| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Short Communication
Volume 14, Number 10, October 2022, pages 425-431
Preliminary Experience With Quadratus Lumborum Catheters for Postoperative Pain Management in Pediatric-Aged Patients With Contraindications to Epidural Anesthesia
Rachel Pooleya, Giorgio Venezianob, c, Candice Burrierb, c, Nguyen K. Tramb, c, Joseph D. Tobiasb, c, d
aHeritage College of Osteopathic Medicine, Dublin Campus, Dublin, Ohio and Ohio University, Athens, OH, USA
bDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
cDepartment of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
dCorresponding Author: Joseph D. Tobias, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 43205, USA
Manuscript submitted August 17, 2022, accepted September 23, 2022, published online October 28, 2022
Short title: QL Catheters for Postoperative Pain Management
doi: https://doi.org/10.14740/jocmr4813
| Abstract | ▴Top |
Background: Although neuraxial techniques such as caudal and epidural anesthesia were initially the predominant regional anesthetic technique used to provide postoperative analgesia in children, there has been a transition to the use of peripheral nerve blockade such as the quadratus lumborum block (QLB). We present preliminary experience with QL catheters for continuous postoperative analgesia in a cohort of pediatric patients following colorectal surgery.
Methods: After institutional review board (IRB) approval, we retrospectively reviewed the records of patients who underwent major colorectal surgery and received QL catheters for postoperative analgesia. The postoperative pain control data consisted of QL catheter characteristics, anesthetic agents, adjuncts, pain scores, and opioid consumption during the postoperative period.
Results: The study cohort included eight pediatric patients, ranging in age from 1 to 19 years (median age 11.8 years). The QL catheters were placed in the operating room after the induction of anesthesia. Comorbid conditions in the cohort that were contraindications to neuraxial anesthesia included spinal/vertebral malformations, presence of a ventriculoperitoneal (VP) shunt, anal atresia, tracheo-esophageal fistula (VACTERL) association, and coagulation disturbances. All patients underwent complex colorectal or genito-urologic procedures. Bilateral QL catheters were placed in six patients, and unilateral catheters were placed in two patients. Four patients received 0.5% ropivacaine and four patients received 0.2% ropivacaine of an initial bolus. The local anesthetic used for continuous infusion was 0.2% ropivacaine in five patients, 0.1% ropivacaine in two patients, and 1.5% chloroprocaine in one patient, with a median infusion rate of 0.11 mL/kg/h. QL catheter infusions were supplemented with intravenous opioids delivered by patient-controlled or nurse-controlled analgesia. The median opioid requirements in oral morphine milligram equivalents (MME) were 1.2, 1.0, 1.1, 0.5, and 0.6 MME/kg on postoperative days 1 - 5. Daily median pain scores were ≤ 2 during the 5-day postoperative course. All catheters functioned successfully and were in place for a median of 79.3 h. Other than early inadvertent removal of two catheters, no adverse effects were noted.
Conclusions: Although our preliminary data suggest the efficacy of QL catheters in providing prolonged postoperative analgesia for up to 3 - 5 days following colorectal procedures, attention needs to be directed at measures to ensure that the catheter is secured to avoid inadvertent removal.
Keywords: Quadratus lumborum block; Pediatric; Children; Postoperative analgesia; Local anesthetic
| Introduction | ▴Top |
The assessment and management of postoperative pain in the pediatric population remains challenging and despite ongoing refinements of techniques, the control of post-surgical pain may be suboptimal [1, 2]. To address these issues, there has been an increased use of regional anesthetic techniques to improve postoperative analgesia while limiting the adverse effects of systemic opioids [3, 4]. Although neuraxial techniques (caudal and epidural anesthesia) were the predominant regional anesthetic technique initially used in children, there has been a transition to peripheral nerve blockade as a means of prolonged postoperative analgesia [5]. Advantages of peripheral nerve blockade include selective blockade with unilateral analgesia, avoidance of sympathetic blockade, selective sensory blockade and preservation of motor function, a lower incidence of urinary retention, and the use of lower volumes of the local anesthetic agent thereby resulting in a limited potential for local anesthetic systemic toxicity (LAST) [5, 6]. Additionally, there may be anatomical or patient-related comorbid conditions which preclude the use of neuraxial techniques.
