammatory profile in obese patients with chronic obstructive pulmonary disease. Chron Respir Dis. 2008;5(1):35-41.
doi pubmed - Kastorini CM, Panagiotakos DB. The obesity paradox: methodological considerations based on epidemiological and clinical evidence—new insights. Maturitas. 2012;72(3):220-224.
doi pubmed - Rutten EP, Calverley PM, Casaburi R, Agusti A, Bakke P, Celli B, Coxson HO, et al. Changes in body composition in patients with chronic obstructive pulmonary disease: do they influence patient-related outcomes? Ann Nutr Metab. 2013;63(3):239-247.
doi pubmed - Kahlon S, Eurich DT, Padwal RS, Malhotra A, Minhas-Sandhu JK, Marrie TJ, Majumdar SR. Obesity and outcomes in patients hospitalized with pneumonia. Clin Microbiol Infect. 2013;19(8):709-716.
doi pubmed - Windsor JA, Hill GL. Risk factors for postoperative pneumonia. The importance of protein depletion. Ann Surg. 1988;208(2):209-214.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


