| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 9, Number 10, October 2017, pages 864-871
Lack of Needs Assessment in Cancer Survivorship Care and Rehabilitation in Hospitals and Primary Care Settings
Charlotte Handberga, b, c, Charlotte Maria Jensena, b, Thomas Mariboa, b
aDepartment of Public Health, Section for Clinical Social Medicine and Rehabilitation, Faculty of Health, Aarhus University, Denmark
bDEFACTUM, Central Denmark Region, Denmark
cCorresponding Author: Charlotte Handberg, Department of Public Health, Section for Clinical Social Medicine and Rehabilitation, Faculty of Health, Aarhus University, Denmark
Manuscript submitted August 11, 2017, accepted August 25, 2017
Short title: Needs Assessment in Cancer Survivorship Care
doi: https://doi.org/10.14740/jocmr3160w
| Abstract | ▴Top |
Background: Formalized and systematic assessment of survivorship care and rehabilitation needs is prerequisite for ensuring cancer patients sufficient help and support through their cancer trajectory. Patients are often uncertain as to how to express and address their survivorship care and rehabilitation needs, and little is known about specific, unmet needs and the plans necessary to meet them. There is a call for both ensuring survivorship care and rehabilitation for cancer patients in need and further for documenting the specific needs related to the cancer disease and its treatment. Thus the aim of this study was to describe specific survivorship care and rehabilitation needs and plans as stated by patients with cancer at hospitals when diagnosed and when primary care survivorship care and rehabilitation begins.
Methods: Needs assessment forms from cancer patients at two hospitals and two primary care settings were analyzed. The forms included stated needs and survivorship care and rehabilitation plans. All data were categorized using the International Classification of Functioning, Disability and Health (ICF).
Results: Eighty-nine patients at hospitals and 99 in primary care, stated their needs. Around 50% of the patients completed a survivorship care and rehabilitation plan. In total, 666 (mean 7.5) needs were stated by hospital patients and 836 (mean 8.0) by those in primary care. The needs stated were primarily within the ICF component “body functions and structure”, and the most frequent needs were (hospitals/primary care) fatigue (57%/67%), reduced muscle strength (55%/67%) and being worried (37%/36%).
Conclusions: The results underpin an urgent need for a systematic procedure to assess needs in clinical practice where cancer patients are being left without survivorship care and rehabilitation needs assessment. Gaining knowledge on needs assessment and the detailed description of needs and plans can facilitate targeted interventions. The findings indicate an urgent need to change the practice culture to be systematic in addressing and identifying survivorship care needs among patients with cancer. Further the findings call for considering the development of a new needs assessment form with involvement of both patients and healthcare professionals.
Keywords: Cancer; Survivorship care; Survivorship; Rehabilitation; Needs assessment; Hospitals; Primary care; International Classification of Functioning, Disability and Health
| Introduction | ▴Top |
Cancer survivors are often left in a gap between health care systems exposed to poorer health outcomes due to lack of survivorship care and rehabilitation [1, 2]. This is unfortunate since a growing body of evidence argues that cancer survivorship care and rehabilitation is effective and necessary to enhance patients’ health, improve the chances of survival and prevent further illness and prolonged side-effects [3-6]. Healthcare staff at hospitals and in primary care are responsible for conducting needs assessment in relation to survivorship care and rehabilitation; however, there are still reports that many cancer survivors experience unmet survivorship care and rehabilitation needs [7-9]. Little research has been conducted on the complexities of cancer survivorship needs assessment in a shared cancer care context.
Background
Patients with cancer are exposed to the risk of experiencing adverse physical, psychological and social symptoms as well as side effects as a result of their malignant disease and its treatment [6, 10]. Cancer survivorship care and rehabilitation addresses these symptoms and side effects, seeking to enhance daily functioning and quality of life through various interventions [11]. The specific aim of rehabilitation (in which we include survivorship care) is to optimize the patient’s physical, psychological, vocational and social functioning while countering the limitations imposed by the side effects of cancer treatments and/or comorbid conditions [12].