First described in the adult population, the quadratus lumborum block (QLB) is a variation of a transversus abdominis plane (TAP) block used to provide postoperative analgesia following abdominal surgery. Like the TAP block, the QLB is an inter-fascial block requiring deposition of the local anesthetic agent between the fascial layers. The primary ultrasound landmark for accurate performance is the quadratus lumborum muscle (QLM) while the key to analgesia is the thoracolumbar fascia (TLF). While it remains open for debate, the mechanism of the analgesia provided by the QLB is postulated to result from the spread of the local anesthetic agent along the TLF and the endothoracic fascia into the paravertebral space, over the anterior primary rami of the various spinal nerves in the thoracolumbar region, thereby providing cutaneous analgesia to the dermatomes of the anterior abdominal wall [7-11]. The degree of dermatomal coverage, which may extend from T5 to L1, depends on the volume injected and hence the spread within the paravertebral space. Additional visceral analgesia may be provided by epidural spread of the local anesthetic agent or splanchnic sympathetic blockade. As QLBs can provide somatic as well as visceral analgesia of both the abdominal wall and the lower aspects of the thoracic wall, it may be a useful analgesic modality for selected abdominal surgical procedures involving the lower thoracic and lumbar dermatomes [12-20].
To date, the majority of experience with QLBs in both the adult and pediatric population have included single injection techniques. As with other forms of peripheral nerve or inter-fascial blockade, the duration of analgesia may be extended by catheter placement and continuous infusion of a local anesthetic agent rather than a single shot technique [21, 22]. So far, there are a limited number of reports of the use of QL catheters to provide analgesia following abdominal surgery in pediatric-aged patients. We present preliminary experience with the largest reported cohort of pediatric patients in whom QL catheters were used for continuous postoperative analgesia following colorectal surgery.
| Materials and Methods | ▴Top |
This study was approved by the Institutional Review Board of Nationwide Children’s Hospital (MOD00012593) and conducted in accordance with the regulations of the Declaration of Helsinki for research involving human subjects. As a retrospective cohort study, patients were deemed as exposed to no more than minimal risk and the need for individual written informed consent was waived. To maintain patient confidentiality, only deidentified data were used for the purpose of this study. Data collected during this study were stored in a secure location and only the collaborators directly involved in this study have access. All electronic files were stored on a secure, password-protected network.
Patients who received a unilateral QL catheter or bilateral QL catheters for postoperative analgesia during 36-month time period were identified. The electronic medical record was reviewed for patient demographic data including the surgical procedure (type and duration), and specifics regarding the QL block including the technique of placement. Demographic information obtained included age, weight, gender, and coexisting medical conditions, such as the presence of spinal cord or vertebral abnormalities (spinal dysraphism) and coagulation disturbances. The postoperative pain control data consisted of QL catheter characteristics (local anesthetic used and the infusion rate), analgesic adjuncts administered postoperatively, and opioid consumption. Also documented were postoperative pain scores, hospital length of stay, time to first ambulation, intensive care unit (ICU) stay, time to first bowel movement, and time to first oral intake. Adverse effects and complications related to the QL catheter, and the local anesthetic infusion were also noted.
Technique for catheter placement
Intraoperative placement of the QL catheters, postoperative use of the QL catheters and, analgesic decisions were directed by the attending pediatric anesthesiologist on the Acute Pain Service. This included the use of local anesthetic bolus doses and rate changes of the ropivacaine infusion. All catheters were placed after the induction of general anesthesia and endotracheal intubation. The patient was positioned in the lateral decubitus with the surgical side facing up. Prior to catheter placement, the skin was prepped with chlorhexidine and draped in sterile fashion. An 18-gauge Tuohy needle was advanced with in-plane ultrasound guidance to the inter-fascial plane between the quadratus lumborum and iliopsoas muscles (anterior technique) or to the lateral aspect of the quadratus lumborum muscle adjacent to the aponeurosis of the transversus abdominis muscle (lateral technique). Using weight-based local anesthetic dosing, ropivacaine (0.2% or 0.5%) was deposited in the fascial plane and a 20-gauge catheter was threaded 4 - 6 cm beyond the needle tip prior to removing the needle. The catheter was secured with 2-octyl cyanoacrylate (Dermabond®) and an occlusive dressing was placed over the insertion site. For bilateral catheters, the patient was repositioned, and the procedure was repeated on the contralateral site.
