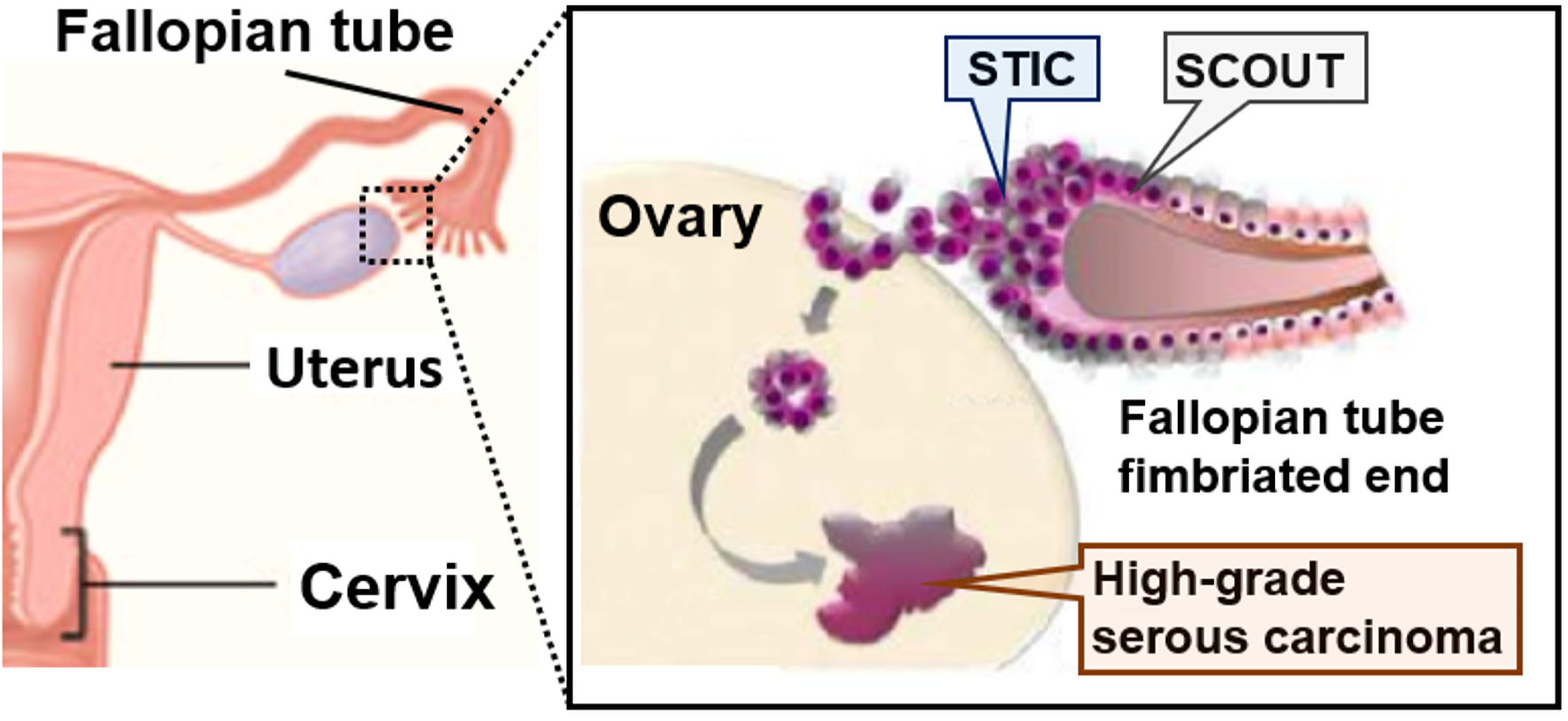
Figure 1. Fallopian tube hypothesis on the origin of high-grade serous carcinoma (HGSC). Fallopian tube epithelium cells of the fimbriated ends undergo initial neoplastic transformation and become serous tubal intraepithelial carcinoma (STIC). STIC cells are resistant to anoikis, which favors settlement and ovarian surface invasion. The ovarian microenvironment, rich in hormonal and inflammatory factors, drives the full neoplastic transformation to invasive high-grade serous carcinoma (HGSC). SCOUT: secretory cell out-growth.