| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Case Report
Volume 1, Number 1, April 2009, pages 56-57
Chronic Non-Exertional Myalgia and Myoadenylate Deaminase Deficiency: a Possible Association
Aiesha Ahmeda, b, Max R Lowdena
aPenn State College of Medicine, Hershey Medical Center, Department of Neurology - EC037, 30 Hope Drive, Hershey, PA 17033, USA
bCorresponding author: E-mail:
Manuscript accepted for publication April 07, 2009
Short title: Myoadenylate Deaminase Deficiency
doi: https://doi.org/10.4021/jocmr2009.04.1231
| Abstract | ▴Top |
Myoadenylate deaminase deficiency is noted in skeletal muscles. It generally presents with exertional myalgias, fatigue and weakness. We present a patient who complained of constant pain unrelated to activity with biopsy finding consistent of myoadenylate deaminase deficiency.
Keywords: Myoadenylate deaminase deficiency; Myalgia; Pain
| Introduction | ▴Top |
Myoadenylate deaminase catalyses the deamination of adenosine monophosphate to inosine monophosphate to release energy during muscle activity [1]. Myoadenylate deaminase deficiency is noted in skeletal muscles of 2-3% of patients with neuromuscular disorders [2]. Different isoforms are present in skeletal and smooth muscles, nerve bundles as well as in endothelial cells [3]. Clinical presentation is usually exertional myalgia and fatigue. We report a patient with biopsy proven myoadenylate deaminase deficiency which did not present with the usual exertion related muscle pain.
| Case Report | ▴Top |
A 46-year-old white man presented to the neuromuscular clinic with generalized muscle pain, fatigue and cramps for 10-15 years. The muscle pain was described as constant, dull and achy. It was present during rest and was unchanged by exercise. There were no paresthesias, fever, swollen joints, rashes, or dark urine but the patient did admit to generalized weakness.
The patient had a past medical history of spontaneous pneumothoraces and hypercholesterolemia. Family history reveals no neuromuscular diseases. Interventions including physical therapy, aquatherapy, tizanidine, tricyclic antidepressants, and nonsteroidal anti-inflammatory drugs provided minimal relief.
