| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 4, April 2022, pages 158-164
An Evaluation of the NICCI Monitor in Providing Continuous, Noninvasive Blood Pressure Readings in Children During Intraoperative Anesthetic Care
Ismail Bekiroglua, Kwaku Owusu-Bediakoa, c, Julie Rice-Weimera, Joseph D. Tobiasa, b
aDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
bDepartment of Anesthesiology & Pain Medicine, The Ohio State University, Columbus, OH, USA
cCorresponding Author: Kwaku Owusu-Bediako, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 43205, USA
Manuscript submitted April 12, 2022, accepted April 22, 2022, published online April 30, 2022
Short title: Accuracy of the NICCI Monitor in Children
doi: https://doi.org/10.14740/jocmr4723
| Abstract | ▴Top |
Background: In specific clinical scenarios or with patient comorbid conditions, continuous blood pressure (BP) monitoring may be required as it can be expected to provide superior physiologic monitoring to intermittent techniques. However, continuous BP monitoring requires an arterial cannula (AC) placement, which may be time-consuming, technically challenging, or associated with adverse events. Various noninvasive BP devices have been developed which provide a continuous BP reading. The current study evaluates the accuracy of a novel continuous BP device, the NICCI monitor (NM), in pediatric patients weighing 10 - 40 kg.
Methods: The study cohort included pediatric patients weighing between 10 and 40 kg, scheduled for surgery for which placement of an AC was planned. Systolic (SBP), diastolic (DBP), and mean arterial (MAP) blood pressure readings were captured from the AC and the NM every second during anesthetic care.
Results: The study cohort included 24 pediatric patients undergoing major orthopedic, cardiac, and neurosurgical procedures. A total of 146,562 pairs of SBP, DBP, and MAP values from the AC and NC were analyzed. The absolute difference for the NM and the AC’s SBP, DBP, and MAP values were 11 ± 9, 10 ± 7, and 10 ± 7 mm Hg, respectively. The difference between the BP values from the NM and the AC was ≤ 10 mm Hg for 57% of the SBP readings, 60% of the DBP readings, and 56% of the MAP readings. The bias was 4, 4, and 6 mm Hg for the SBP, DBP, and MAP, respectively.
Conclusions: Although there were some technical limitations given patient size, potentially resulting in variation in accuracy, the NM provided a continuous noninvasive BP measurement within clinically useful limits during a significant portion of anesthetic care compared to values obtained from an AC. Ongoing modification of the technology to improve its application in pediatric patients will likely increase its accuracy.
Keywords: Arterial blood pressure; Blood pressure monitors; Pediatrics anesthesiology; Intraoperative monitoring
| Introduction | ▴Top |
Blood pressure (BP) measurement remains a recommended standard of care for intraoperative monitoring during anesthetic care [1, 2]. In these circumstances, BP is measured either intermittently with a noninvasive, oscillometric blood pressure device or continuously from an invasive arterial cannula. For the majority of surgical procedures, intermittent BP monitoring is sufficient. However, continuous BP monitoring may be preferable based on patient comorbidity or the surgical procedure if hemodynamic impairment or blood loss is anticipated [3]. Arterial cannulation may be time-consuming or even rarely impossible in specific clinical scenarios or patient populations. Additionally, reported adverse effects may include arterial occlusion, hematoma formation, blood loss due to unintended disconnection, infection, nerve injury with sensory disturbances, ischemia, necrosis, and fistula formation [4-7].
