| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 9, Number 1, January 2017, pages 30-34
Hyaluronic Acid Fat Graft Myringoplasty Versus Autologous Platelet Rich Plasma
Salman F. Alhabiba, Issam Salibaa, b
aDepartment of Surgery, Division of Otorhinolaryngology, Head & Neck Surgery, Montreal University Hospital Center (CHUM), University of Montreal, Montreal, QC, Canada
bCorresponding Author: Issam Saliba, Division of Otorhinolaryngology, Head & Neck Surgery, CHUM, Hopital Notre Dame, 1560 Sherbrooke East, Montreal, QC, H2L 4M1, Canada
Manuscript accepted for publication November 04, 2016
Short title: HAFGM vs. PRPM
doi: https://doi.org/10.14740/jocmr2800w
| Abstract | ▴Top |
Background: Hyaluronic acid fat graft myringoplasty (HAFGM) is an office-based technique for tympanic membrane perforation (TMP) treatment. It is simple, inexpensive, and performed under local anesthesia at the outpatient office department. We aimed to compare HAFGM technique to a recently described topical use of autologous platelet rich plasma myringoplasty (PRPM) in the repair of TMP. We also aimed to assess the hearing level improvement postoperatively.
Methods: We conducted a prospective study in an adult tertiary care center between January 2015 and January 2016. Adult patients presenting with simple TMP were operated randomly using either HAFGM or PRPM under local anesthesia in an office-based setting. Perforations were classified into four grades. Success was considered when complete closure is achieved. Audiometric parameters were evaluated pre- and postoperatively.
Results: We included 27 patients, of whom 16 were operated with HAFGM and 11 were operated with PRPM. Complete closure was achieved in 81.2% and 18.1%, respectively. Postoperatively, no worsening of bone conduction threshold was noted. The study was abandoned due to the low success rate in patients with PRPM. The pure tone audiometry was improved postoperatively in patients with closed tympanic membrane.
Conclusions: The study was aborted because of the unsatisfactory obtained results using PRPM. It confirms once again the beneficial effect of hyaluronic acid in the healing process when added to fat graft myringoplasty. Furthermore, it requires no hospitalization.
Keywords: Tympanic membrane perforations; Myringoplasty; Hearing loss; Autologous platelet rich plasma; HAFGM
| Introduction | ▴Top |
Tympanic membrane perforation (TMP) is a common otologic problem leading to a conductive hearing loss. TMP heals spontaneously without surgical procedure in 88% of the patients [1]. A persistent TMP increases the patient’s risk of developing recurrent acute otitis media or chronic middle ear disease. These conditions are frequently associated with an unpleasant otorrhea. The myringoplasty is a surgical procedure that closes a simple perforated tympanic membrane without elevating the annulus [2]. The aim of this procedure is to create an intact tympanic membrane, forming a dry ear and no further need to protect the ear from water after complete healing. However, the complications of myringoplasty include anterior blunting, tympanic membrane lateralization, stenosis of the external ear canal, delayed healing, epithelial pearls, and a risk of inclusion iatrogenic cholesteatoma [3].
The senior author introduced in 2008 a novel technique to repair all sizes of TMP by combining hyaluronic acid to fat graft myringoplasty (HAFGM) [4]. In this simple office-based technique, performed under local anesthesia, he achieved a global success rate of 92.7% in adults and 87% in children [5-7]. Hyaluronic acid seems to play an important role during the healing process [8].
In a recent study, El-Anwar and El-Ahl [9] described a myringoplasty under general anesthesia using autologous platelet rich plasma (PRP) with perichondrium graft. They operated 64 patients for tympanoplasty with perichondrium graft, then they used the PRP as dressing lateral to perforated tympanic membrane and they compared it with another group where they used gelfoam as dressing. They had a success rate of 100% closure of tympanic membrane with PRP in 32 patients compared to 81% closure of tympanic membrane with gelfoam in 32 patients in control group [9].
The aim of this study was to compare the HAFGM technique with PRPM without perichondrium graft in an attempt to spare the financial cost of hyaluronic acid and to avoid additional scar in the neck. Our aim was also to assess hearing improvement 6 and 12 months after the surgery.
| Patients and Methods | ▴Top |
A prospective study was conducted at our tertiary care center between January 2015 and January 2016. Patients were well operated under local anesthesia in an outpatient setting. Patients were assigned randomly to HAFGM (group I) and PRPM (group II).