An increasing amount of evidence endorses cancer rehabilitation as beneficial, effective and necessary to improve patients’ health and quality of life, increase the chances of survival and prevent further illness and prolonged side and late effects [4-6, 13]. Cancer rehabilitation should be an integral part of treatment; however, a significant number of patients do not receive an assessment of rehabilitation needs even though this is described as prerequisite for ensuring the possibility to address needs and ensure referral to rehabilitation [14-16]. Cancer rehabilitation in the primary care system is available for all patients in Denmark. It usually includes a selection of interdisciplinary evidence-based interventions, such as physical training, stress relief and supportive care, and is aimed at restoring functioning and supporting the patient to achieve an independent and meaningful life [11, 17]. Patients are referred by a hospital doctor, nurse or other healthcare professional, by their general practitioner or by themselves.
Patients are however often uncertain as to how to express and address their rehabilitation needs, and little is known about specific, unmet needs and the plans necessary to meet them [18, 19]. There is a call for both ensuring rehabilitation for cancer patients in need and further documenting the specific needs related to the cancer illness and its treatment [20, 21]. Thus the aim of this study was to describe specific rehabilitation needs and plans as stated by patients with cancer at hospitals when diagnosed and when primary care rehabilitation begins.
| Materials and Methods | ▴Top |
Design and setting
The present study involved a cross-sectional survey of patients with cancer at hematology departments at two hospitals and patients with different cancers attending rehabilitation in two primary care settings in the Central Denmark Region. The study is part of a larger study entailing four studies on clinical practice on how needs assessment is organized and practiced among patients with cancer and their healthcare professionals.
Two separate sectors are responsible for rehabilitation in Denmark: 1) the regional level, which constitutes five regions responsible for hospital services and inpatient specialized rehabilitation, and 2) the local authority level, which constitutes 98 primary care settings responsible for general rehabilitation during or after hospitalization.
National policies recommend integrating cancer rehabilitation from the beginning of treatment, and all patients are entitled to an assessment of their needs at both hospitals at the time of diagnosis and in primary care [17]. A significant number of patients do not, however, receive an assessment and are not referred to rehabilitation [14, 15].
The two included hospitals have a background population of 1.3 million individuals. The two primary care settings have a background population of 333,000 and 57,000 individuals. Data were obtained from rehabilitation needs assessment forms (see below).
Participants
A convenience sample that included hematological patients was recruited from the two hospitals. These patients were chosen because this group of patients often have extensive rehabilitation needs due to the length and complexity of their illness and treatment [22]. In addition, the hematological wards were in the process of implementing needs assessment. Data were also obtained from all patients (with different types of cancer) in primary care cancer rehabilitation programmes. The reason for including all the patients in primary care was the low numbers of patients with hematological cancers.
Patients were eligible to participate in the study if they had a diagnosis of cancer, were aged 18 years or older, and had needs assessment conducted between April 2015 and December 2015. All patients cooperated in the process of assessment of their rehabilitation needs with a healthcare professional (nurses, physiotherapists or a dietician).
Ethical considerations
Ethical approval was obtained from the Danish Data Protection Agency approval (number 2007-58-0010). Eligible patients were invited to participate in the project, and both oral and written consent was given.
Needs assessment form
In the Central Denmark Region, a specific two-page paper needs assessment form is used (Fig. 1). Page 1 covers the six domains, practical, work/school, family, physical, emotional and spiritual/religious, and 58 fixed areas to identify and state possible needs. A tick in either “area” or “need for support” (or both) was registered as one stated need, which means each patient could potentially state 0 to 58 needs.
