| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 10, October 2022, pages 400-408
Patient Portal Use Among Diabetic Patients With Different Races and Ethnicities
Hao Wanga, c , Ryan Kirbya, Aimee Piercea, Michael Barbaroa, Amy F. Hoa, Jake Blalockb, Chet D. Schradera
aDepartment of Emergency Medicine, JPS Health Network, Fort Worth, TX 76104, USA
bTCU and UNTHSC School of Medicine, Fort Worth, TX 76107, USA
cCorresponding Author: Hao Wang, Department of Emergency Medicine, John Peter Smith Health Network, Fort Worth, TX 76104, USA
Manuscript submitted September 3, 2022, accepted October 13, 2022, published online October 28, 2022
Short title: Patient Portal and Diabetes
doi: https://doi.org/10.14740/jocmr4822
| Abstract | ▴Top |
Background: Patient portal (PP) use varies among different patient populations, specifically among those with diabetes mellitus (DM). In addition, it is still uncertain whether PP use could be linked to improved clinical outcomes. Therefore, the aim of this paper was to determine PP use status for patients, recognize factors promoting PP use, and further identify the association between PP use and clinical outcome among diabetic patients of different races and ethnicities.
Methods: This was a single-center cross-section study. Patients were divided into non-Hispanic white (NHW), non-Hispanic black (NHB), and Hispanic/Latino groups. PP use was compared among these three groups. Multivariate logistic regressions were used to determine factors associated with PP use, serum glycemic control, and emergency department (ED) hospitalizations.
Results: A total of 77,977 patients were analyzed. The rate of PP use among patients of NHW (24%) was higher than those of NHB (19%) and Hispanic/Latinos (18%, P < 0.0001). The adjusted odds ratio (AOR) of insurance coverage associated with PP use was 2.12 (2.02 - 2.23, P < 0.0001), and having a primary care physician (PCP) associated with PP use was 3.89 (3.71 - 4.07, P < 0.0001). In terms of clinical outcomes, the AOR of PP use associated with serum glycemic control was 0.98 (0.90 - 1.05, P = 0.547) and ED hospitalization was 0.79 (0.73 - 0.86, P < 0.0001).
Conclusion: PP use disparity occurred among NHB and Hispanic/Latino patients in the ED. Having insurance coverage and PCPs seem to correlate with PP use. PP use did not seem to associate with serum glycemic control among DM patients present in the ED but could possibly reduce patient hospitalizations.
Keywords: Patient portal; Diabetes mellitus; Races; Ethnicities
| Introduction | ▴Top |
Personal health records (PHR) tethered to patient electronic medical records (i.e., patient portals (PPs)) have been introduced to patients for decades [1, 2]. PP has many features and allows patients to have better communication with their healthcare providers, request refills for their medications, and arrange their clinic follow-ups. In short, it is a tool that allows patients to have better patient-healthcare connections [1, 3-5].
In previous reports, PP use has been increasing in recent years among patients with chronic conditions, especially those with diabetes mellitus (DM) [1, 6]. Some studies depict that 32-40% of patients with DM have adopted portal accounts in their healthcare systems [6, 7]. However, the digital divide occurred among patients of different races/ethnicities [8], and studies show that PP usage has not increased evenly across demographics in those with DM [6]. Patients who live in rural areas with low income, and nonwhites with low income were less likely to access their PP [6]. Similarly, non-Hispanic black (NHB) were less likely to register their PP compared to their non-Hispanic white (NHW) counterparts [9]. However, these studies either had relatively small sample sizes; or the populations of different races/ethnicities were not well balanced (e.g., different sample sizes compared among NHW, NHB, or Hispanic/Latinos). Additionally, PP use disparities occurred more often among patients with chronic conditions. Previous studies focused more on the report of their PP use among patients with DM, whereas few studies reported PP use status among patients with other chronic conditions [7, 10, 11]. To address this literature gap, it is necessary to determine PP use status among different races/ethnicities using a well-balanced patient sample in the same healthcare environment. Meanwhile, it is also important to determine PP use status among patients with DM in comparison to those with other chronic conditions.