Inclusion criteria were: 1) perforations present for at least 12 months, 2) no cholesteatoma, retraction pocket formation, or chronic otitis media, and 3) an air-bone gap (ABG) of 40 dB or better.
We excluded all patients with purulent discharge, suspected ossicular disease, uncontrolled retraction pocket and cholesteatoma. Sizes of the TMP were graded according to Saliba classification: 1) grade I: small, less than 25% of the tympanic membrane surface, 2) grade II: medium, 25-50% of the tympanic membrane surface, 3) grade III: large, 50-75% of the tympanic membrane surface, and 4) grade IV: total, more than 75% of the tympanic membrane surface [3].
Surgical technique
All patients, in both groups, were operated in an outpatient setting in a sterile environment. Local anesthesia was achieved by injecting 1% xylocaine with 1:100,000 epinephrine in the four quadrant of external auditory canal (EAC). In group I, the fat graft was harvested as previously described through a 5 mm incision under local anesthesia between the paravertebral midline and the posterior limit of the sternocleidomastoid muscle [6]. The fat was introduced through the perforation after trimming the perforated edge. Hyaluronic acid EpiDisc® (EpiDisc® Otologic Lamina; Xomed-Medtronic, Jacksonville, FL, USA) was applied over the fat graft and the remnants of the tympanic membrane. Care was taken to make an intimate contact of the hyaluronic acid lamina and the fat graft without excessive pressure. One to four hyaluronic acid was used depending on the size of the TMP. Pieces of gelfoam soaked with ofloxacin were used to pack over the hyaluronic aci and to fill all the EAC. Postoperatively, patients were discharged immediately and instructed to keep their ears dry, to avoid plane traveling, and to prevent strong nose blowing for 2 months.
In group II, 15 mL of peripheral venous blood was drawn from the patient with a 16-gauge needle and collected in three plain vacuum tubes without an anticoagulant (5 mL per tube), and then the tubes were immediately centrifuged using a tabletop centrifuge machine for 12 - 30 min at 3,200 rpm. Blood was separated into three layers: the bottom layer consists of red blood cells, the middle layer contains PRP, which is composed of platelets and white blood cells (WBCs; buffy coat) that could be easily obtained and the top layer contains platelet poor plasma (Fig. 1). PRP was inserted through the