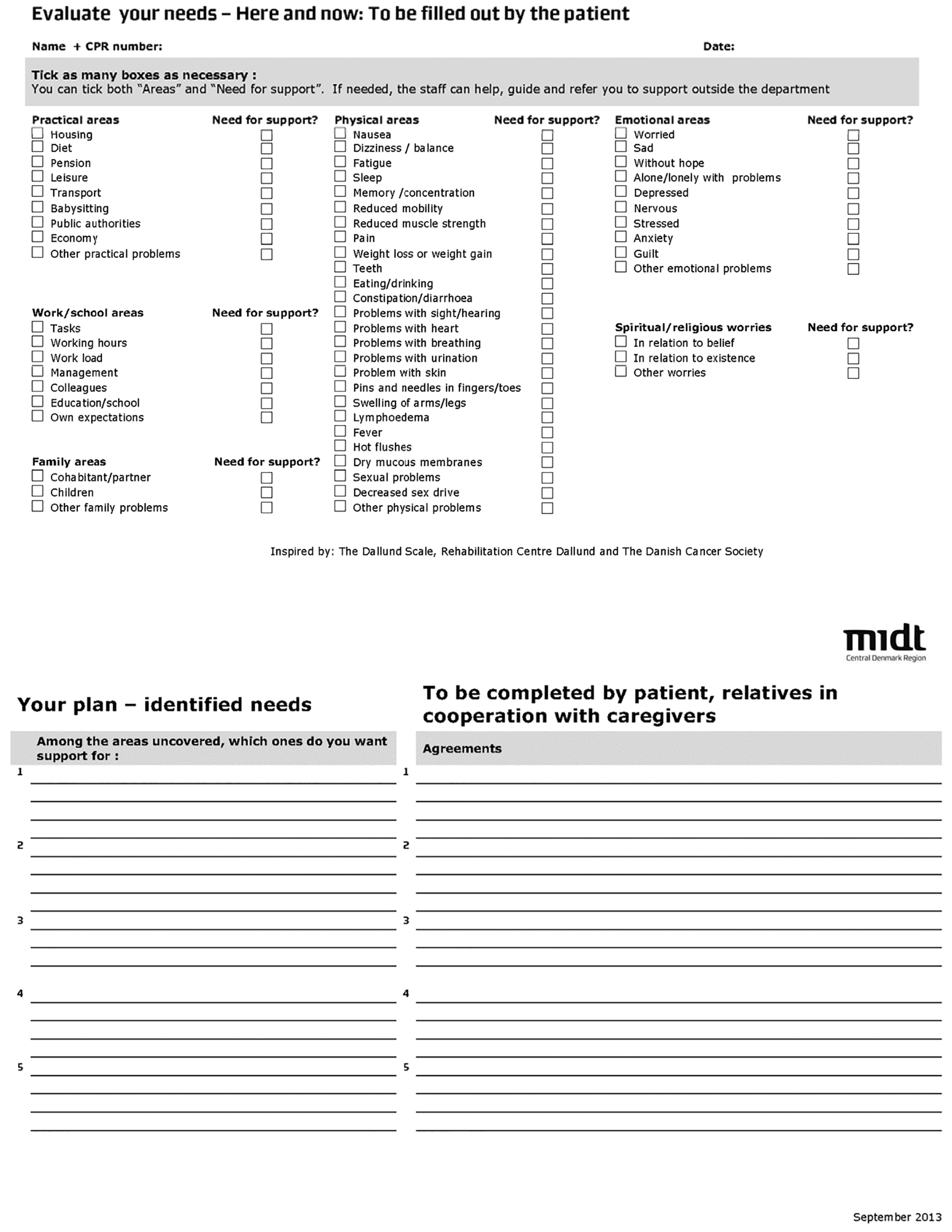 Click for large image | Figure 1. Needs assessment form. |
Page 2 consists of an area to state and document the rehabilitation plans to support the patient’s further cancer trajectory. The rehabilitation plans contain a blank space for stating identified needs and a blank space for plans. An identified need in the first blank space was registered as a rehabilitation plan, and each patient could have multiple plans.
The International Classification of Functioning, Disability and Health (ICF) was used to categorize stated needs and rehabilitation plans using the ICF linking rules [23].
Statistical analysis
Characteristics of patients were summarized using frequencies and proportions. Data from the hospitals and primary care (all four departments) were collated. All analyses were conducted using STATA 13 (StataCorp LP, College Station, TX, USA).
| Results | ▴Top |
A total of 933 patients with cancer, 703 at the two hospital departments and 230 in the two primary care settings, were admitted during the study period. Of these, 724 (78%) patients did not complete a needs assessment form and 21 (2%) did not wish to participate in the study (Fig. 2).