When reviewing the literature, PP use in those with DM has been linked to improved healthcare outcomes [12, 13]. The use of PP has been significantly associated with better serum glycemic control [6, 14, 15]. Similarly it has been found that patients who use their PP more frequently, and for longer periods of time, are likely to have better clinical outcomes than those who use it less often [16, 17]. PP use for patients with DM who have multiple medical conditions has also been associated with significantly higher rates of outpatient office visits, fewer emergency department (ED) visits, and preventative hospital stays [11]. However, these clinical outcomes have rarely been compared among diabetic patients of different races/ethnicities, especially in an acute care setting.
There are many barriers and facilitators that play a role in PP use [18-20]. Determining the current PP use status among patients of different races/ethnicities and identifying promoting factors of PP use may help patients gain better healthcare connections, improve self-care management of chronic diseases, and eventually improve patient healthcare outcomes [21-23]. Therefore, we aim to determine: 1) the PP use status, 2) the PP use associated with clinical outcomes (serum glycemic control and hospitalization), and 3) potential facilitators of PP use among diabetic patients of different races and ethnicities.
| Materials and Methods | ▴Top |
Study design and setting
This was a single-center retrospective cross-sectional study. The study hospital is a publicly funded hospital with one ED. An electronic medical record (Epic) and a tethered PP (MyChart) have been implemented in the study healthcare system since 2012. All patients within the study healthcare system have access to their MyChart. MyChart has many features similar to other PPs. The main features are: 1) refill medications, 2) check lab and image results, 3) pay healthcare costs, 4) arrange clinical appointments, and 5) communicate with healthcare providers. The hospital ED has annual patient visits of approximately 120,000. The ED has patients of various racial and ethnic backgrounds including approximately one-third of NHW, one-third of NHB, and another third of Hispanic/Latino patients. The study procedure was designed in compliance with the Declaration of Helsinki. This study was approved by the institution’s respective Institutional Review Board with waived informed consent due to its retrospective study and deidentified data (No. 1600198-5).
Study participants
Patients who visited the ED at least once from March 1, 2019 to February 28, 2021 were included. In this study, we intended to determine patient PP use status upon their indexed ED visits. Therefore, we only included patients who had visited the study healthcare system before their indexed ED visits. This would ensure that our participants had access to their PP prior to their indexed ED visits. In addition, if patients had multiple ED encounters during the study period, we only investigated patients’ latest PP status (i.e., all variables were extracted from the last recorded visit during the study period). Patients’ chronic conditions were identified and multimorbidity was defined as the presence of two or more chronic conditions based on Goodman’s criteria [24]. Additionally, this study mainly focused on the comparisons of NHW, NHB, and Hispanic/Latino patient populations. Since our ED patients of other races (e.g., American Native Indian, Alaska Natives, Hawaiian, and other Pacific Islanders, etc.) only accounted for approximately 6% of the entire study cohort, we further excluded those in our final analyses. A detailed study flow of the patient selection is shown in Figure 1.