perforation toward the middle ear, after trimming the perforated edge, as an hourglass shaped blog. Then we covered the repaired perforation and tympanic membrane remnant by another piece of PRP. A piece of gelfoam was used to pack over the PRP and the EAC. Postoperatively, patients were discharged immediately with oral antibiotic and instructed to keep their ears dry, to avoid plane traveling, and to prevent strong nose blowing for 2 months.
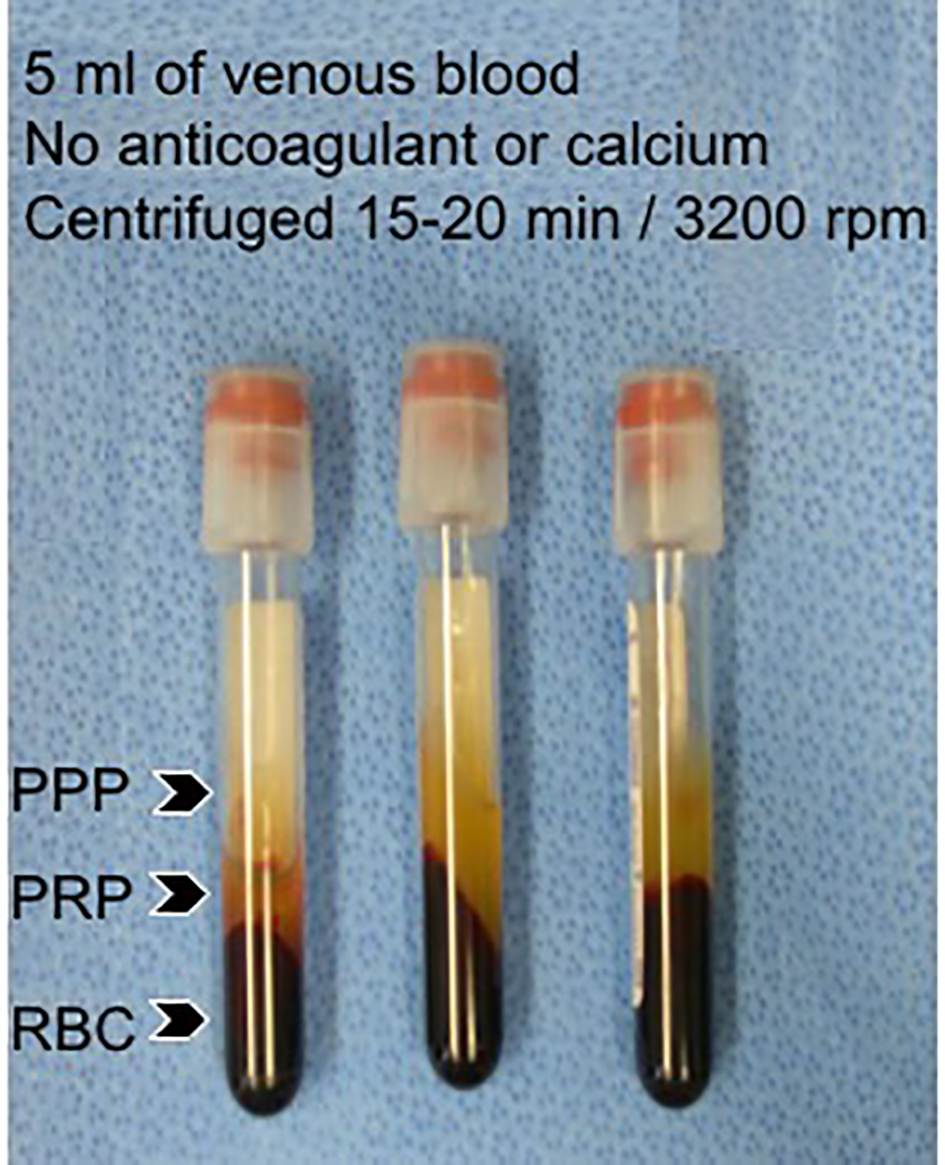 Click for large image | Figure 1. After centrifugation blood was separated into three layers: the bottom layer consists of red blood cells, the middle layer contains platelet poor plasma (PRP), which is composed of platelets and white blood cells (WBCs), and the top layer contains platelet poor plasma (PPP). |
Statistical analysis
SPSS statistics® version 20 (Chicago, IL, USA) was used for statistical analysis. Fisher’s exact test was used to detect differences in tympanic membrane closure and the Student’s t-test was used for audiometric comparison. Calculated P-value < 0.05 was considered statistically significant.
| Results | ▴Top |
We included 27 patients, of whom 16 were operated with HAFGM and 11 patients were operated with PRPM. The PRPM technique was aborted as unsatisfied results. The HAFGM success rate was 81.2% compared to 18.1% for the PRP group (P > 0.001). There were no influences of age, sex, or any previous ear surgery (Table 1). The size of TMP did not influence the success rate (Table 2). Myringitis and two pearls of cholesteatoma were found in three patients operated with PRPM technique. However, the tympanic membrane in HAFGM technique was characterized by a new epithelization and new vascularization, which restore the tympanic membrane integrity and function. Pre- and postoperative hearing results are listed in Table 3. There was no significant difference in the result of bone conduction audiometry or speech discrimination score 6 and 12 months postoperatively on both groups. Better pure tone average (PTA) was statistically significant at 6 and 12 months postoperatively (P = 0.0001) in HAFGM and not in PRPM group (P = 0.93). The ABG was improved at 6 and 12 months postoperatively in the HAFGM group (at 6 months, P = 0.0004, at 12 months, P = 0.001), where the ABG of PRPM was not improved postoperatively. The hearing improvement when comparing the two groups was better in the HAFGM group (P = 0.03).