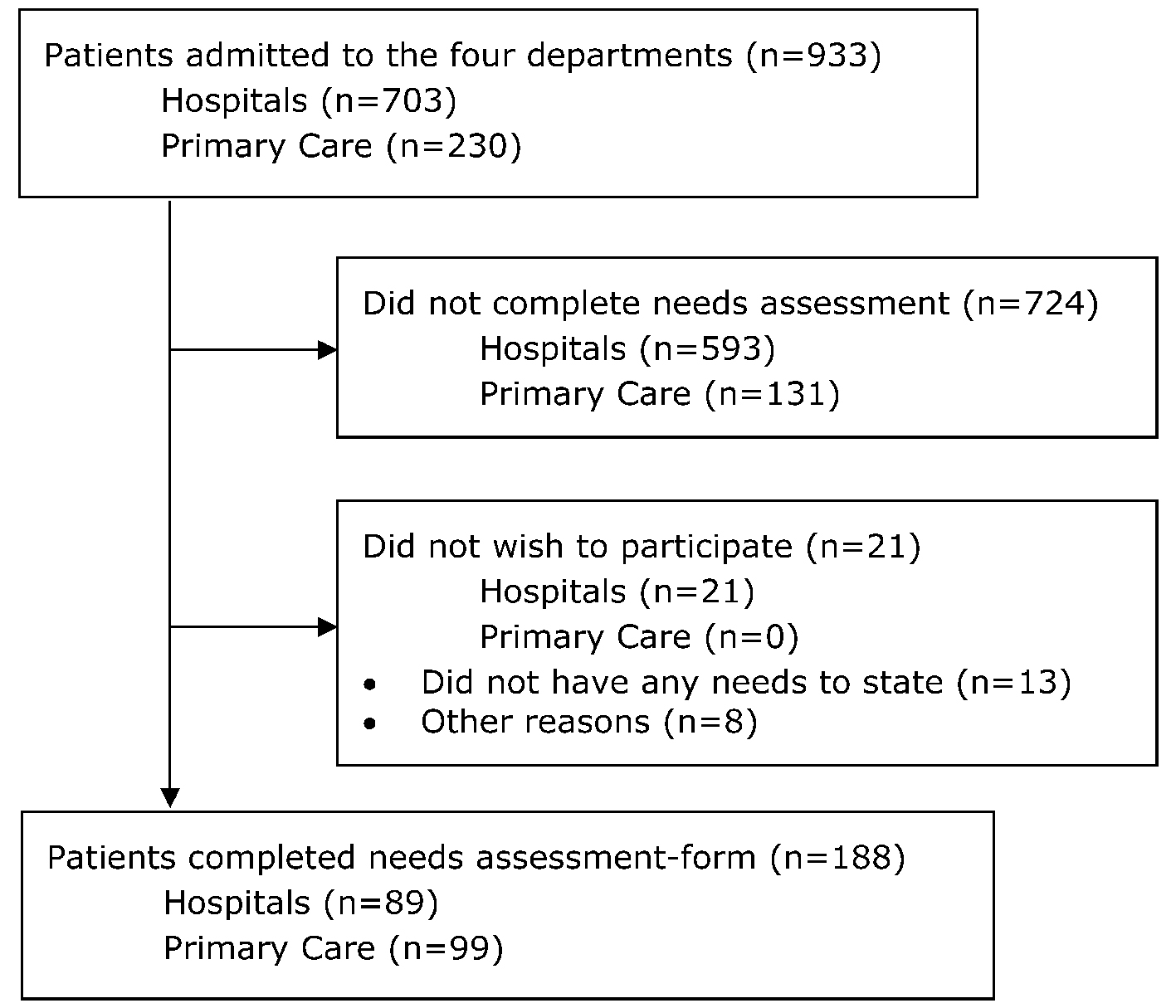 Click for large image | Figure 2. Flow diagram. |
Of all eligible patients, 188 (20%) agreed to participate and completed a needs assessment form in which they stated their needs. Baseline characteristics are shown in Table 1.
 Click to view | Table 1. Baseline Characteristics of the Study Population (n = 188) |
Stated needs and rehabilitation plans
In total, the 89 patients at the hospitals stated 666 needs, whereas the 99 patients in primary care stated 836 needs (Table 2). The patients that completed the needs assessment form stated around eight needs on average. Seven patients at the hospital stated no present needs, and they all expressed a wish for a new needs assessment after discharge. Almost half the patients completed a rehabilitation plan, and on average the patients had three plans (Table 2).