Given these concerns, there is ongoing development of technologies to provide continuous noninvasive BP measurement. Many of these devices provide a beat-to-beat BP reading with a waveform similar to that seen with direct arterial cannulation. One novel monitor is the NICCI monitor (NM) (Getinge/Pulsion Medical Systems, Feldkirchen, Germany). The NM uses infrared technology to continuously measure BP and display it in a waveform resembling that of an arterial cannula. The NM may allow the rapid continuous measurement of BP without the need to place an arterial cannula, especially in patients who experience unanticipated hemodynamic instability. The present study prospectively compares systolic, diastolic, and mean arterial pressure readings from an arterial cannula with values obtained using the NM in pediatric patients.
| Materials and Methods | ▴Top |
The study was approved by the Institutional Review Board of Nationwide Children’s Hospital (Columbus, OH, USA) and registered at ClinicalTrials.gov (NCT04373746). The study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from a parent or guardian, and assent for patients ≥ 9 years of age. The NM used for the study was a CE version with an investigational device exemption. As the device is not currently available for commercial sale, no list price has been determined. Inclusion criteria included patients weighing between 10 and 40 kg, undergoing surgical procedures that required an intra-arterial catheter placement. Exclusion criteria included a history of peripheral neurologic disorders, patients in whom an arterial catheter could not be placed, patients with vascular implants at the sites of noninvasive blood pressure (NIBP) measurement, and patients with pre-existing edema of the upper extremities.
The techniques of anesthetic induction and maintenance were left to the discretion of the attending pediatric anesthesiologist. Following the induction of anesthesia, an invasive arterial cannula was placed in a radial artery. After positioning, the sensory from the NM was attached to the patient, with the calibrating NIBP cuff and finger cuff placed on the side opposite the radial arterial cannula (Fig. 1). The site of monitoring in all cases was at the level of the heart. The NM was set up and used according to the manufacturer’s recommendations. Systolic (SBP), diastolic (DBP), and mean arterial pressure (MAP) values from the NM and the arterial cannula were captured every second for subsequent analysis. Following the procedure, the data were downloaded from the laptop via ixTrend software to a standard Excel spreadsheet. Data were reviewed visually, and incomplete data sets or erroneous values such as those recorded during arterial cannula access, arterial cannula calibration, or periodic calibration of the NM were excluded from the analysis.
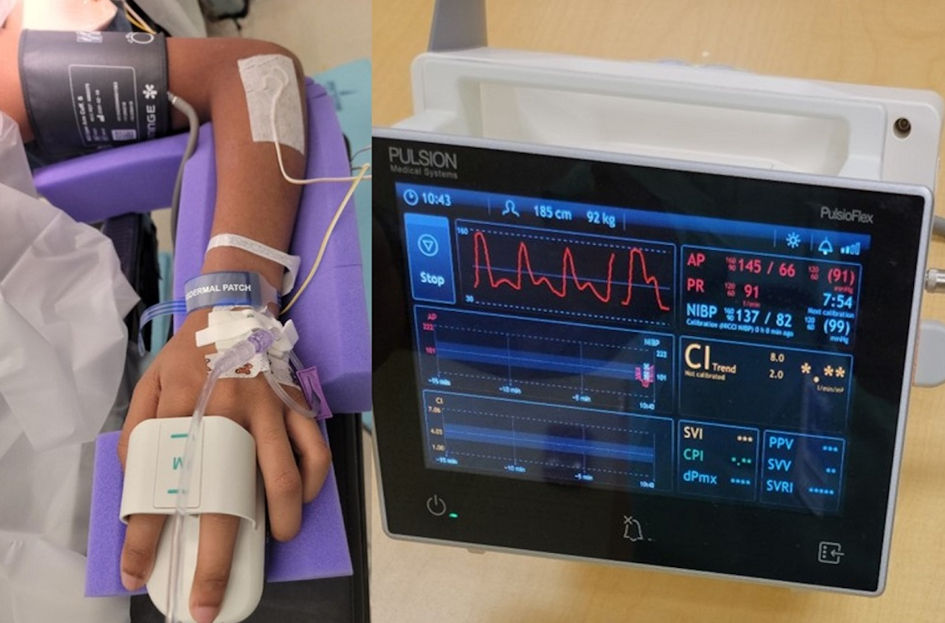 Click for large image | Figure 1. The NICCI device attached to a patient in the prone position with the calibrating noninvasive blood pressure cuff and finger cuffs in place (left). The inflation of the two finger cuffs is alternated to avoid pressure injury. The external pressure required to maintain blood flow within the fingers is measured using infrared technology. The pressure is then converted into a continuous readout which is displayed on the bedside monitor (right). |
Statistical analysis
