| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 15, Number 3, March 2023, pages 161-165
Predictive Factors for the Necessity of Hospitalization of Patients With Acute Alcohol Intoxication
Hiroaki Takeokaa, b, c, Ken Horibataa, b, Shinta Masuia, Hiroki Suzuyamaa, Kazuhiko Ajisakaa, Shigeki Nabeshimaa
aGeneral Medicine, Fukuoka University Hospital, 7-45-1 Nanakuma, Jonan-ku, Fukuoka 814-0180, Japan
bThese authors contributed equally to this article.
cCorresponding Author: Hiroaki Takeoka, General Medicine, Fukuoka University Hospital, 7-45-1 Nanakuma, Jonan-ku, Fukuoka 814-0180, Japan
Manuscript submitted February 4, 2023, accepted March 3, 2023, published online March 28, 2023
Short title: Acute Alcohol Intoxication and Hospitalization
doi: https://doi.org/10.14740/jocmr4881
| Abstract | ▴Top |
Background: The aim of the study was to identify factors related to the need for hospitalization due to acute alcohol intoxication.
Methods: The data of 42 patients with acute alcohol intoxication who visited our hospital from April 1, 2014 to September 30, 2015 were available for analysis. Factors related to outcome included hospitalization or release to home, Glasgow coma scale (GCS), temperature, pulse rate, blood pressure, oxygen saturation of the peripheral artery (SpO2), and respiratory rate. A retrospective survey was done that included estimated blood alcohol concentration, osmotic pressure, and serum lactate level. The following formula was used to estimate blood alcohol concentration: (measured osmotic pressure - estimated osmotic pressure × 4.6 mg/dL). Univariate analysis of each variable was done for the two outcome groups, hospital admission or release to home, then statistically significant items were subjected to multivariate analysis.
Results: Of the 42 patients (average age 22.8 ± 8.6 years, 33 men, six women), 29 were admitted and 13 were released to home. There was a weak correlation between estimated blood alcohol concentration and GCS. There was no significant difference in alcohol concentration or GCS between the hospitalized and released to home groups. In multivariate analysis using the outcome as the objective variable, a serum lactate level of 26 mg/dL or higher was associated with the need for hospitalization (odds ratio: 6.7).
Conclusion: A serum lactate level of 26 mg/dL would be useful for deciding if hospitalization is necessary for patients with acute alcohol intoxication.
Keywords: Alcohol intoxication; Serum lactate level; Hospitalization
| Introduction | ▴Top |
Emergency department (ED) visits for acute alcohol intoxication are common [1-4]. Most are mild cases, but sometimes severe cases are experienced. Although often the estimated alcohol concentration is related to the level of consciousness, other causes must be considered if there is dissociation between the estimated alcohol concentration and the symptoms. Some patients have strong symptoms even with a low estimated alcohol concentration, and a decision on admission or release to home can be difficult in cases with few symptoms despite a high estimated alcohol concentration. Previous studies have shown that the blood alcohol level is not directly associated or correlated with severity or consciousness disorder [5].
The serum lactate level has become an important prognostic indicator for patients receiving emergency treatment [6]. Blood lactate is an anaerobic metabolite that reflects the severity of the disease state and that can be used as an index of circulatory and respiratory failure. In particular, it is a useful index for predicting the outcome from changes over time and determining the therapeutic effect [7, 8].
During heavy drinking, the nicotinamide adenine dinucleotide oxidized/reduced (NADH/NAD+) ratio increases due to the metabolism of ethanol. An increased NADH/NAD + ratio also promotes conversion of pyruvic acid to lactate, which tends to accompany hyperlacticacidemia [9]. It has been reported that the lactic acid level does not fluctuate significantly between venous blood and arterial blood, making it easy to test [10]. The plasma lactate level has been reported to be an independent prognostic factor for drug overdose patients [11], and we hypothesized that it might also be useful for monitoring excessive alcohol consumption. In previous reports [12], alcoholic liver damage caused by chronic alcohol intake was associated with elevated lactate. A recent report [13] found that alcohol intake contributed to an increase in lactic acid, regardless of disease.