 Click to view | Table 2. Stated Rehabilitation Needs and Plans |
Table 3 shows the stated needs and rehabilitation plans categorized into ICF components. The most frequently stated needs, around 80% in both hospital and primary care patients, were categorized within ICF’s component “body functions and structure”. The most frequently stated plans were also allocated within “body functions and structure”, 59% for the hospital patients and 70% for primary care patients.
 Click to view | Table 3. Stated Needs and Rehabilitation Plans Categorized in ICF Components |
Needs identified by more than 20% of the hospital patients or primary care patients are shown in Table 4, and the largest groups of needs stated by both hospital and primary care patients were fatigue, reduced muscle strength and being worried.
 Click to view | Table 4. Tabel 4. Most Frequently Stated Needs |
| Discussion | ▴Top |
This is the first study to look at needs assessment culture in a cross-sectoral setting and specifically on needs and plans stated by the patients at both hospitals and in primary care. A growing body of evidence argues that rehabilitation is effective and necessary to enhance patient’s health, improve the chances of survival and prevent further illness and prolonged side effects [4-6, 13], supporting the need for knowledge in this area. The systematic analysis gave knowledge on the patients’ stated needs and plans and the distribution within the ICF framework. Contributing with knowledge in an unexplored field meant, however, that we did not have other studies to compare our results with. Overall, the implementation of needs assessment and the rate of the completion of rehabilitation plans seem to be a research area that is rather unexplored. Studies on needs assessment have been done in Denmark [8, 13, 15] and also in other countries [10, 24, 25], but the research in the cross-sectoral field is limited and needs further exploration.
The findings provide an insight into current practice on needs assessment, specifics of stated needs and plans in both hospital and primary care patients. Knowing that rehabilitation is effective [4-6, 13] and that the patients state many needs makes it problematic that only around 50% patients completed a rehabilitation plan. During the last few years, there has been a focus on improving and ensuring rehabilitation for patients with cancer, with particular emphasis on a systematic assessment of patients’ rehabilitation needs [26]; thus, the fact that only 50% of the patients completed a rehabilitation plan is unsatisfactory. In addition, all sectors in the healthcare system have an obligation to identify cancer patients’ need for rehabilitation [17, 26, 27], which makes it alarming that needs assessment is apparently only documented in 20% of the patients. If the hospital in relation to their needs assessment uncovers rehabilitation needs, they must refer the patient to primary care rehabilitation [17, 27], which may not take place if a needs assessment is not conducted systematically. When rehabilitation needs assessment is not systematically executed in clinical practice, the explanations for a high number of patients not completing an assessment remain unidentified and uncertain.
It is an important finding that 724 patients (593 at hospitals and 131 in primary care) did not complete the needs assessment form. The hospitals staff mentioned two overarching reasons for not completing the forms: 1) Implementation of the needs assessment form: The healthcare professionals were not familiar with the form and described it as meaningless. The design and content were described as awkward, and furthermore the staff found that the needs assessment in general was conducted too early after the diagnosis (at the latest 2 weeks after diagnosis at the hematological departments). 2) Uncertainty among the staff: The healthcare professionals expressed how they were uncertain as to what rehabilitation services completion of the needs assessment form led to and further that the electronic possibility to refer patients was difficult to understand. Hospital staff estimated that 80% of the missing assessments were due to implementation problems and 20% of the missing assessments were due to uncertainty. In primary care, the staff mentioned two reasons for patients not completing the forms: 1) No need for rehabilitation: It was decided by the patients that they did not need rehabilitation after the first consultation (often by phone). 2) Referral from another programme within the primary care setting: In this case, the patients had already completed a needs assessment. Staff from primary care estimated that 70% of the missing assessments were due to no need for rehabilitation and 30% of the missing assessments were due to referral from another programme. As described, the reasons for not completing the forms in primary care were related to distinct issues, whereas the reasons at the hospitals were primarily related to different barriers within the members of the staff. A recent study documented how healthcare professionals in oncology wards intentionally or unintentionally screened patients for rehabilitation needs, and it showed how this conduct was designed as a decisive mechanism in order to resolve when it would be relevant to begin discussing and providing rehabilitation information with the patients [28].