Postoperative catheter care
Postoperatively, the QL catheters were continuously infused with ropivacaine (0.1% or 0.2%) or chloroprocaine 1.5%. When ropivacaine was used, the infusion rate and concentration were adjusted so as not to exceed departmental-based guidelines of 0.4 mg/kg/h. Selection of the ropivacaine concentration was based on the patient’s weight, the intended infusion rate, and adherence to institutional local anesthetic dosing guidelines. Postoperative analgesia was supplemented by bolus doses of intravenous opioids (morphine or hydromorphone) administered by patient-controlled or nurse-controlled analgesia. Once patients were tolerating oral intake, analgesia supplementation was changed to oral opioids (oxycodone). Catheters were removed at the bedside when no longer indicated or when catheter concerns (nonocclusive dressing barrier breach, inadvertent catheter disconnect) were noted.
Data presentation and statistical analysis
The following postoperative outcomes were analyzed during the postoperative period: pain scores, use of adjunctive analgesic agents, opioid consumption, and QLB-related complications. Pain was evaluated in our study population by a visual analog pain score (VAS) using a 0 - 10 scale. If the VAS scale could not be used based on the patient's age or cognitive state, an observational scale (Wong-Baker pain scale or Faces, Legs, Agitation, Cry, and Consolability or FLACC scale), was used. All three scales are validated assessment tools for pain that use a 10-point grading system, with zero being most comfortable or no pain. Pain scores were collected at 6-h intervals for all patients. Mean individual pain scores for each 24-h postoperative period were tabulated and the median and interquartile range were calculated. Opioid consumption was determined over the first 5 postoperative days with conversion of all administered intravenous and oral opioids to oral morphine milligram equivalents (MMEs) in mg/kg/day [23].
Parametric continuous data were presented as means and standard deviations. Nonparametric data were presented as medians and interquartile ranges. Categorical variables were presented as frequencies and percentages. Repeated measures analysis of variance (ANOVA) was used to determine the statistical trends for pain score and opioid use observed for postoperative days. All statistical analysis was performed using Python (Python Software Foundation, Wilmington, DE).
| Results | ▴Top |
The study cohort included eight patients, ranging in age from 1 to 19 years (median age 11.8 years) and a median weight of 41.3 kg. The demographic data for the cohort are summarized in Table 1. Comorbid conditions which generally precluded the use of neuraxial anesthesia included coagulation disturbances or vertebral and spinal abnormalities such as tethered spinal cord, spina bifida, and myelomeningocele. All the patients underwent complex colorectal and genito-urologic procedures including exploratory laparotomy, lysis of intra-abdominal adhesions, colostomy placement or revision, posterior sagittal anorectoplasty, and bowel resection.
 Click to view | Table 1. Demographic Data of the Study Cohort |
The QL catheters were bilateral in six patients and unilateral in two patients. The QL catheter characteristics are outlined in Table 2. The median procedure time for QL catheter placement was 15 min (interquartile range (IQR): 11.5, 18.0 min). There were no patient-related complications during QL catheter placement or subsequent use. Following placement, a bolus dose of the local anesthetic was administered through the catheter (median volume of 0.5 mL/kg, IQR: 0.3, 0.7) of either 0.2% ropivacaine or 0.5% ropivacaine. The local anesthetic used for continuous infusion was 0.2% ropivacaine in five patients, 0.1% ropivacaine in two patients, and 1.5% chloroprocaine in one patient. The infusion rate of the local anesthetic agent was a median of 0.11 mL/kg/h (IQR: 0.06, 0.16). In one patient, the infusion was decreased from 6 mL/h to 3 mL/h as the parents noted subjective concerns that the patient was sleepy while the patient stated that they felt flushed and dizzy. The success rate was judged as 100% with patients generally maintaining median pain scores ≤ 2 during the postoperative course (Fig. 1). Other than early removal of catheter (n = 2, 25%), no complications were documented. Catheters remained in place for a median of 79.3 h (IQR: 15.1, 110.7 h). Early removal of the catheter was necessitated in two patients by disconnection of the infusion tubing or disruption of the sterile barrier of the bio-occlusive dressing of the catheter. One additional patient required removal of one side of their bilateral catheters due to inadvertent disconnection of the infusion tubing.