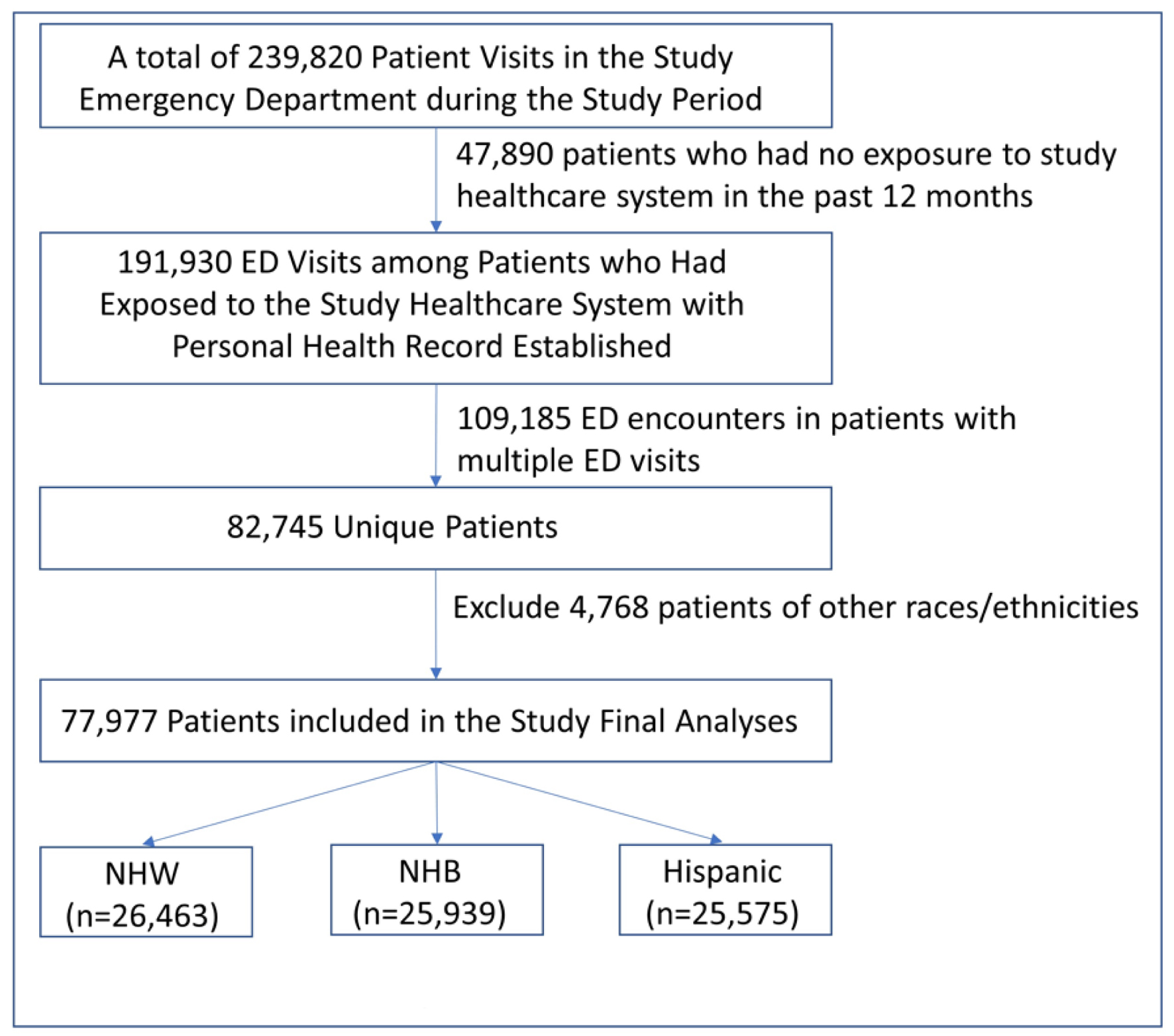 Click for large image | Figure 1. Study flow diagram. |
Variables
Dependent variable
The primary outcome was to determine PP use (yes/no): ED patients who signed on to their MyChart account at least once within 12 months prior to their indexed ED visit were considered positive PP users. If patients did not log on to their MyChart in the past 12 months, we considered them to be negative PP users. Our secondary outcome was to determine DM patient clinical outcomes including serum glycemic control upon patient presenting to the ED triage (i.e., serum glucose level). At ED triage, a serum glucose measurement was performed in patients with a history of DM regardless of their chief complaints. Similarly, if patients were brought in by ambulance, a bedside serum glucose check was also performed on each diabetic patient. Additionally, patient hospitalization was tracked as a secondary outcome.
Key explanatory variables
Patient demographic variables included age, sex (male and female), preferred language (English, Spanish, and others), and race/ethnicity. We divided race/ethnicity into three groups: NHW, NHB, and Hispanic/Latino. In addition, patients’ other healthcare information included insurance status (yes or no), and whether patients had a primary care physician (PCP) (yes or no).