The fact that there has been no involvement of the patients or the healthcare professionals in the formulation of the needs assessment form could lead to a proposal for involvement of both groups in developing the form and content [29]. Still, this uncertainty calls for further studies, and some of the underlying reasons why so many patients did not complete the needs assessment form are therefore being explored further in follow-up studies that explore the perspectives of the healthcare professionals and the patients.
Gaining knowledge on needs assessment and the specifics of needs and plans facilitates the implementation of targeted rehabilitation interventions. Most needs were stated within the IFC component “body function and structure”. This may be due to the fact that the needs assessment form focuses on symptoms and disease and not everyday life. Symptoms and disease are for the most part within the “body function and structure” component. Having this center of attention could aim the patients’ needs in the direction of physical needs and symptoms [30]. Had the frame for the needs assessment form been more on the substance of rehabilitation instead of symptoms and disease, it might have conceptualized functioning in a holistic framework as comprising body functions, structures, activities and participation, and at the same time take cognisance of environmental and personal factors [30].
The use of ICF as a framework of functioning was shown to be applicable to get an overview on the distribution of needs and plans. ICF is traditionally used within other contexts than cancer treatment and rehabilitation, but ICF may prove useful across settings or countries to facilitate data comparisons and thereby facilitate a systematic coding scheme for health information systems [31]. In this study, it became apparent that it could have been profitable if the focus on the needs assessment form, as in the ICF, was on the person’s functioning in everyday life and environment and not primarily on treatment and illness. ICF helped to achieve an insight into the distribution and specific details of the stated needs and plans and seemed to have the potential to add to the framework of studies within cancer rehabilitation and needs assessment.
Being worried was stated as the third largest need, with almost the same proportion among hospital and in primary care patients. This is an issue to be taken into consideration as it can be argued that knowing what the patients’ needs are may help to provide a more targeted rehabilitation service [32]. There is a tendency in rehabilitation services to have an excessive focus on the physical elements of rehabilitation [11], which is known to be effective and beneficial with regard to many parameters [4-6, 13], but the fact that one-third of the patients stated being worried as a need should indicate an essential need for aiming rehabilitation interventions towards this need for psychological support as well.
A limitation in the study is the two different patient populations, both hospital patients and primary care patients. Including a bigger sample from for example different wards would have improved our comparison between the patients. Nevertheless, irrespective of the disease, the setting (hospital or primary care), etc., the distribution of rehabilitation needs and plans appeared to be quite similar in the two groups, and this is in line with previous research findings [13, 30].
Another limitation is that in only 188 out of 933 patients was there documented use of a needs assessment form during the study period. In all, 724 patients did not complete the needs assessment form. We have no information on these patients, and it is not possible to test whether they differed from the included patients. In primary care, we reckon that it is only the patients with needs that complete an assessment form. It is not possible to know which patients completing an assessment at the hospital actually participated in primary care rehabilitation and moreover, it is not possible to test whether a rehabilitation plan is important for participating and completing a programme.
Conclusion
This is the first study to investigate and describe survivorship care and rehabilitation needs and plans as stated by patients with cancer both when diagnosed at hospitals and when rehabilitation in primary care begins. The rate of implementation of needs assessment was very low, even though all sectors in the healthcare system have an obligation to identify cancer patients’ needs. The results underpin an urgent need for a systematic procedure on the assessment of needs in clinical practice. Gaining knowledge on needs assessment and the specific details of needs and plans facilitates targeted survivorship care and rehabilitation interventions. Future studies should focus on needs assessment within cancer rehabilitation in both hospital and primary care settings in order to develop validated needs assessment tools that have been formulated by both patients and healthcare professionals.
Relevance to clinical practice
Knowing that cancer survivorship and rehabilitation is effective (from the time of diagnosis) makes is pressing to adapt a culture with systematically identifying exposed cancer patients needs for survivorship care and rehabilitation support.