 Click to view | Table 2. Quadratus Lumborum Catheter Characteristics |
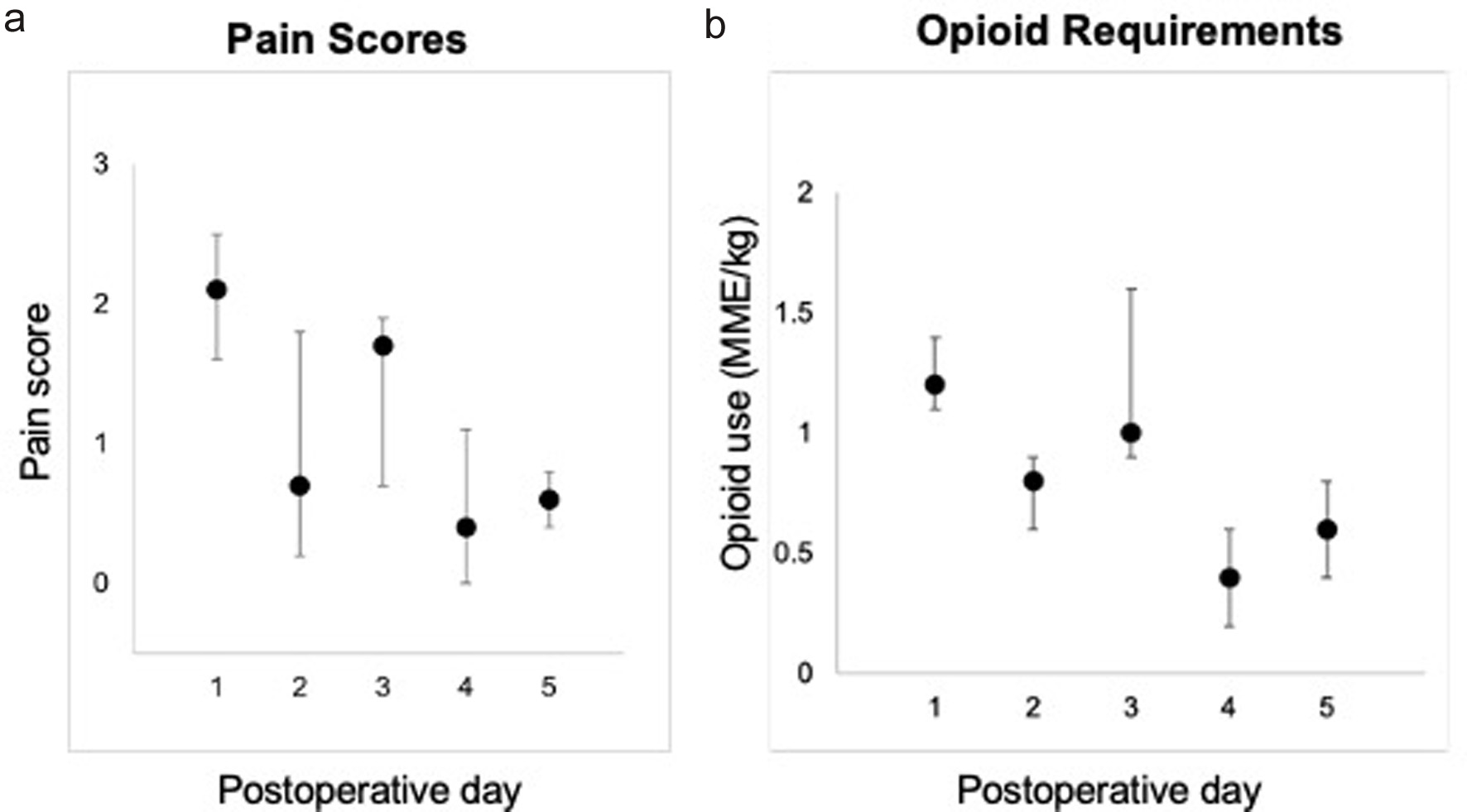 Click for large image | Figure 1. Postoperative pain scores (a) using a 0 - 10 visual analogue score and opioid requirements (b) expressed as oral MMEs. MME: morphine milligram equivalent. Data are listed as median and interquartile ranges. |
Postoperative outcome data are listed in Table 3. Three patients were admitted to the ICU after surgery with a median ICU stay time of 15.1 h (IQR: 15.0, 18.9 h). The median time to first ambulation following surgery was 51.8 h (IQR: 21.1, 68.7 h). The time to first intake was 32.7 h (IQR: 17.3, 54.7 h). The first flatus or bowel movement occurred at 24.8 h (IQR: 16.7, 42.2 h) postoperatively. Daily median pain scores were ≤ 2.1 during the first 5 postoperative days. The QL catheter infusion was supplemented with intravenous opioids (nurse-controlled analgesia (NCA) or patient-controlled analgesia (PCA)), with six patients receiving hydromorphone and two patients receiving morphine. If needed, patients were transitioned to the opioid oxycodone once they were able to tolerate oral intake. The median opioid requirements in oral MME were 1.2, 1.0, 1.1, 0.5, and 0.6 MME/kg on the first 5 postoperative days, respectively. No statistical trends were found for pain score and opioid use observed for the postoperative days. Adjunctive analgesic agents are listed in Table 4. Acetaminophen was used in all eight patients while diazepam was used in six patients.
 Click to view | Table 3. Postoperative Course |
 Click to view | Table 4. Postoperative Analgesic Adjuncts |
| Discussion | ▴Top |
The QLB has gained popularity as a nonopioid adjunct in lower thoracic and abdominal surgery, owing to its efficacy, opioid-sparing properties, and avoidance of neuraxial access. While several studies have demonstrated the utility of the QLB in various surgical procedures, predominantly in the adult population, the limited published data also support its efficacy in the pediatric population. Our retrospective study summarizes the characteristics and safety profile of a novel technique using QL catheters as a means of providing prolonged analgesia (up to 5 days) following colorectal surgery in children and adolescents. To date, this is the first study outlining the use of QL catheters with a continuous infusion as opposed to a single shot technique. This technique allows the feasibility