Even if Glasgow coma scale (GCS) is bad when intoxicated patients arrive at the hospital, some people will eventually recover by intravenous drip, while others will need to be hospitalized and may not wake up for hours; thus, the lactate level might be a useful index for determining the need for hospitalization of patients in a drunken stupor.
This paper was done to identify factors other than the level of consciousness and blood alcohol level on arrival that would be useful for determining the severity and for predicting the necessity of hospitalization of patients with acute alcohol intoxication.
| Materials and Methods | ▴Top |
Subjects
This was a retrospective review of the data of patients who were transported to Fukuoka University Hospital by ambulance because of acute alcohol intoxication between April 2014 and September 2015. Of the 42 patients, 29 were hospitalized and 13 were released to home. The decision to admit the patient to the hospital depended on the examining physician. Blood tests were performed upon arrival at the emergency room. Data on the following clinical items were collected: age, sex, outcome in terms of hospitalization or release to home, GCS, body temperature, pulse rate, blood pressure, SpO2, respiratory rate, estimated alcohol concentration, and serum lactate (mg/dL × 0.11101 = mmol/L). For the calculation of estimated alcohol concentration, the formula “(measured osmotic pressure - estimated osmotic pressure) × 4.6 mg/dL” was used. In addition, patients who presented with other conditions, for example, shock, bacterial infection, disseminated intravascular coagulopathy, diabetes mellitus, or liver failure that might affect plasma lactate concentration were excluded. This study was conducted in compliance with the ethical standards for human subjects and the Declaration of Helsinki and was approved by the Institutional Review Board of Fukuoka University Hospital (Reference No. 16-8-12).
Statistical analysis
All statistical analyses were performed with EZR [14], a modified version of R commander designed to add statistical functions frequently used in biostatistics. We regarded P < 0.05 as statistically significant. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Univariate analysis was done with all variables to determine differences between the hospitalized and released to home groups. Multivariate logistic regression analysis was done with body temperature, respiratory rate, and lactate as explanatory variables and hospitalization or release to home as objective variables. The discriminative ability of the multivariate model was evaluated by receiver operating characteristic (ROC) curve. Cutoff values were set with “hospitalization or release to home” as the objective variable and “serum lactate level”, “respiratory rate”, “body temperature”, and “blood pressure” as the explanatory variables. The sensitivity, specificity, and likelihood ratio of the identified independent variables were calculated.
| Results | ▴Top |
Figure 1 shows the relation between GCS and the estimated alcohol concentration at the time of the emergency visit. Estimated alcohol concentration and GCS had a weak negative correlation (correlation coefficient minus 0.42). Our results also showed a decrease in the level of consciousness when the estimated alcohol concentration was from 160 to 200 mg/dL.