Statistical analyses
Continuous data were summarized as: 1) means ± standard deviation (SD) and compared using analysis of variance (ANOVA); and 2) medians (interquartile ranges (IQRs)) and compared using Wilcoxon rank sum test between groups. Categorical data were summarized by frequencies and percentages and compared using the Chi-squared test among groups. Then, a multivariate logistic regression was performed to determine the association between different races/ethnicities and PP use, and further identify factors promoting PP use. Similarly, the associations of PP use and serum glycemic control and hospitalizations were also analyzed using multivariate logistic regression models. All these logistic regressions were analyzed with the adjustment of patient age, sex, race/ethnicity, language, insurance coverage, and having PCPs. Adjusted odds ratios (AORs) were reported with 95% confidence intervals (CIs). Investigators used STATA 14.2 (College Station, TX) for all statistical study analyses, with P < 0.05 considered statistically significant.
Reporting guideline
This study was reported using the Strengthening of the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines [25].
| Results | ▴Top |
In this study, after excluding patients who did not have previous exposure to the study healthcare system with no PP access, we found 82,745 unique patients met the inclusion criteria during the study period. After further exclusion of 4,768 patients of other races/ethnicities, a total of 77,977 unique patients were placed in our final analysis, among which 26,463 patients (34%) were NHW, 25,939 patients (33%) were NHB, and 25,575 patients (33%) were Hispanic/Latinos. Therefore, well-balanced patient populations of three different races/ethnicities were achieved. A detailed study flow diagram is shown in Figure 1.
Table 1 shows the baseline characteristics of the study patients. We divided all patients into three groups. The rate of PP use among patients of NHW was higher than those of NHB and Hispanic/Latinos (P < 0.0001). Additionally, NHB and Hispanic/Latino patients tended to be female predominant, and younger than NHWs (P < 0.0001). Hispanic/Latino patients had less insurance coverage than NHW and NHB, whereas NHB patients had less PCPs than NHW and Hispanic/Latinos (P < 0.0001). In terms of chronic conditions, the top nine common chronic conditions are listed in Table 1. NHB and Hispanic/Latino patients had a higher occurrence of DM than NHW, whereas NHW had a higher occurrence of depression, asthma/chronic obstructive pulmonary disease (COPD), and coronary artery disease (CAD)/congestive heart failure (CHF) than NHB and Hispanic/Latino (Table 1).
 Click to view | Table 1. Description of the Study Population (N = 77,977) |
Since one of this study’s foci was determining PP status in patients with DM, we further divided patients into five groups (group 1: patients with no chronic disease, group 2: patients with only a history of DM, group 3: patients with one chronic condition but not DM, group 4: patients with multimorbidity including DM, and group 5: patients with multimorbidity without DM). We found that only 1.3% (1,041/77,977) patients had DM as their only chronic condition. The PP use rate increased with the addition of chronic conditions regardless of patient races/ethnicities (Table 2). In general, more PP users were found in NHW patients than NHB and Hispanic/Latino patients.
 Click to view | Table 2. Patient PP Use Among ED Patients With Different Races/Ethnicities |
When determining factors associated with PP use, a multivariate logistic regression was performed. The AOR of NHB with PP use was 0.61 (95% CI: 0.58 - 0.64, P < 0.0001) and the AOR of Hispanic/Latino with PP use was 0.91 (0.86 - 0.96, P < 0.0001) in comparison to PP use among NHWs. These findings indicate the lack of PP usage among NHB and Hispanic/Latino patients. Additionally, increased PP use occurred with the increased number of patients’ chronic conditions, and such a trend occurred among patients with any chronic conditions. These findings indicate that DM is not the only chronic disease promoting the use of PP (Table 3). We also found that females tended to use PP more often than males (AOR = 2.09, 95% CI: 2.01 - 2.17, P < 0.0001). The AOR of insurance coverage was 2.12 (2.02 - 2.23, P < 0.0001) and having a PCP was 3.89 (3.71 - 4.07, P < 0.0001), indicating these two independent factors potentially promoting PP usage (Table 3).
 Click to view | Table 3. Factors Associated With PP Use Among ED Patients |
To further determine the association of PP use and patient clinical outcomes, a sub-cohort analysis was performed in DM patients. Blood serum glucose level and patient hospitalization were considered as two outcome measures. After adjusting for age, sex, race/ethnicity, language spoken, insurance coverage, PCP, and patient chronic conditions, PP use was not associated with better serum glycemic control (AOR = 0.98, P = 0.547). However, PP use was associated with significant reduction of patient hospitalization (AOR = 0.79, P < 0.0001, Table 4).