 Click to view | Table 1. Demographic Data |
 Click to view | Table 2. Success Rates According to the Size of Tympanic Membrane Perforation |
 Click to view | Table 3. Audiometric Results |
| Discussion | ▴Top |
Simple tympanoplasty in the office under local anesthesia is gaining the interest in the past few decades as they are cost effective and without the need of hospital admission. On the other hand, results should be comparable to conventional tympanoplasty either under local or general anesthesia.
Hyaluronic acid is a natural component of extracellular matrix of many body tissues. Hyaluronic acid stimulates the endogenous growth factor, epidermal growth factor, insulin growth factor, tumor necrosis factor, and vascular endothelial growth factor in a reported animal study [10]. It plays a role in fibrous tissue regeneration and regulation during healing process of tympanic membrane [11-13]. It promotes the centripetal migration of epithelial tissue over the temporary fat graft support [12]. Many studies [1, 11-14] showed that these factors promote the revascularization, cell growth and differentiation during healing process of tympanic membrane. Review studies show the success rate of HAFGM in adult and children (Table 4) [4-7, 15, 16]. Fat graft myringoplasty (FGM) was described by Ringenberg [17] in 1962 with success rate varying in literature between 56% and 92%. We compared previously the FGM to the HAFGM in pediatric small TMP with a success rate of 57.1% and 90%, respectively. Then we compared it with a fat-FGM (F-FGM) that was described by Koc et al [18] and our success rate with HAFGM was 80% vs. 42.8% for the F-FGM [15].
 Click to view | Table 4. Review Studies Show the Success Rates of HAFGM |
PRP is defined as a volume of plasma having a platelet concentration above baseline levels. Mixture of calcium and PRP results in release of growth factors, forming a gel structure [19]. Erkilet and Koyuncu were the first to study the rapidity of healing process of traumatic tympanic membrane with and without application of PRP on 44 healthy Sprague-Dawley rats [19]. The control