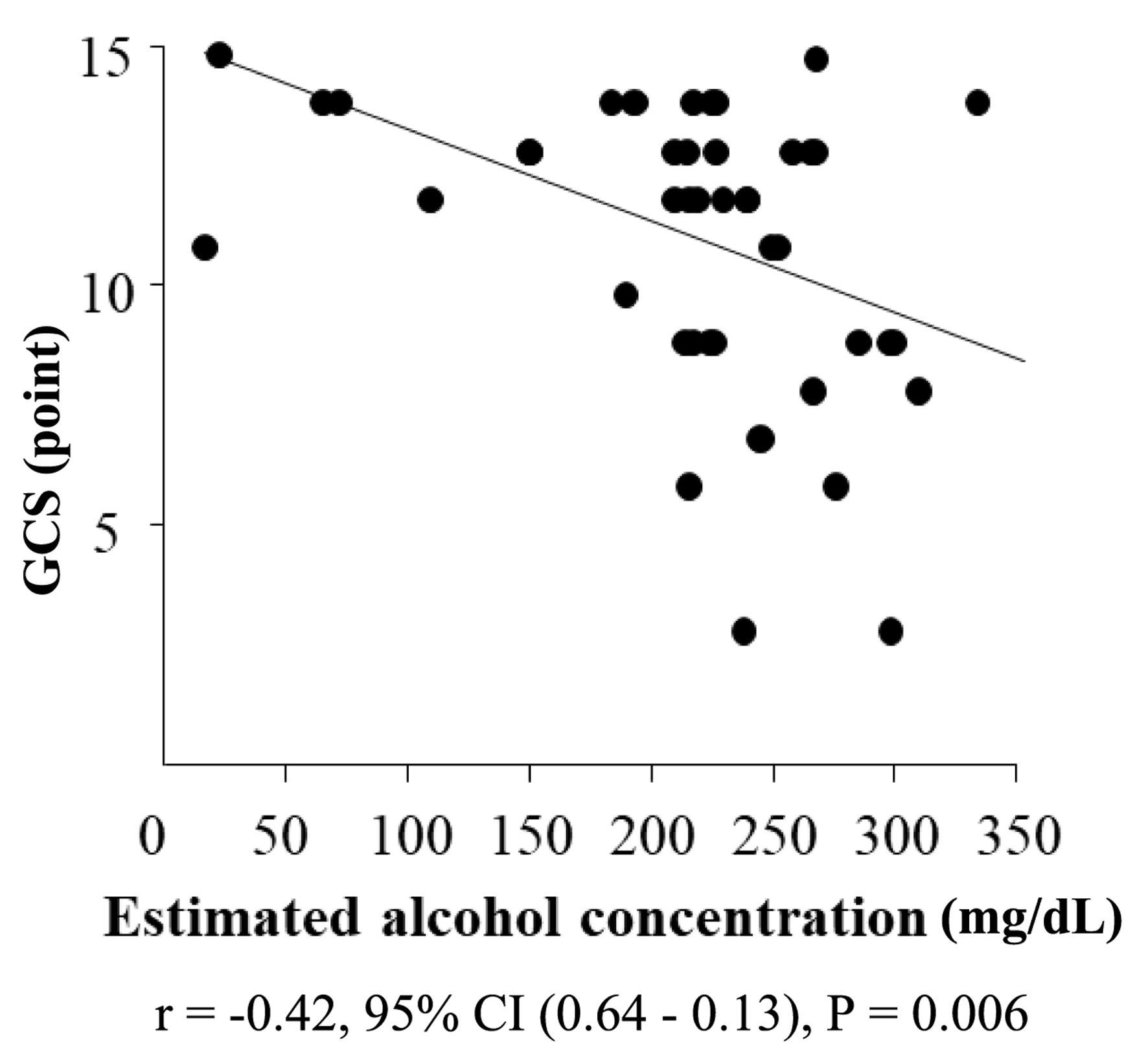 Click for large image | Figure 1. Relation between GCS and estimated alcohol concentration at the time of the emergency visit. Analysis of the estimated alcohol concentration and GCS showed a weak negative correlation coefficient of 0.42. GCS: Glasgow coma scale. |
Table 1 shows a comparison of the hospitalized and released to home groups for each background factor. There was no significant difference in GCS or estimated alcohol concentration, but there were significant differences in age, body temperature, respiratory rate, and serum lactate level. The age of the patients was concentrated around 20 years.
 Click to view | Table 1. Clinical Characteristics |
Table 2 shows the results of multivariate analysis. The only factor extracted that was related to the necessity of hospitalization was the serum lactate level. When the serum lactate level was 26.0 mg/dL (2.9 mmol/L) or higher, the patient was hospitalized 6.67 times more often than if the level was lower than 26.0 mg/dL (2.9 mmol/L).
 Click to view | Table 2. Multivariate Analysis of Factors Related to Acute Alcohol Intoxication |
Table 3 is a summary of the characteristics of diagnostic prediction in cases where a serum lactate level of 26.0 mg/dL (2.9 mmol/L) or more was indicated for hospitalization. The sensitivity was 0.769 and the specificity was 0.667.