On physical examination, he had intact muscle bulk, strength and tone throughout. His muscle stretch reflexes were normal. The remainder of the neurological examination was normal. Evaluations including blood work for connective tissue disorders, chemistry, thyroid studies, creatine phosphokinase and electrodiagnostic studies which failed to identify an etiology for his complaints.
A muscle biopsy of the left vastus lateralis was performed in light of persistent symptomatology. It showed mild morphologic abnormalities consistent with variation in myofiber size and shape (Fig. 1). Myofiber glycogen content and staining for phosphorylase, phosphofructokinase, and acid phosphatase were unrevealing. Staining for myoadenylate deaminase activity was markedly diminished (Fig. 2). Biochemical analyses for acid maltase, fatty acid transport (carnitine, carnitine palmitoyltransferase) and mitochondrial enzymes including respiratory chain enzymes were unremarkable.
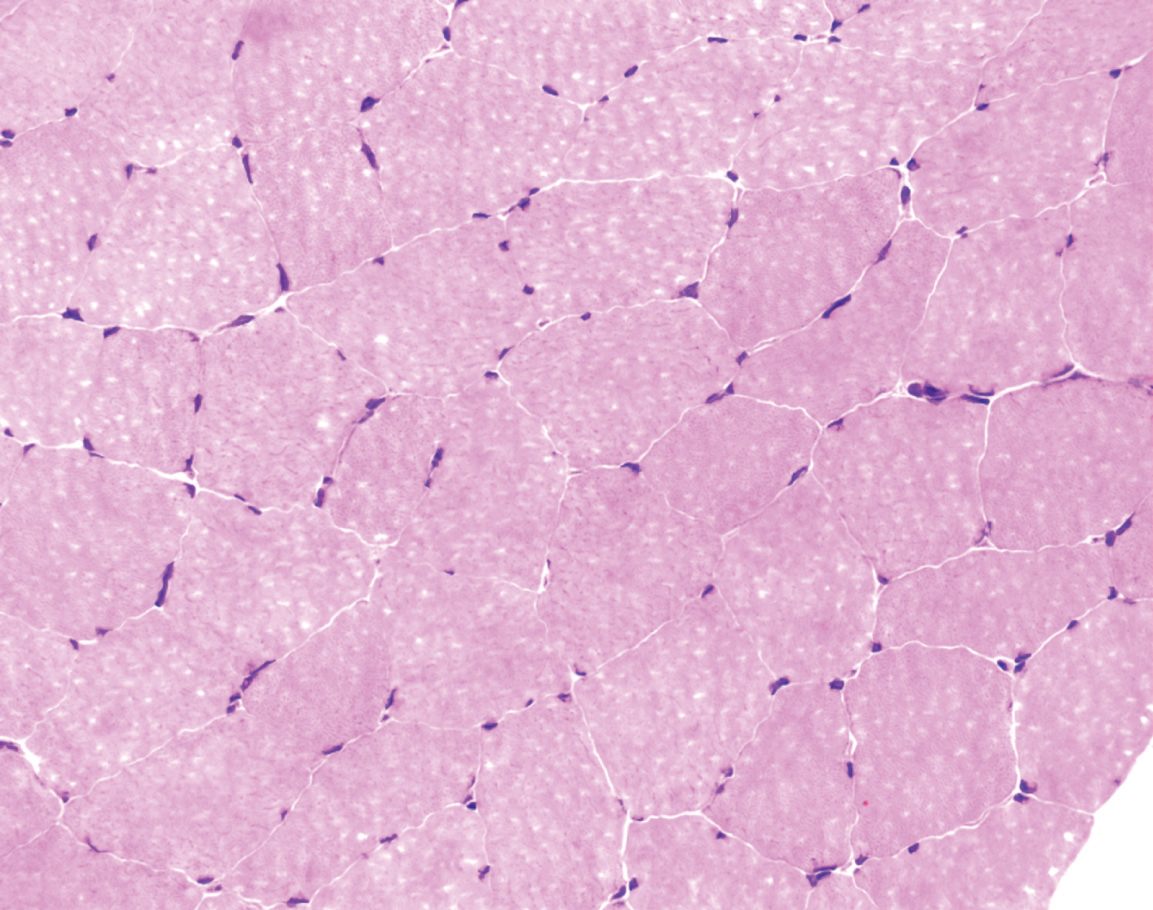 Click for large image | Figure 1. Hematoxylin and eosin stain of muscle showing mild variation in myofiber size and shape but overall preservation of normal morphology as typically seen in myoadenylate deaminase deficiency. x 400. |
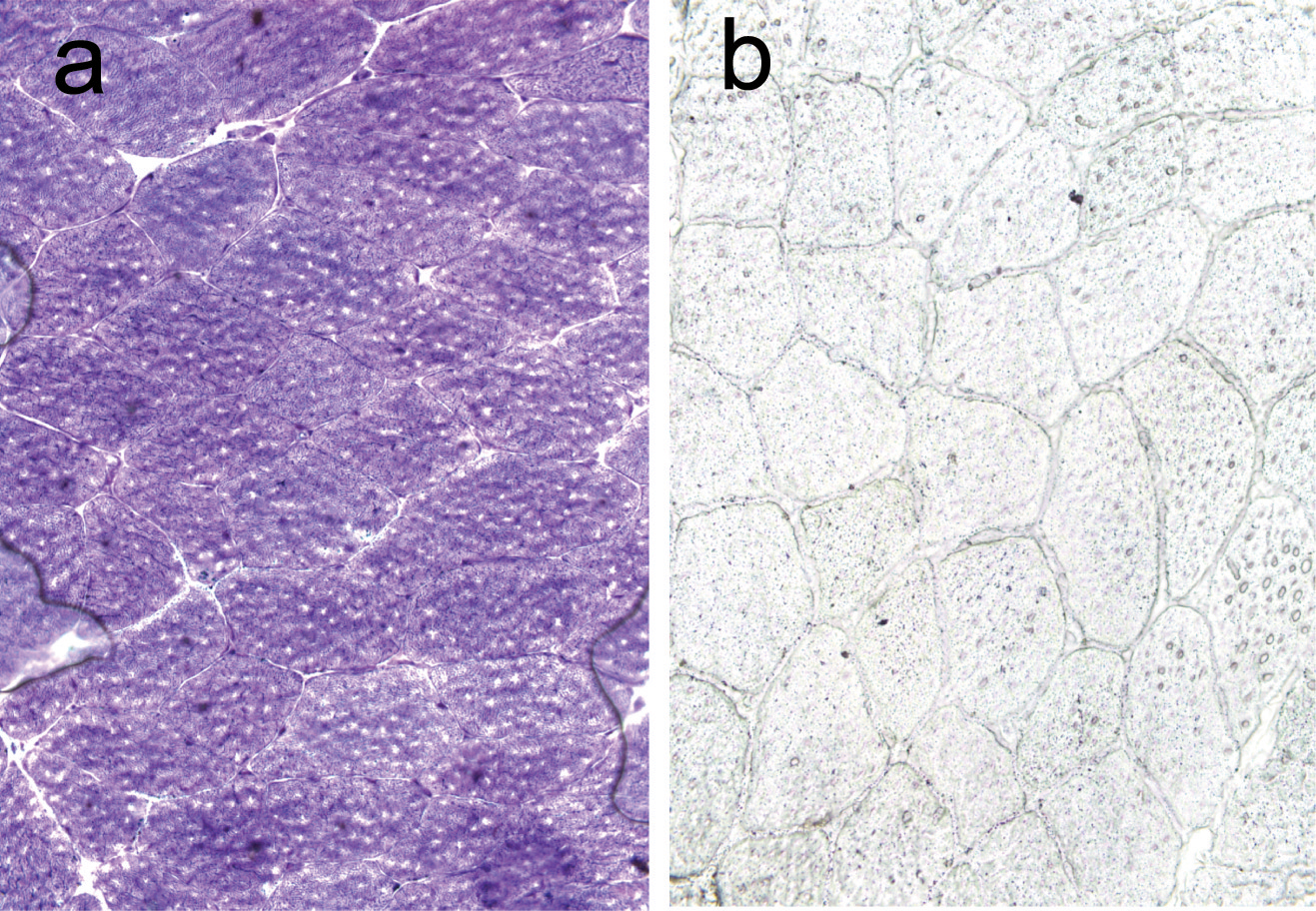 Click for large image | Figure 2. Adenosine monophosphate deaminase stain of muscle showing normal control (a) and markedly diminished myoadenylate deaminase activity (b). x 400. |
| Discussion | ▴Top |
Exertional myalgia is seen with myoadenylate deaminase deficiency in most of the reported cases [4-7], along with fatigue and weakness. We present a case of longstanding constant pain which was not triggered by exertion. We found a few reports of resting pain in patients with myoadenylate deaminase deficiency, however these patients developed it either subsequent to having exertional mylagia for some time [3] or the pain was minimal at rest and would worsen on exertion [8].