For data presentation and analysis, the entire cohort’s data were analyzed and presented. Additionally, the patients were divided into two groups based on weight (10 - 25 kg and 25 - 40 kg) for subset analysis and presentation to further evaluate the performance of the device at different pediatric weight classes (see below). Next, we calculated the absolute difference between the SBP, DBP, and MAP values of the arterial cannula and NM. Instead of the directional difference, the absolute difference was used to avoid affecting the data when calculating the mean and standard deviations of the differences. For example, if the reading from the NM was 5 mm Hg above or below the reading from the arterial line, a value of 5 mm Hg was used instead of -5 mm Hg or +5 mm Hg. Additionally, we calculated the percentage of values from the NM that were ≤ 5 mm Hg, ≤ 10 mm Hg, and > 10 mm Hg from the values obtained by the arterial cannula. A Pearson’s correlation coefficient was calculated to compare the SBP, DBP, and MAP values between the values from the NM and the arterial cannula. Finally, a Bland-Altman analysis was performed to determine the bias, precision, and 95% level of agreement between the NM and the arterial cannula values. Briefly, the Bland-Altman plot is a scatterplot of the difference between BP readings from the NM and the arterial cannula (NM - arterial cannula) plotted on the y-axis against the mean of the BP readings from the NM and arterial cannula on the x-axis. Horizontal lines are drawn at the mean difference (blue line) and 95% limit of agreement (mean difference ± 1.96 × standard deviation (SD)) on either side of the mean difference line (red lines). Per routine practice, when calculating the Bland-Altman analysis, the actual value (-5 or +5) was used for calculations. The performance and accuracy of the NM was assessed according to the Association for the Advancement of Medical Instrumentation standards for noninvasive BP measurement. All analyses were conducted using the Statistical Package for the Social Sciences (SPSS) software for Windows, version 26.0. Armonk, New York, IBM Corporation.
| Results | ▴Top |
The study cohort included 24 patients (13 girls, 11 boys) weighing between 10 and 40 kg undergoing major orthopedic, neurosurgical, or cardiothoracic procedures. None of the patients had a history of preoperative hypertension or comorbid conditions related to their BP. The demographic information and clinical characteristics, including positioning for the surgical procedure, are outlined in Table 1. Small size finger cuffs (13 - 17 mm) were used for 17 patients, and medium finger cuffs (16 - 22 mm) were used for seven patients. The NM was placed on the opposite side of the arterial cannula in all of the patients. A total of 146,562 pairs of SBP, DBP, and MAP values from the arterial cannula and the NM were analyzed. The average SBP, DBP, and MAP for the entire study cohort recorded from the NM were 96 mm Hg, 57 mm Hg, and 75 mm Hg, respectively, compared with an average of 92 mm Hg, 53 mm Hg, and 67 mm Hg from the arterial cannula.
 Click to view | Table 1. Demographic and Clinical Characteristics of Study Cohort |
The absolute difference, percentage of values that were ≤ 5 mm Hg, ≤ 10 mm Hg, and more than 10 mm Hg from the actual value of the arterial cannula are listed in Table 2. The correlation coefficients between the readings from the NM and the arterial cannula are summarized in Table 2. The difference between the BP values from the NM and the arterial cannula was ≤ 5 mm Hg for 32% of the SBP readings, 35% of the DBP readings, and 31% of the MAP readings. The difference was ≤10 mm Hg for 57% of the SBP readings, 60% of the DBP readings, and 56% of the MAP readings. The Pearson’s correlation coefficient comparing the values between the NM and those from the arterial cannula showed a strong correlation for the SBP (0.65) and MAP (0.59) and a moderate correlation for the DBP (0.43).