 Click to view | Table 4. Factors Associated With Serum Glycemic Control and ED Disposition Among Diabetic Patients |
| Discussion | ▴Top |
To determine healthcare disparity in PP use, we performed a comparison study among three patient populations (i.e., NHW, NHB, and Hispanic/Latino) within the same healthcare environment. We found healthcare disparities still exist with PP use in NHB and Hispanic/Latino patients when compared to their NHW counterparts. Such disparity not only occurred among patients with DM but extended to patients with other chronic conditions. Meanwhile, being a female, having insurance coverage, and having PCPs positively correlated to patient PP usage. When focused on patients with DM, our findings show no association between PP use and serum glycemic control. However, our results show that patients who used PP had less hospitalizations in comparison to ones not using PP. Our study used well-balanced patient populations (i.e., similar sample size in NHW, NHB, and Hispanic/Latino) within the same healthcare system, determined the existence of PP use disparity among NHB and Hispanic/Latinos, and further identified factors promoting PP use. Our study findings contributed in several important areas to the literature pool: 1) a direct comparison of three common patient populations with relatively large sample size, 2) not only focusing on patients with DM but analyzing patients with other common chronic health conditions, and 3) determined PP status in an acute care setting instead of clinical setting, where PP use is not often emphasized. Our study findings could serve as a foundation for future implantation of efficient interventions to promote PP use, especially at an acute care setting.
PP use disparity has been reported in the past [6, 9, 26]. Our findings show similar results and validate the current PP use disparity among NHB and Hispanic/Latino patients, with a more robust sample population [26]. Many factors could be associated with such disparities, including low socioeconomic status (SES), education level, or internet access [10, 27, 28]. These factors have been reported and validated in the past. Therefore, our study avoids such redundancies. Instead, we focused on potential factors that can be promoted by healthcare providers. Our findings showed insurance coverage and having a PCP are two factors promoting PP use. Though similar findings were reported in the past, it was reported from a national representative survey with no emphasis on patients with different races/ethnicities, nor focus on patients with DM [20]. Our study validated facilitators that may affect PP use regardless of patient race/ethnicity. Implementations to increase insurance coverage by providing hospital sponsored insurance coverage and increasing the referrals to PCPs by case managers in the study hospital have been initiated and showed certain improvement [29].
Strikingly, we did not find any association between PP use and patient serum glycemic control. Previous studies showed better DM control with the use of PP [6, 13]. However, these studies were either performed outside of an acute care setting or occurred as survey questionnaires [6, 13]. Furthermore, the high serum glucose levels might be affected by multiple factors including infection, medication interactions, stress, etc. [30-32]. DM patients might present to the ED due to other acute conditions unrelated to their DM, which might indirectly cause the elevation of serum glucose levels. We did not analyze patients’ HbA1c level since this is not a routine test ordered in the ED. Given the potential for many confounding factors which can result in the elevation of serum glucose, we believe using HbA1c as the outcome measure may be better for determining such an association. On the other hand, this study also found that patients using PP had less hospitalizations. This may indicate that establishing patient-provider communication could avoid unnecessary hospitalizations. There are many PP features that could enhance patient-provider communication. If ED physicians recognized these resources, they may feel less pressure to admit patients especially among patients with high psychosocial risks. However, our study findings did not have direct evidence to support this hypothesis and future research is warranted for such validations.
Our study has the strength of a relatively large sample size with balanced patient populations. In addition, factors promoting the PP use determined in this study are feasible interventions that could be initiated instantly. Our future study will be to determine PP use with these interventions and further determine the association between PP use and patient clinical outcomes using better outcome indicators. Since such interventions can be applied to any patient populations, PP use disparity might thus be minimized.