 Click to view | Table 3. Accuracy of a Serum Lactate Level of 26 mg/dL or Over as a Predictor of Hospitalization |
| Discussion | ▴Top |
This is the first study to show that the serum lactate level is useful for predicting the need for hospitalization due to acute alcoholism intoxication.
Studies of alcohol concentration and disturbance of consciousness have related 100 mg/dL to impaired judgment, 200 mg/dL to amnesia, and 400 mg/dL to respiratory depression and coma [15]. Although we found weak correlations, as shown in Figure 1, we were unable to show accurate correlations or to evaluate these data because the distributions were too diverse. In addition, the consciousness level of patients with alcohol intoxication can be easily changed by the appropriate hydration.
The most common cause of elevated blood lactate, in general, is circulatory shock. Acute or chronic alcohol abuse predisposes a person to sepsis, gastrointestinal hemorrhage, pancreatitis, and other disorders that can lead to shock. In emergency medicine, lactic acid is a useful metabolite of anaerobic glycolysis. It is used as an index to the severity of peripheral circulatory insufficiency, such as shock. We hypothesized that the serum lactate level might also be a useful marker as an index of the need for hospitalization for acute alcohol intoxication. In our study, lactate levels were measured in venous blood. A previous study reported that the lactate level of venous blood was increased 1.7 times after drinking alcohol [13], and ethanol intoxication was associated with a higher lactate level (mean difference: 0.69 mmol/L; 95% CI, 0.11 to 1.27 mmol/L) [16]. A blood lactate concentration in excess of 45 mg/dL (5 mmol/L) on intensive care unit admission was associated with 3- and 30-day mortality rates of 59% and 83%, respectively [17]. Acute alcoholism may result in hospitalization due to social problems, slow awakening, or violent behavior. We found that an increase in lactate was useful for determining the needed hospitalization or release. The increase in the lactic acid level in acute alcohol intoxication is due to the effect of alcohol decomposition, a decrease in tissue perfusion due to dehydration, and increases in anaerobic metabolism and pyruvate. Hospitalization is necessary when there is heavy alcohol consumption over a short period of time and dehydration. Severe lactic acidosis usually has a poor prognosis [18]. Plasma lactate concentrations were reported to be significantly higher than normal in patients who have recently consumed alcohol, even in patients without conditions known to increase lactate concentration [13].
Another important consideration in Japan is that acute alcohol intoxication tends to be common among young people [19]. There are reports [20] that education on alcoholism shapes the environmental impact of alcohol use, thus more such intervention is necessary in Japan.
This study has several limitations. The first is the small number of cases, but the results provide a basis for more in-depth study. Second, the weak correlation of GCS may be because it is a calculated value rather than a direct measurement of alcohol concentration. Third, no hospital wide guidelines presenting criteria for hospitalizing a patient were in place at the time of the study. Lastly, this is a cross-sectional study, thus future prospective studies are needed.
Conclusion
We found that a serum lactate level of 26.0 mg/dL (2.9 mmol/L) or higher would be useful for predicting the necessity for hospitalization due to acute alcohol intoxication.
Acknowledgments
None to declare.
Financial Disclosure
There was no specific funding source for this research.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
All subjects provided written informed consent.
Author Contributions
Drs. Takeoka and Horibata were the lead researchers and analyzed the data. Drs. Masui, Suzuyama, and Ajisaka examined and treated the patients. Dr. Nabeshima supervised and helped design the study.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Mullins PM, Mazer-Amirshahi M, Pines JM. Alcohol-related visits to US emergency departments, 2001-2011. Alcohol Alcohol. 2017;52(1):119-125.
doi - Verelst S, Moonen PJ, Desruelles D, Gillet JB. Emergency department visits due to alcohol intoxication: characteristics of patients and impact on the emergency room. Alcohol Alcohol. 2012;47(4):433-438.