 Click to view | Table 2. Comparison of Blood Pressure Readings From the Arterial Cannula and the NM Monitor |
Table 3 and Figures 2 - 4 display the Bland-Altman analysis with the bias, precision, and 95% level of agreement between the NM and values from the arterial cannula. The difference between the NM and the arterial cannula values is plotted on the vertical axis, while the average of the two values is plotted on the horizontal access. The bias and precision were 4 and 14 mm Hg for the SBP, 4 and 12 mm Hg for the DBP, and 6 and 12 mm Hg for the MAP.
 Click to view | Table 3. Bland-Altman Analysis Comparing Blood Pressure Readings From the Arterial Cannula and NM Monitor |
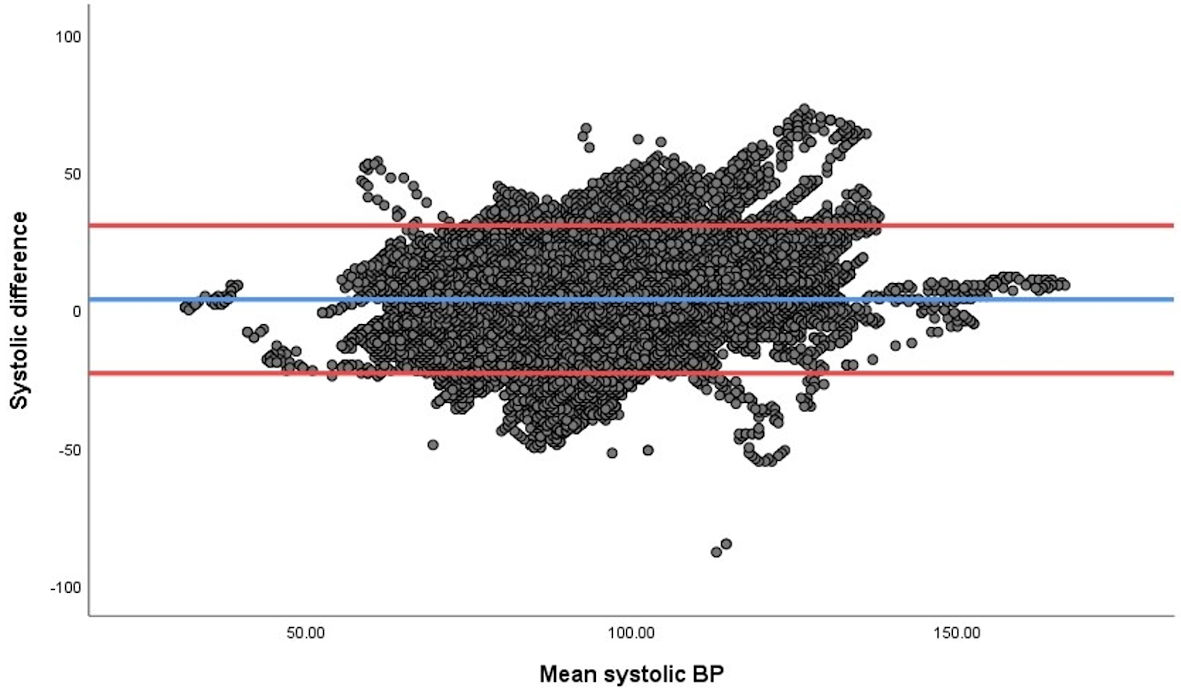 Click for large image | Figure 2. Bland-Altman analysis of the agreement for systolic blood pressure (SBP) readings from the arterial cannula (AC) and the NICCI monitor (NM). The difference between the NM and AC values are plotted on the vertical axis while the average of the two values is plotted on the horizontal access. All values are in mm Hg. The red horizontal lines demonstrate the 95% limits of agreement, and the blue horizontal line corresponds to the bias. |