The findings indicate an urgent need to be formalized and systematic in screening, addressing and identifying which cancer patients are in need of survivorship care and rehabilitation both at hospitals and in primary care.
The findings indicate that there should be focus on making a contribution to considering the development of a new needs assessment form with involvement of both patients and healthcare professionals.
Cooperation across sectors (hospitals and primary care settings) seems prerequisite in order to ensure a seamless trajectory for exposed cancer patients - ensuring them with the best possible help and support.
Acknowledgments
Special thanks to all the patients and their healthcare professionals who participated and helped in making this study possible. We also want to thank the management at the hospitals and primary care settings for their generous contribution and kind assistance. This study was supported by the foundation “Folkesundhed i Midten”, Denmark.
Conflicts of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
| References | ▴Top |
- Moustsen IR, Larsen SB, Vibe-Petersen J, Trier K, Bidstrup PE, Andersen KK, Johansen C, et al. Social position and referral to rehabilitation among cancer patients. Acta Oncol. 2015;54(5):720-726.
doi - Holm LV, Hansen DG, Larsen PV, Johansen C, Vedsted P, Bergholdt SH, Kragstrup J, et al. Social inequality in cancer rehabilitation: a population-based cohort study. Acta Oncol. 2013;52(2):410-422.
doi pubmed - Pearson EJ, Twigg VJ. A framework for rehabilitation for cancer survivors. Eur J Cancer Care (Engl). 2013;22(6):701-708.
doi pubmed - de Leeuw J, Larsson M. Nurse-led follow-up care for cancer patients: what is known and what is needed. Support Care Cancer. 2013;21(9):2643-2649.
doi pubmed - Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733-742.
doi pubmed - Armes J, Crowe M, Colbourne L, Morgan H, Murrells T, Oakley C, Palmer N, et al. Patients' supportive care needs beyond the end of cancer treatment: a prospective, longitudinal survey. J Clin Oncol. 2009;27(36):6172-6179.
doi pubmed - Gronvold M. The cancer patient's world - a study of Danish cancer patients' needs - results, assessments and proposals. [Kraeftpatientens verden: En undersoegelse af hvad danske kraeftpatienter har brug for]. The Danish Cancer Society [Kraeftens Bekaempelse]. 2006.
- Holm LV, Hansen DG, Kragstrup J, Johansen C, Christensen R, Vedsted P, Sondergaard J. Influence of comorbidity on cancer patients' rehabilitation needs, participation in rehabilitation activities and unmet needs: a population-based cohort study. Support Care Cancer. 2014;22(8):2095-2105.
doi pubmed - Jansen F, van Uden-Kraan CF, van Zwieten V, Witte BI, Verdonck-de Leeuw IM. Cancer survivors' perceived need for supportive care and their attitude towards self-management and eHealth. Support Care Cancer. 2015;23(6):1679-1688.
doi pubmed - Thorsen L, Gjerset GM, Loge JH, Kiserud CE, Skovlund E, Flotten T, Fossa SD. Cancer patients' needs for rehabilitation services. Acta Oncol. 2011;50(2):212-222.
doi pubmed - The Danish Cancer Society [Kraeftens Bekaempelse]. From knowledge to action in cancer rehabilitation - Report from a National task group [Fra viden til handling i rehabiliteringsindsatsen i forbindelse med kraeft - Rapport fra en national arbejdsgruppe]. 2015.
- Alfano CM, Ganz PA, Rowland JH, Hahn EE. Cancer survivorship and cancer rehabilitation: revitalizing the link. J Clin Oncol. 2012;30(9):904-906.
doi pubmed - Hansen DG, Larsen PV, Holm LV, Rottmann N, Bergholdt SH, Sondergaard J. Association between unmet needs and quality of life of cancer patients: a population-based study. Acta Oncol. 2013;52(2):391-399.
doi pubmed - Veloso AG, Sperling C, Holm LV, Nicolaisen A, Rottmann N, Thayssen S, Christensen RD, et al. Unmet needs in cancer rehabilitation during the early cancer trajectory--a nationwide patient survey. Acta Oncol. 2013;52(2):372-381.
doi pubmed - Holm LV, Hansen DG, Johansen C, Vedsted P, Larsen PV, Kragstrup J, Sondergaard J. Participation in cancer rehabilitation and unmet needs: a population-based cohort study. Support Care Cancer. 2012;20(11):2913-2924.
doi pubmed - LeBlanc MR. Oncology nurses need to get serious about cancer rehabilitation. Clin J Oncol Nurs. 2015;19(5):500.
doi pubmed - Danish Health and Medicines Authority. Disease management program for rehabilitation and palliation in cancer: part of the overall disease management program for cancer [Forloebsprogram for rehabilitering og palliation i forbindelse med kraeft]. 2012.