of continuing the use of the regional anesthetic technique for up to 3 - 5 days following the surgical procedure as compared to 12 - 18 h of analgesia following a single bolus technique [24]. Our retrospective review suggests that the QLB with continuous infusions can be performed safely and efficiently in anesthetized patients with a high success rate, and it may serve as a useful analgesic adjunct for children undergoing open colorectal surgery.
As the QLB (continuous infusion or single bolus technique) is our current standard for providing postoperative analgesia following major colorectal surgery in infants and children, a comparable control group was not available during the same time period at our institution. To evaluate the analgesia efficacy, it is necessary to compare our data (patient scores and opioid requirements) to that from a published cohort of similar patients that did not receive a QLB [25]. George et al reported an average 24-h postoperative pain score of 4.5 in 148 children who underwent laparoscopic and open colorectal surgery without the use of adjunctive regional anesthesia [25]. The median postoperative pain score was 2.1 in our cohort of patients during the first 24 postoperative hours with a reduction in the need for systemic opioids [26]. The analgesic efficacy of the QLB in our cohort is likely attributable to analgesic coverage of somatic abdominal pain. However, persistent opioid requirement may be secondary to the visceral pain component which may not be completely controlled by the QLB. This was the case in our patient cohort who received both nonopioid adjunctive agents as well as opioids during the postoperative period.
Although our regional anesthesia practice, specifically that use continuous postoperative infusions, initially focused on the use of neuraxial techniques such as epidural analgesia, our practice has mirrored that of the adult population with a transition over the past 5 - 6 years to an increased use of peripheral nerve blockade including continuous infusions [27, 28]. When compared to epidural anesthesia, advantages of the QLB include the provision of unilateral blockade, avoidance of motor blockade, lack of urinary retention, and placement in patients who are not candidates for neuraxial techniques including those with spinal dysraphism and coagulation disturbances. These latter comorbid conditions are common in patients with anorectal malformations.