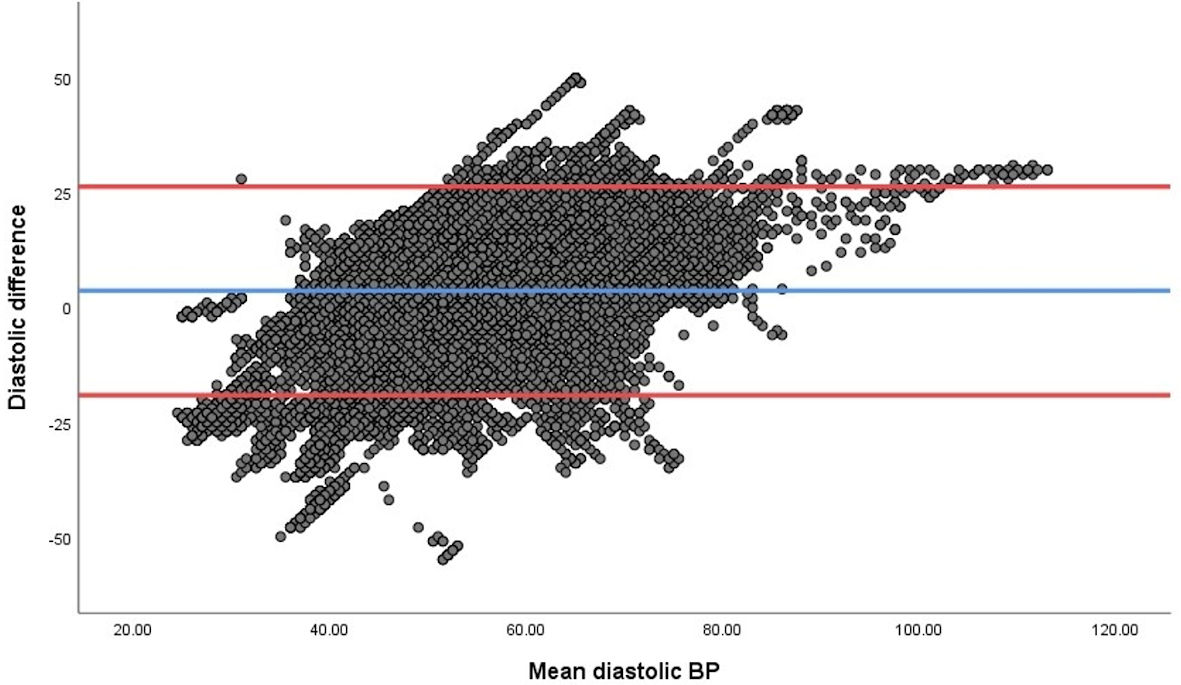 Click for large image | Figure 3. Bland-Altman analysis of the agreement for diastolic blood pressure (DBP) readings from the arterial cannula (AC) and the NICCI monitor (NM). The difference between the NM and AC values are plotted on the vertical axis while the average of the two values is plotted on the horizontal access. All values are in mm Hg. The red horizontal lines demonstrate the 95% limits of agreement, and the blue horizontal line corresponds to the bias. |
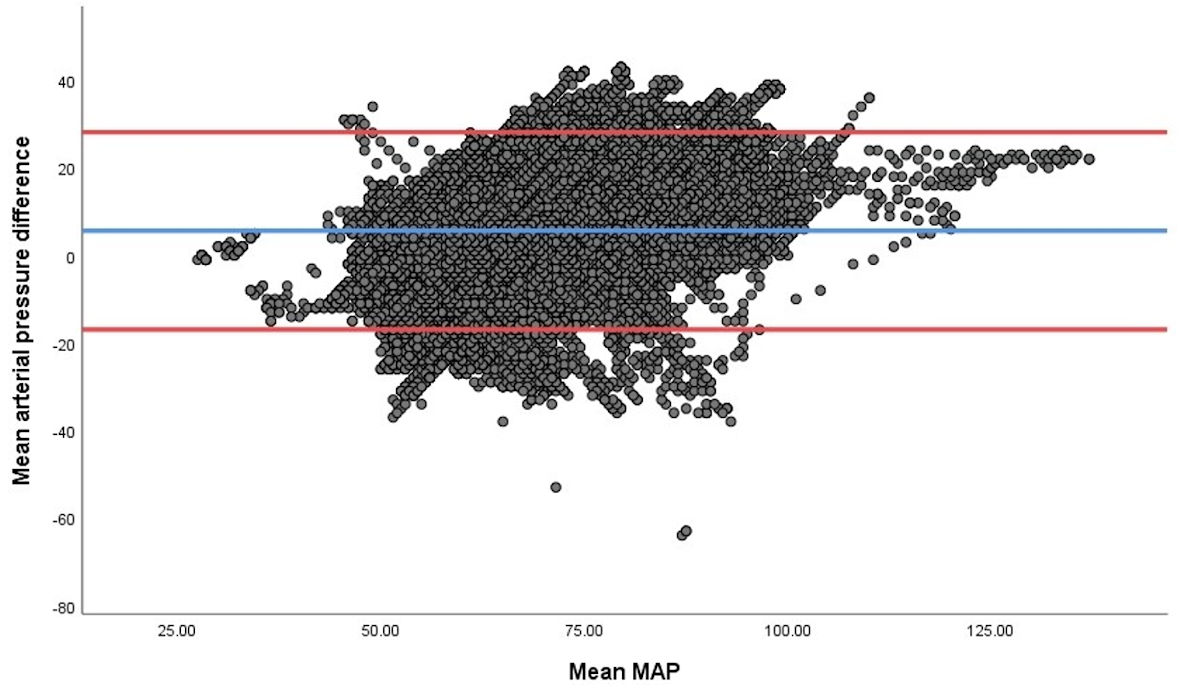 Click for large image | Figure 4. Bland-Altman analysis of the agreement for mean arterial pressure (MAP) readings from the arterial cannula (AC) and the NICCI monitor (NM). The difference between the NM and AC values are plotted on the vertical axis while the average of the two values is plotted on the horizontal access. All values are in mm Hg. The red horizontal lines demonstrate the 95% limits of agreement, and the blue horizontal line corresponds to the bias. |
For the subset analysis, there were seven patients in the 10 - 25 kg weight range and 17 patients in the 25 - 40 kg weight range. The absolute difference, percentage of values that were ≤ 5 mm Hg, ≤ 10 mm Hg, and more than 10 mm Hg from the actual value of the arterial cannula and the correlation coefficients for the two weight groups are listed in Table 4. The Bland-Altman analysis of the two separate weight groups with the bias, precision, and 95% level of agreement are displayed in Table 5.
 Click to view | Table 4. Comparison of Blood Pressure Readings From the Arterial Cannula and NM Monitor Based on Weight |
 Click to view | Table 5. Bland-Altman Analysis Based on Weight |
| Discussion | ▴Top |
The current study investigated the agreement between BP readings from a novel continuous BP device, the NM, and those obtained from an arterial cannula in pediatric patients weighing 10 to 40 kg. The current study is the first to investigate the accuracy of the NM in the pediatric population. This novel technology is based on the continuous noninvasive arterial pressure technology (CNAP™, CNSystems, Graz, Austria) introduced to the market in 2006 [8, 9]. Additional modifications of the technology have resulted in improved hardware design, facilitating set-up, and decreasing application time. The novel hand device that simulates the design of a computer mouse allows easier application of the finger cuffs than the previously used wrist mount and double finger cuff system of the CNAP™ system.