In summary, our patient's presentation of constant mylagias in the absence of laboratory work up suggesting a neuromuscular disorder other than biopsy proven myoadenylate deaminase deficiency is unusual. Investigations for connective tissue disorder, infections and malignancy were also unremarkable. We approached muscle biopsy as a last step to exclude all possibilities. The biopsy results showing remarkable absence of myoadenylate deaminase bring ups the question that this deficiency may be associated with symptoms of constant pain. We suggest that chronic constant myalgias should be considered as a possible uncommon presentation for myoadenylate deaminase deficiency and good clinical judgment and exclusion of other etiologies should be undertaken.
Conflict of Interest
The authors declare no conflicts of interest.
| References | ▴Top |
- Riggs JE, Schochet SS, Jr., Webb RW. Exertional myalgia syndrome associated with diminished serum ammonia elevation in ischemic exercise testing. Mil Med. 1999;164(9):663-665.
pubmed - Shumate JB, Katnik R, Ruiz M, Kaiser K, Frieden C, Brooke MH, Carroll JE. Myoadenylate deaminase deficiency. Muscle Nerve. 1979;2(3):213-216.
pubmed - Marin R, Connick E. Tension myalgia versus myoadenylate deaminase deficiency: a case report. Arch Phys Med Rehabil. 1997;78(1):95-97.
pubmed - Hayes DJ, Summers BA, Morgan-Hughes JA. Myoadenylate deaminase deficiency or not? Observations on two brothers with exercise-induced muscle pain. J Neurol Sci. 1982;53(1):125-136.
pubmed - Kelemen J, Rice DR, Bradley WG, Munsat TL, DiMauro S, Hogan EL. Familial myoadenylate deaminase deficiency and exertional myalgia. Neurology. 1982;32(8):857-863.
pubmed - Rossi LN, Cornelio F, Dworzak F, Morandi L, Rossi G, Di Mauro S. Myoadenylate deaminase deficiency in a 5-year-old boy with intermittent muscle pain. Helv Paediatr Acta. 1984;39(1):89-93.
pubmed - Sinkeler SP, Wevers RA, Joosten EM, Binkhorst RA, Oei LT, Van't Hof MA, De Haan AF. Improvement of screening in exertional myalgia with a standardized ischemic forearm test. Muscle Nerve. 1986;9(8):731-737.
pubmed - Lally EV, Friedman JH, Kaplan SR. Progressive myalgias and polyarthralgias in a patient with myoadenylate deaminase deficiency. Arthritis Rheum. 1985;28(11):1298-1302.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