Limitations of our current study are inherent to its retrospective nature and include a lack of standardization of the intraoperative anesthetic technique, the postoperative analgesic regimen, and the technique of the QLB. Additionally, there was some variation in the surgical procedure which would likely impact the postoperative course and analgesic requirements. Some of these issues are mitigated to some degree as the technique for QL catheter placement and use (bolus and continuous infusion techniques) did not vary significantly as they followed the structured clinical practice of our acute pain service. Additionally, there was standardization for the assessment of postoperative pain including routine use of pain scores.
Our preliminary data support the use of QL catheters as an adjunctive to the analgesic regimen following major colorectal procedures in infants and children. Our cohort is the first report regarding the use of continuous infusions using QL catheters in pediatric-aged patients. The catheters were effective adjuncts to postoperative analgesia as judged by the postoperative pain scores and opioid requirements. As noted in our cohort, the primary concern was inadvertent catheter disconnects which may result in a risk of infectious complications thereby necessitating catheter removal. However, other potential adverse effects that may occur in larger cohorts include motor blockade due to spread of the local anesthetic to the lumbar plexus and sympathetic blockade with hypotension due to spread of local anesthetic to the paravertebral and epidural space. Additionally, whenever local anesthetic infusions are used postoperatively, attending to local anesthetic dosing is required due to the potential for LAST.
Acknowledgments
None to declare.
Financial Disclosure
This research did not receive any specific grant from agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
None to declare.
Informed Consent
As a retrospective cohort study, patients were deemed as exposed to no more than minimal risk and the need for individual written informed consent was waived.
Author Contributions
Rachel Pooley: data acquisition, manuscript writing including original draft, revisions, and final version. Candice Burrier: patient care in operating room and on the acute pain service, manuscript preparation and review of final draft. Nguyen K. Tram: data analysis, manuscript preparation and review of drafts and final version. Giorgio Veneziano: patient care in operating room and on the acute pain service, manuscript preparation and review of drafts and final version. Joseph D. Tobias: manuscript preparation and review of drafts and final version.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97(2):534-540.
doi pubmed - Taylor EM, Boyer K, Campbell FA. Pain in hospitalized children: a prospective cross-sectional survey of pain prevalence, intensity, assessment and management in a Canadian pediatric teaching hospital. Pain Res Manag. 2008;13(1):25-32.
doi pubmed - Berde CB, Sethna NF. Analgesics for the treatment of pain in children. N Engl J Med. 2002;347(14):1094-1103.
doi pubmed - Ross AK, Eck JB, Tobias JD. Pediatric regional anesthesia: beyond the caudal. Anesth Analg. 2000;91(1):16-26.
doi pubmed - Polaner DM, Taenzer AH, Walker BJ, Bosenberg A, Krane EJ, Suresh S, Wolf C, et al. Pediatric Regional Anesthesia Network (PRAN): a multi-institutional study of the use and incidence of complications of pediatric regional anesthesia. Anesth Analg. 2012;115(6):1353-1364.
doi pubmed - Walker BJ, Long JB, De Oliveira GS, Szmuk P, Setiawan C, Polaner DM, Suresh S, et al. Peripheral nerve catheters in children: an analysis of safety and practice patterns from the pediatric regional anesthesia network (PRAN). Br J Anaesth. 2015;115(3):457-462.
doi pubmed - Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus Lumborum Block: Anatomical Concepts, Mechanisms, and Techniques. Anesthesiology. 2019;130(2):322-335.
doi pubmed - Adhikary SD, El-Boghdadly K, Nasralah Z, Sarwani N, Nixon AM, Chin KJ. A radiologic and anatomic assessment of injectate spread following transmuscular quadratus lumborum block in cadavers. Anaesthesia. 2017;72(1):73-79.
doi pubmed - Elsharkawy H, El-Boghdadly K, Kolli S, Esa WAS, DeGrande S, Soliman LM, Drake RL. Injectate spread following anterior sub-costal and posterior approaches to the quadratus lumborum block: A comparative cadaveric study. Eur J Anaesthesiol. 2017;34(9):587-595.
doi pubmed - Sondekoppam RV, Ip V, Johnston DF, Uppal V, Johnson M, Ganapathy S, Tsui BCH. Ultrasound-guided lateral-medial transmuscular quadratus lumborum block for analgesia following anterior iliac crest bone graft harvesting: a clinical and anatomical study. Can J Anaesth. 2018;65(2):178-187.