Both of these devices use vascular unloading (volume clamping) technology to provide a real-time beat-to-beat noninvasive measure of BP [2]. The technique of volume clamping was originally developed by Penaz in the 1970s [10]. The absorption of infrared light, which is shined through a finger, is used to estimate the arterial volume within the vascular bed of the digit. Photoplethysmography and closed-loop control of a pneumatic cuff are used to continuously adjust the cuff pressure to regulate the arterial pressure pulse [2]. The external pressure in the finger cuff is rapidly adjusted such that the arterial volume is “clamped” throughout the pressure pulse. As a result, the cuff pressure waveform closely approximates the intra-arterial pressure waveform measured by a noninvasive BP cuff at the arm. The degree of external counter pressure required is compared to the noninvasive BP measurement at the arm (brachial artery) and is converted into a beat-to-beat BP waveform that is displayed on the bedside monitor. The device uses two-finger cuffs, which come in three different sizes (small, medium, large), with infrared light sensors to measure the counter-pressure required to maintain a stable blood flow. The cuffs can be used on fingers varying in size from 13 to 28 mm. Inflation of one of the two cuffs is alternated to allow continued use of the device while limiting the risk of injury from continuous inflation. In addition to continuous BP monitoring, additional analysis of the beat-to-beat BP pulse contour and waveform can be integrated into the device for additional derived hemodynamic parameters, including pulse rate, cardiac index, stroke volume index, stroke volume variation, pulse pressure variation, systemic vascular resistance, and cardiac power index [8, 11].
Similar to previous studies evaluating the CNAP™ device in adult and pediatric populations, the NM provided a continuous noninvasive BP measurement which was within clinically useful limits of values obtained from an arterial cannula during a significant portion of the anesthetic care [8, 9, 11-14]. According to the Association for the Advancement of Medical Instrumentation standards for noninvasive BP measurement (ANSI/AAMI SP10), a clinically acceptable agreement is met by a mean difference of ± 5 mm Hg and a standard deviation of 8 mm Hg [15]. Although the monitor functioned efficiently without technical issues in the current cohort of pediatric patients, it did not meet these strict criteria. However, several factors may impact the accuracy of such devices, including inherent differences in the pediatric arterial system when compared to adults, such as increased compliance of the vascular system, non-supine positioning of patients, and problems with the arm and finger cuffs which are not specifically manufactured for the pediatric population. In some patients, effective fit of the finger cuffs was problematic, given the varied dimensions and shape of the fingers. Another factor that may have affected the accuracy was that the NM was placed on one arm and the arterial cannula was in the other radial artery. Additionally, the NM represents the arterial pressure values at the brachial artery because of the calibration with the upper arm oscillometric measurements using a cuff placed above the elbow. As the arterial pressure measured varies based on the site along the same extremity, the values obtained from two different sites may vary. Although various mechanisms maintain normothermia during intraoperative care, the patient’s hand and forearm may be exposed to lower temperatures in comparison to the core body temperature as they are exposed. This may alter the peripheral circulation, which may affect the NM.
When hemodynamic instability can be predicted, and arterial access is possible, intra-arterial BP measurement remains the gold standard. However, in various clinical scenarios, the NM’s continuous information regarding BP changes may be clinically more relevant and useful than intermittent BP measurements obtained from an oscillometric device. These may include scenarios in which an arterial cannula cannot be placed, in emergent situations when time is limited, in cases of unpredicted hemodynamic instability, or when patient positioning makes arterial cannulation difficult. Additionally, there may be scenarios where the risk-benefit profile does not warrant insertion of an arterial, even if continuous BP monitoring would be beneficial when compared to intermittent BP measurements. Future studies are needed in various clinical scenarios to more formally delineate the application of this new technology in the perioperative setting. Additional technological and equipment modifications may also be feasible to improve its accuracy in the pediatric population.
Acknowledgments
None to declare.
Financial Disclosure
No funding was provided for the study.
Conflict of Interest
No author has a conflict of interest with regard to any device employed in this study. The NICCI monitor used for the study was provided without charge by Getinge/Pulsion Medical Systems SE, Feldkirchen, Germany.