This study has its limitations. First, since this is a retrospective cross-section study, incomplete, inaccurate, or missing data cannot be completely avoided. Due to data from a single healthcare system, we are unable to determine PP use status outside of our system. However, as the study hospital is the only publicly funded hospital in the county and most of the patient population received benefit from seeking healthcare in the study hospital (e.g., with hospital sponsored health insurance coverage, robust case management and social work network within the study healthcare system, etc.), we assume that very few patients would seek care from outside healthcare systems. Second, MyChart is one of the PPs that was investigated in our study. Since different PPs in different electronic medical records might have different features, our study findings might only reflect ones using MyChart and may not be generalizable. Future studies focusing on different PPs should be performed to validate our findings. Third, we were unable to include all variables that could affect PP use. We avoided choosing variables that have already been well validated in previous studies, although this could lead to some bias in the statistical analyses. Fourth, as mentioned above, we chose serum glucose level as one of the outcome measures, which might not be an accurate representation of serum glycemic control. Fifth, since our study hospital is a publicly funded hospital with special vulnerable patient populations, our findings might only be applied to patients in a similar setting. Therefore, a prospective multi-center study is warranted to further validate our findings.
Conclusion
PP use disparity occurred among NHB and Hispanic/Latino patients in the ED. Having insurance coverage and a PCP was associated with increased PP use. PP use was not associated with serum glycemic control in DM patients presenting to the ED but could possibly reduce patient hospitalizations.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
This is waived by regional institution review board.
Author Contributions
Conceptualization: HW, RK, AFH, and CDS. Methodology: HW, AP, and MB. Validation: AP, MB, and JB. Formal analysis: HW, RK, and CDS. Data curation: HW and RK. Writing original draft preparation: HW and RK. Writing review and editing: HW, RK, AP, MB, AFH, JB, and CDS.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Turner K, Hong YR, Yadav S, Huo J, Mainous AG. Patient portal utilization: before and after stage 2 electronic health record meaningful use. J Am Med Inform Assoc. 2019;26(10):960-967.
doi pubmed - Zhao JY, Song B, Anand E, Schwartz D, Panesar M, Jackson GP, Elkin PL. Barriers, facilitators, and solutions to optimal patient portal and personal health record use: a systematic review of the literature. AMIA Annu Symp Proc. 2017;2017:1913-1922.
- Wright JA, Volkman JE, Leveille SG, Amante DJ. Predictors of Online Patient Portal Use Among a Diverse Sample of Emerging Adults: Cross-sectional Survey. JMIR Form Res. 2022;6(2):e33356.
doi pubmed - Sarkar U, Lyles CR, Parker MM, Allen J, Nguyen R, Moffet HH, Schillinger D, et al. Use of the refill function through an online patient portal is associated with improved adherence to statins in an integrated health system. Med Care. 2014;52(3):194-201.
doi pubmed - Yang R, Zeng K, Jiang Y. Prevalence, factors, and association of electronic communication use with patient-perceived quality of care from the 2019 Health Information National Trends Survey 5-Cycle 3: exploratory study. J Med Internet Res. 2022;24(2):e27167.
doi pubmed - Sun R, Burke LE, Saul MI, Korytkowski MT, Li D, Sereika SM. Use of a patient portal for engaging patients with type 2 diabetes: patterns and prediction. Diabetes Technol Ther. 2019;21(10):546-556.
doi pubmed - Coughlin SS, Heboyan V, Young L, De Leo G, Wilkins T. Use of a web portal by adult patients with pre-diabetes and type 2 diabetes mellitus seen in a family medicine outpatient clinic. J Hosp Manag Health Policy. 2018;2:21.
doi pubmed - Graetz I, Gordon N, Fung V, Hamity C, Reed ME. The digital divide and patient portals: internet access explained differences in patient portal use for secure messaging by age, race, and income. Med Care. 2016;54(8):772-779.
doi pubmed - Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, Lopez A, Schillinger D. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18(3):318-321.
doi pubmed - Sun R, Korytkowski MT, Sereika SM, Saul MI, Li D, Burke LE. Patient portal use in diabetes management: literature review. JMIR Diabetes. 2018;3(4):e11199.
doi pubmed - Reed ME, Huang J, Brand RJ, Neugebauer R, Graetz I, Hsu J, Ballard DW, et al. Patients with complex chronic conditions: Health care use and clinical events associated with access to a patient portal. PLoS One. 2019;14(6):e0217636.