- Ganz PA. Survivorship: adult cancer survivors. Prim Care. 2009;36(4):721-741.
doi pubmed - von Heymann-Horan AB, Dalton SO, Dziekanska A, Christensen J, Andersen I, Mertz BG, Olsen MH, et al. Unmet needs of women with breast cancer during and after primary treatment: a prospective study in Denmark. Acta Oncol. 2013;52(2):382-390.
doi pubmed - Wiedenbein L, Kristiansen M, Adamsen L, Hjort D, Hendriksen C. Assessment of rehabilitation needs in colorectal cancer treatment: Results from a mixed audit and qualitative study in Denmark. Acta Oncol. 2016;55(6):705-711.
doi pubmed - Duijts S, Dalton SO, Lundh MH, Horsboel TA, Johansen C. Cancer survivors and return to work: current knowledge and future research. Psychooncology. 2017;26(5):715-717.
doi pubmed - Horsboel TA, Nielsen CV, Andersen NT, Nielsen B, de Thurah A. Risk of disability pension for patients diagnosed with haematological malignancies: a register-based cohort study. Acta Oncol. 2014;53(6):724-734.
doi pubmed - Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustun B, Stucki G. ICF linking rules: an update based on lessons learned. J Rehabil Med. 2005;37(4):212-218.
doi pubmed - Bayly JL, Lloyd-Williams M. Identifying functional impairment and rehabilitation needs in patients newly diagnosed with inoperable lung cancer: a structured literature review. Support Care Cancer. 2016;24(5):2359-2379.
doi pubmed - Kim YM, Kim DY, Chun MH, Jeon JY, Yun GJ, Lee MS. Cancer rehabilitation: experience, symptoms, and needs. J Korean Med Sci. 2011;26(5):619-624.
doi pubmed - The Danish Cancer Society [Kreftens Bekempelse]. Strategic Presentation on Cancer Rehabilitation [Strategisk Opleg om kreftrehabilitering]. 2010.
- Close Health Offers, Strategy and Planning, Central Denmark Region [Naere Sundhedstilbud, Strategi og Planlaegning, Region Midtjylland]. Health Agreement for rehabilitation of cancer, Health Agreement 2015-2018, Regional guideline [Sundhedsaftale om rehabilitering i forbindelse med kraeft, Sundhedsaftale 2015-2018, Regional retningslinje]. 2015.
- Handberg C, Midtgaard J, Nielsen CV, Thorne S, Lomborg K. Healthcare professionals' attitudes to rehabilitation programming for male cancer survivors. Rehabil Nurs. 2016.
doi pubmed - Handberg C, Beedholm K, Bregnballe V, Nellemann AN, Seibaek L. Reflections on patient involvement in research and clinical practice: A secondary analysis of women's perceptions and experiences of egg aspiration in fertility treatment. Nurs Inq. 2017.
doi pubmed - Takeuchi EE, Keding A, Awad N, Hofmann U, Campbell LJ, Selby PJ, Brown JM, et al. Impact of patient-reported outcomes in oncology: a longitudinal analysis of patient-physician communication. J Clin Oncol. 2011;29(21):2910-2917.
doi pubmed - Maribo T, Petersen KS, Handberg C, Melchiorsen H, Momsen AM, Nielsen CV, Leonardi M, et al. Systematic literature review on ICF from 2001 to 2013 in the nordic countries focusing on clinical and rehabilitation context. J Clin Med Res. 2016;8(1):1-9.
doi pubmed - Johansen C, Dalton SO. Survivorship - searching for new directions. Acta Oncol. 2015;54(5):569-573.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