Informed Consent
Written informed consent was obtained.
Author Contributions
Kwaku Owusu-Bediako helped with study design/conduct, patient recruitment, statistical analysis, data interpretation, manuscript preparation and editing. Joseph D. Tobias helped with study design/conduction, patient recruitment, statistical analysis, data interpretation, manuscript preparation and editing. Ismail Bekiroglu helped with study conduct, patient recruitment and manuscript preparation. Julie Rice-Weimer helped study conduct, patient recruitment and manuscript preparation.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Bartels K, Esper SA, Thiele RH. Blood pressure monitoring for the anesthesiologist: a practical review. Anesth Analg. 2016;122(6):1866-1879.
doi pubmed - Kuck K, Baker PD. Perioperative noninvasive blood pressure monitoring. Anesth Analg. 2018;127(2):408-411.
doi pubmed - Saugel B, Sessler DI. Perioperative blood pressure management. Anesthesiology. 2021;134(2):250-261.
doi pubmed - Gleich SJ, Wong AV, Handlogten KS, Thum DE, Nemergut ME. Major short-term complications of arterial cannulation for monitoring in children. Anesthesiology. 2021;134(1):26-34.
doi pubmed - Weiss BM, Gattiker RI. Complications during and following radial artery cannulation: a prospective study. Intensive Care Med. 1986;12(6):424-428.
doi - Furfaro S, Gauthier M, Lacroix J, Nadeau D, Lafleur L, Mathews S. Arterial catheter-related infections in children. A 1-year cohort analysis. Am J Dis Child. 1991;145(9):1037-1043.
doi pubmed - Slogoff S, Keats AS, Arlund C. On the safety of radial artery cannulation. Anesthesiology. 1983;59(1):42-47.
doi pubmed - Jeleazcov C, Krajinovic L, Munster T, Birkholz T, Fried R, Schuttler J, Fechner J. Precision and accuracy of a new device (CNAPTM) for continuous non-invasive arterial pressure monitoring: assessment during general anaesthesia. Br J Anaesth. 2010;105(3):264-272.
doi pubmed - Dewhirst E, Corridore M, Klamar J, Beebe A, Rice J, Barry N, Tobias JD. Accuracy of the CNAP monitor, a noninvasive continuous blood pressure device, in providing beat-to-beat blood pressure readings in the prone position. J Clin Anesth. 2013;25(4):309-313.
doi pubmed - Geddes LA. The direct and indirect measurement of blood pressure. Am Heart J. 1970;80:435-436.
doi - Wagner JY, Grond J, Fortin J, Negulescu I, Schofthaler M, Saugel B. Continuous noninvasive cardiac output determination using the CNAP system: evaluation of a cardiac output algorithm for the analysis of volume clamp method-derived pulse contour. J Clin Monit Comput. 2016;30(4):487-493.
doi pubmed - Biais M, Vidil L, Roullet S, Masson F, Quinart A, Revel P, Sztark F. Continuous non-invasive arterial pressure measurement: evaluation of CNAP device during vascular surgery. Ann Fr Anesth Reanim. 2010;29(7-8):530-535.
doi pubmed - Kako H, Corridore M, Rice J, Tobias JD. Accuracy of the CNAP monitor, a noninvasive continuous blood pressure device, in providing beat-to-beat blood pressure readings in pediatric patients weighing 20-40 kilograms. Paediatr Anaesth. 2013;23(11):989-993.
doi pubmed - Tobias JD, McKee C, Herz D, Teich S, Sohner P, Rice J, Barry N, et al. Accuracy of the CNAP monitor, a noninvasive continuous blood pressure device, in providing beat-to-beat blood pressure measurements during bariatric surgery in severely obese adolescents and young adults. J Anesth. 2014;28(6):861-865.
doi pubmed - ANSI/AAMI. American national standard for manual, electronic, or automated sphygmomanometers. Association for the Advancement of Medical Instrumentation. 2002.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