doi pubmed - Alturkistani A, Qavi A, Anyanwu PE, Greenfield G, Greaves F, Costelloe C. Patient portal functionalities and patient outcomes among patients with diabetes: systematic review. J Med Internet Res. 2020;22(9):e18976.
doi pubmed - Conway NT, Allardice B, Wake DJ, Cunningham SG. User Experiences of an Electronic Personal Health Record for Diabetes. J Diabetes Sci Technol. 2019;13(4):744-750.
doi pubmed - Sun R, Burke LE, Korytkowski MT, Saul MI, Li D, Sereika SM. A longitudinal examination of patient portal use on glycemic control among patients with uncontrolled type 2 diabetes. Diabetes Res Clin Pract. 2020;170:108483.
doi pubmed - Lau M, Campbell H, Tang T, Thompson DJ, Elliott T. Impact of patient use of an online patient portal on diabetes outcomes. Can J Diabetes. 2014;38(1):17-21.
doi pubmed - Zocchi MS, Robinson SA, Ash AS, Vimalananda VG, Wolfe HL, Hogan TP, Connolly SL, et al. Patient portal engagement and diabetes management among new portal users in the Veterans Health Administration. J Am Med Inform Assoc. 2021;28(10):2176-2183.
doi pubmed - Shimada SL, Allison JJ, Rosen AK, Feng H, Houston TK. Sustained use of patient portal features and improvements in diabetes physiological measures. J Med Internet Res. 2016;18(7):e179.
doi pubmed - Kooij L, Groen WG, van Harten WH. Barriers and facilitators affecting patient portal implementation from an organizational perspective: qualitative study. J Med Internet Res. 2018;20(5):e183.
doi pubmed - Powell KR. Patient-perceived facilitators of and barriers to electronic portal use: a systematic review. Comput Inform Nurs. 2017;35(11):565-573.
doi pubmed - El-Toukhy S, Mendez A, Collins S, Perez-Stable EJ. Barriers to patient portal access and use: evidence from the health information national trends survey. J Am Board Fam Med. 2020;33(6):953-968.
doi pubmed - Wang H, Ho AF, Wiener RC, Sambamoorthi U. The Association of Mobile Health Applications with self-management behaviors among adults with chronic conditions in the United States. Int J Environ Res Public Health. 2021;18(19):10351.
doi pubmed - Han HR, Gleason KT, Sun CA, Miller HN, Kang SJ, Chow S, Anderson R, et al. Using patient portals to improve patient outcomes: systematic review. JMIR Hum Factors. 2019;6(4):e15038.
doi pubmed - Wade-Vuturo AE, Mayberry LS, Osborn CY. Secure messaging and diabetes management: experiences and perspectives of patient portal users. J Am Med Inform Assoc. 2013;20(3):519-525.
doi pubmed - Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis. 2013;10:E66.
doi pubmed - von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800-804.
doi pubmed - Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med. 2011;26(10):1112-1116.
doi pubmed - Ronda MC, Dijkhorst-Oei LT, Rutten GE. Reasons and barriers for using a patient portal: survey among patients with diabetes mellitus. J Med Internet Res. 2014;16(11):e263.
doi pubmed - Irizarry T, DeVito Dabbs A, Curran CR. Patient portals and patient engagement: a state of the science review. J Med Internet Res. 2015;17(6):e148.
doi pubmed - Schrader CD, Robinson RD, Blair S, Shaikh S, Ho AF, D'Etienne JP, Kirby JJ, et al. Common step-wise interventions improved primary care clinic visits and reduced emergency department discharge failures: a large-scale retrospective observational study. BMC Health Serv Res. 2019;19(1):451.
doi pubmed - Dungan KM, Braithwaite SS, Preiser JC. Stress hyperglycaemia. Lancet. 2009;373(9677):1798-1807.
doi - Konishi H, Shirakawa J, Arai M, Terauchi Y. Drug-induced hyperglycemia in the Japanese Adverse Drug Event Report database: association of evelolimus use with diabetes. Endocr J. 2019;66(6):571-574.
doi pubmed - Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17(1):11-30.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