group was the left ear and the PRP group was the right ear. TMP healing was achieved in both groups but it was faster in the PRP group (P < 0.001) compared to the naturally tympanic membrane healing in the control group. The author concludes the effectiveness of PRP application in an attempt to have a successful tympanic membrane closure. In our study, the TMPs present for at least 12 months and they were secondary to chronic ear infection. The two cases of PRPM technique with success were characterized by a weak membrane that has a tendency to retract medially (Fig. 2). This could explain the high failure rate of this technique and increase the risk of re-perforation. Unfortunately, the PRP technique without fat graft or facia shows a success rate of 18.1% compared to 81.2% in HAFGM group (Fig. 3). PTA and ABG were improved 6 and 12 months postoperatively in HAFGM and not in PRPM and this is a result of successful tympanic membrane vibration as most of the patients in HAFGM group had a complete closure of tympanic membrane. However, for the two successful cases of PRPM, the ABG differences postoperatively reach 16 and 3 dB. In front of this very low success rate of PRPM, the study was aborted, as it was unethical to continue the study.
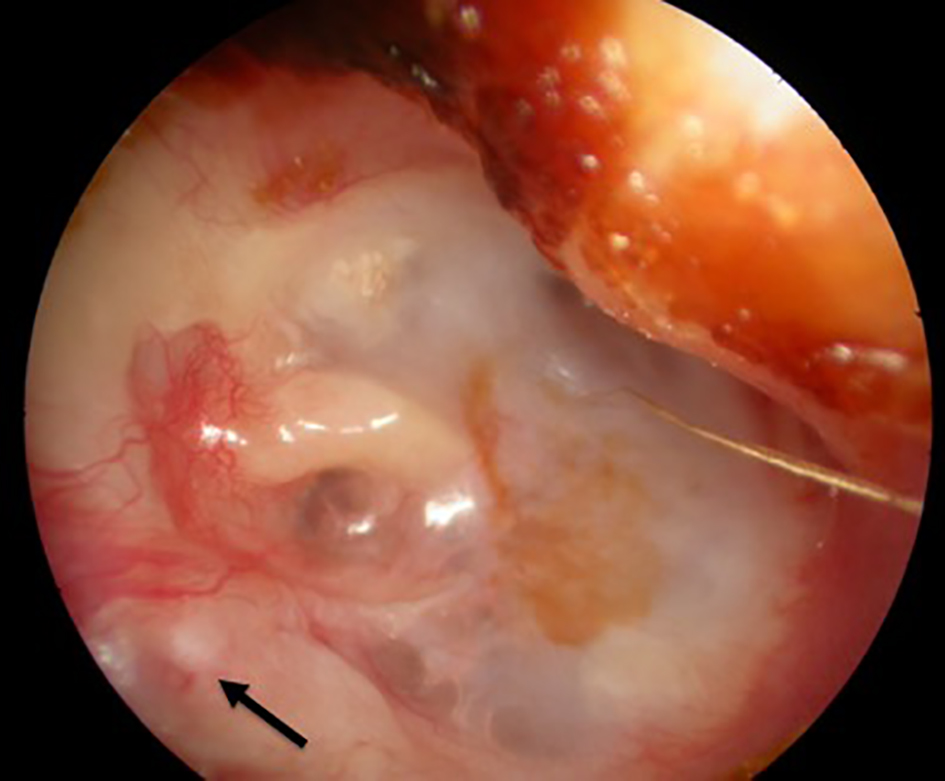 Click for large image | Figure 2. Right ear operated with PRPM technique shows postero-superiorly retracted healed tympanic membrane at 6 months postoperatively with external auditory canal pearl of cholesteatoma (arrow). |
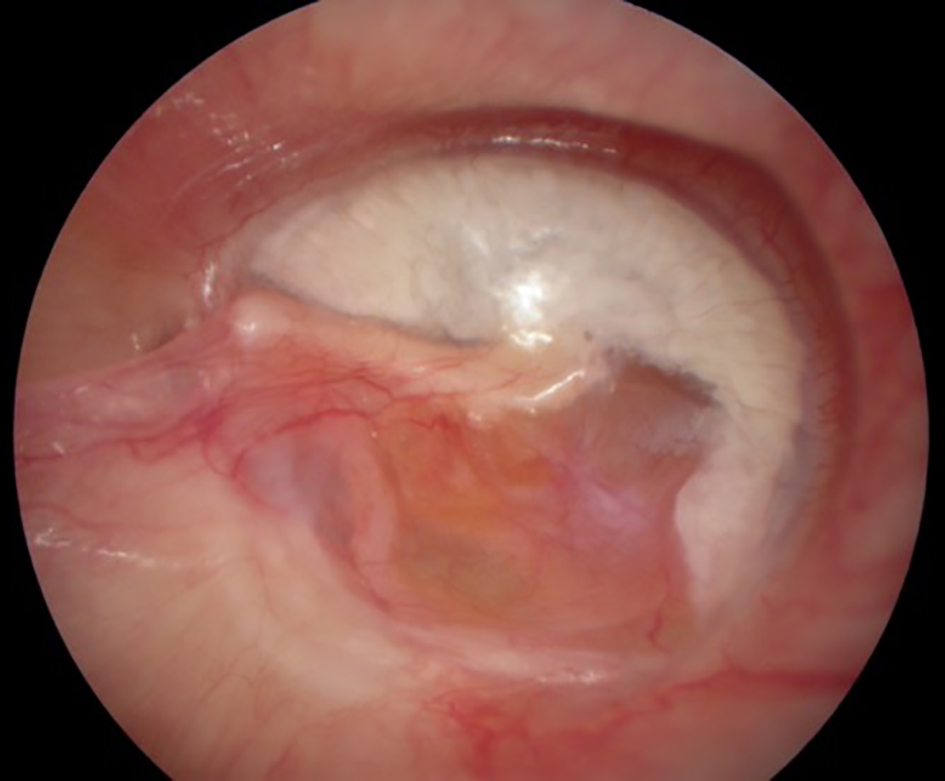 Click for large image | Figure 3. Right ear operated with HAFGM technique shows the healed tympanic membrane at 12 months postoperatively. We can identify the corda tympani through the new ear drum. |
Conclusion
PRPM shows a success rate not reaching 20%. The study was abandoned due to the unsatisfactory obtained results. However, it confirms once again the anatomical and audiological beneficial effect of HAFGM of an office-based technique performed under local anesthesia. Furthermore, it requires no hospitalization.
Financial Disclosure
None.