doi pubmed - Dam M, Moriggl B, Hansen CK, Hoermann R, Bendtsen TF, Borglum J. The pathway of injectate spread with the transmuscular quadratus lumborum block: a cadaver study. Anesth Analg. 2017;125(1):303-312.
doi pubmed - La Colla L, Ben-David B, Merman R. Quadratus lumborum block as an alternative to lumbar plexus block for hip surgery: a report of 2 cases. A A Case Rep. 2017;8(1):4-6.
doi pubmed - Spence NZ, Olszynski P, Lehan A, Horn JL, Webb CA. Quadratus lumborum catheters for breast reconstruction requiring transverse rectus abdominis myocutaneous flaps. J Anesth. 2016;30(3):506-509.
doi pubmed - Visoiu M, Yakovleva N. Continuous postoperative analgesia via quadratus lumborum block - an alternative to transversus abdominis plane block. Paediatr Anaesth. 2013;23(10):959-961.
doi pubmed - Chakraborty A, Goswami J, Patro V. Ultrasound-guided continuous quadratus lumborum block for postoperative analgesia in a pediatric patient. A A Case Rep. 2015;4(3):34-36.
doi pubmed - Hockett MM, Hembrador S, Lee A. Continuous quadratus lumborum block for postoperative pain in total hip arthroplasty: a case report. A A Case Rep. 2016;7(6):129-131.
doi pubmed - Shaaban M, Esa WA, Maheshwari K, Elsharkawy H, Soliman LM. Bilateral continuous quadratus lumborum block for acute postoperative abdominal pain as a rescue after opioid-induced respiratory depression. A A Case Rep. 2015;5(7):107-111.
doi pubmed - Kadam VR. Ultrasound-guided quadratus lumborum block as a postoperative analgesic technique for laparotomy. J Anaesthesiol Clin Pharmacol. 2013;29(4):550-552.
doi pubmed - Johnston DF, Sondekoppam RV. Continuous quadratus lumborum block analgesia for total hip arthroplasty revision. J Clin Anesth. 2016;35:235-237.
doi pubmed - Hernandez MA, Vecchione T, Boretsky K. Dermatomal spread following posterior transversus abdominis plane block in pediatric patients: our initial experience. Paediatr Anaesth. 2017;27(3):300-304.
doi pubmed - Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011;113(4):904-925.
doi pubmed - Ganesh A, Rose JB, Wells L, Ganley T, Gurnaney H, Maxwell LG, DiMaggio T, et al. Continuous peripheral nerve blockade for inpatient and outpatient postoperative analgesia in children. Anesth Analg. 2007;105(5):1234-1242.
doi pubmed - Gammaitoni AR, Fine P, Alvarez N, McPherson ML, Bergmark S. Clinical application of opioid equianalgesic data. Clin J Pain. 2003;19(5):286-297.
doi pubmed - Manupipatpong K, Anuranhan G, Tram NK, Tobias JD, Veneziano G. Quadratus lumborum blockade for postoperative analgesia in infants and children following colorectal surgery. J Pain Res. (submitted).
- George JA, Salazar AJG, Irfan A, Prichett L, Nasr IW, Garcia AV, Boss EF, et al. Effect of implementing an enhanced recovery protocol for pediatric colorectal surgery on complication rate, length of stay, and opioid use in children. J Pediatr Surg. 2022;57(7):1349-1353.
doi pubmed - Rizk E, Haas EM, Swan JT. Opioid-Sparing Effect of Liposomal Bupivacaine and Intravenous Acetaminophen in Colorectal Surgery. J Surg Res. 2021;259:230-241.
doi pubmed - Gable A, Burrier C, Stevens J, Wrona S, Klingele K, Bhalla T, Martin DP, et al. Home peripheral nerve catheters: the first 24 months of experience at a children's hospital. J Pain Res. 2016;9:1067-1072.
doi pubmed - Heydinger G, Tobias J, Veneziano G. Fundamentals and innovations in regional anaesthesia for infants and children. Anaesthesia. 2021;76(Suppl 1):74-88.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