doi - Pletcher MJ, Maselli J, Gonzales R. Uncomplicated alcohol intoxication in the emergency department: an analysis of the National Hospital Ambulatory Medical Care Survey. Am J Med. 2004;117(11):863-867.
doi - Piccioni A, Cicchinelli S, Saviano L, Gilardi E, Zanza C, Brigida M, Tullo G, et al. Risk Management in First Aid for Acute Drug Intoxication. Int J Environ Res Public Health. 2020;17(21):8021.
doi pubmed pmc - Sullivan JB, Jr., Hauptman M, Bronstein AC. Lack of observable intoxication in humans with high plasma alcohol concentrations. J Forensic Sci. 1987;32(6):1660-1665.
doi - Andersen LW, Mackenhauer J, Roberts JC, Berg KM, Cocchi MN, Donnino MW. Etiology and therapeutic approach to elevated lactate levels. Mayo Clin Proc. 2013;88(10):1127-1140.
doi pubmed pmc - Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-810.
doi pubmed pmc - Freund Y, Delerme S, Goulet H, Bernard M, Riou B, Hausfater P. Serum lactate and procalcitonin measurements in emergency room for the diagnosis and risk-stratification of patients with suspected infection. Biomarkers. 2012;17(7):590-596.
doi - Umpierrez GE, DiGirolamo M, Tuvlin JA, Isaacs SD, Bhoola SM, Kokko JP. Differences in metabolic and hormonal milieu in diabetic- and alcohol-induced ketoacidosis. J Crit Care. 2000;15(2):52-59.
doi - Datta D, Grahamslaw J, Gray AJ, Graham C, Walker CA. Lactate - Arterial and Venous Agreement in Sepsis: a prospective observational study. Eur J Emerg Med. 2018;25(2):85-91.
- Tarui T, Yoshikawa K, Miyakuni Y, Kaita Y, Tamada N, Matsuda T, Miyauchi H, et al. Independent risk factors for a complicated hospital course in intensive care unit overdose patients. Acute Med Surg. 2015;2(2):98-104.
doi pubmed pmc - Fulop M, Bock J, Ben-Ezra J, Antony M, Danzig J, Gage JS. Plasma lactate and 3-hydroxybutyrate levels in patients with acute ethanol intoxication. Am J Med. 1986;80(2):191-194.
doi - Sonoo T, Iwai S, Inokuchi R, Gunshin M, Nakajima S, Yahagi N. Quantitative analysis of high plasma lactate concentration in ED patients after alcohol intake. Am J Emerg Med. 2016;34(5):825-829.
doi - Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48(3):452-458.
doi pubmed pmc - Vonghia L, Leggio L, Ferrulli A, Bertini M, Gasbarrini G, Addolorato G, Alcoholism Treatment Study Group. Acute alcohol intoxication. Eur J Intern Med. 2008;19(8):561-567.
doi - Zehtabchi S, Sinert R, Baron BJ, Paladino L, Yadav K. Does ethanol explain the acidosis commonly seen in ethanol-intoxicated patients? Clin Toxicol (Phila). 2005;43(3):161-166.
doi - Stacpoole PW, Wright EC, Baumgartner TG, Bersin RM, Buchalter S, Curry SH, Duncan C, et al. Natural history and course of acquired lactic acidosis in adults. DCA-Lactic Acidosis Study Group. Am J Med. 1994;97(1):47-54.
doi - Lien D, Mader TJ. Survival from profound alcohol-related lactic acidosis. J Emerg Med. 1999;17(5):841-846.
doi - Yoshimoto H, Takayashiki A, Goto R, Saito G, Kawaida K, Hieda R, Kataoka Y, et al. Association between excessive alcohol use and alcohol-related injuries in college students: a multi-center cross-sectional study in Japan. Tohoku J Exp Med. 2017;242(2):157-163.
doi - Barr PB, Salvatore JE, Maes H, Aliev F, Latvala A, Viken R, Rose RJ, et al. Education and alcohol use: A study of gene-environment interaction in young adulthood. Soc Sci Med. 2016;162:158-167.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