Conflicts of Interest
None.
| References | ▴Top |
- Amoils CP, Jackler RK, Lustig LR. Repair of chronic tympanic membrane perforations using epidermal growth factor. Otolaryngol Head Neck Surg. 1992;107(5):669-683.
doi pubmed - Sckolnick JS, Mantle B, Li J, Chi DH. Pediatric myringoplasty: factors that affect success-a retrospective study. Laryngoscope. 2008;118(4):723-729.
doi pubmed - Mokhtarinejad F, Okhovat SA, Barzegar F. Surgical and hearing results of the circumferential subannular grafting technique in tympanoplasty: a randomized clinical study. Am J Otolaryngol. 2012;33(1):75-79.
doi pubmed - Saliba I. Hyaluronic acid fat graft myringoplasty: how we do it. Clin Otolaryngol. 2008;33(6):610-614.
doi pubmed - Saliba I, Froehlich P. Hyaluronic acid fat graft myringoplasty: an office-based technique adapted to children. Arch Otolaryngol Head Neck Surg. 2011;137(12):1203-1209.
doi pubmed - Saliba I, Knapik M, Froehlich P, Abela A. Advantages of hyaluronic acid fat graft myringoplasty over fat graft myringoplasty. Arch Otolaryngol Head Neck Surg. 2012;138(10):950-955.
doi pubmed - Saliba I, Woods O. Hyaluronic acid fat graft myringoplasty: a minimally invasive technique. Laryngoscope. 2011;121(2):375-380.
doi pubmed - Laurent TC, Fraser JR. Hyaluronan. FASEB J. 1992;6(7):2397-2404.
pubmed - El-Anwar MW, El-Ahl MA, Zidan AA, Yacoup MA. Topical use of autologous platelet rich plasma in myringoplasty. Auris Nasus Larynx. 2015;42(5):365-368.
doi pubmed - Saliba I, Alzahrani M, Zhu T, Chemtob S. Growth factors expression in hyaluronic acid fat graft myringoplasty. Laryngoscope. 2014;124(6):E224-230.
doi pubmed - Chauvin K, Bratton C, Parkins C. Healing large tympanic membrane perforations using hyaluronic acid, basic fibroblast growth factor, and epidermal growth factor. Otolaryngol Head Neck Surg. 1999;121(1):43-47.
doi - Guneri EA, Tekin S, Yilmaz O, Ozkara E, Erdag TK, Ikiz AO, Sarioglu S, et al. The effects of hyaluronic acid, epidermal growth factor, and mitomycin in an experimental model of acute traumatic tympanic membrane perforation. Otol Neurotol. 2003;24(3):371-376.
doi pubmed - McCarty MF. Glucosamine for wound healing. Med Hypotheses. 1996;47(4):273-275.
doi - Hakuba N, Iwanaga M, Tanaka S, Hiratsuka Y, Kumabe Y, Konishi M, Okanoue Y, et al. Basic fibroblast growth factor combined with atelocollagen for closing chronic tympanic membrane perforations in 87 patients. Otol Neurotol. 2010;31(1):118-121.
doi pubmed - Alzahrani M, Saliba I. Hyaluronic acid fat graft myringoplasty vs fat patch fat graft myringoplasty. Eur Arch Otorhinolaryngol. 2015;272(8):1873-1877.
doi pubmed - Gun T, Boztepe OF, Atan D, Ikinciogullari A, Dere H. Comparison of Hyaluronic Acid Fat Graft Myringoplasty, Fat Graft Myringoplasty and Temporal Fascia Techniques for the Closure of Different Sizes and Sites of Tympanic Membrane Perforations. J Int Adv Otol. 2016;12(2):137-141.
doi pubmed - Ringenberg JC. Fat graft tympanoplasty. Laryngoscope. 1962;72:188-192.
doi pubmed - Koc S, Akyuz S, Gurbuzler L, Aksakal C. Fat graft myringoplasty with the newly developed surgical technique for chronic tympanic membrane perforation. Eur Arch Otorhinolaryngol. 2013;270(5):1629-1633.
doi pubmed - Erkilet E, Koyuncu M, Atmaca S, Yarim M. Platelet-rich plasma improves healing of tympanic membrane perforations: experimental study. J Laryngol Otol. 2009;123(5):482-487.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


