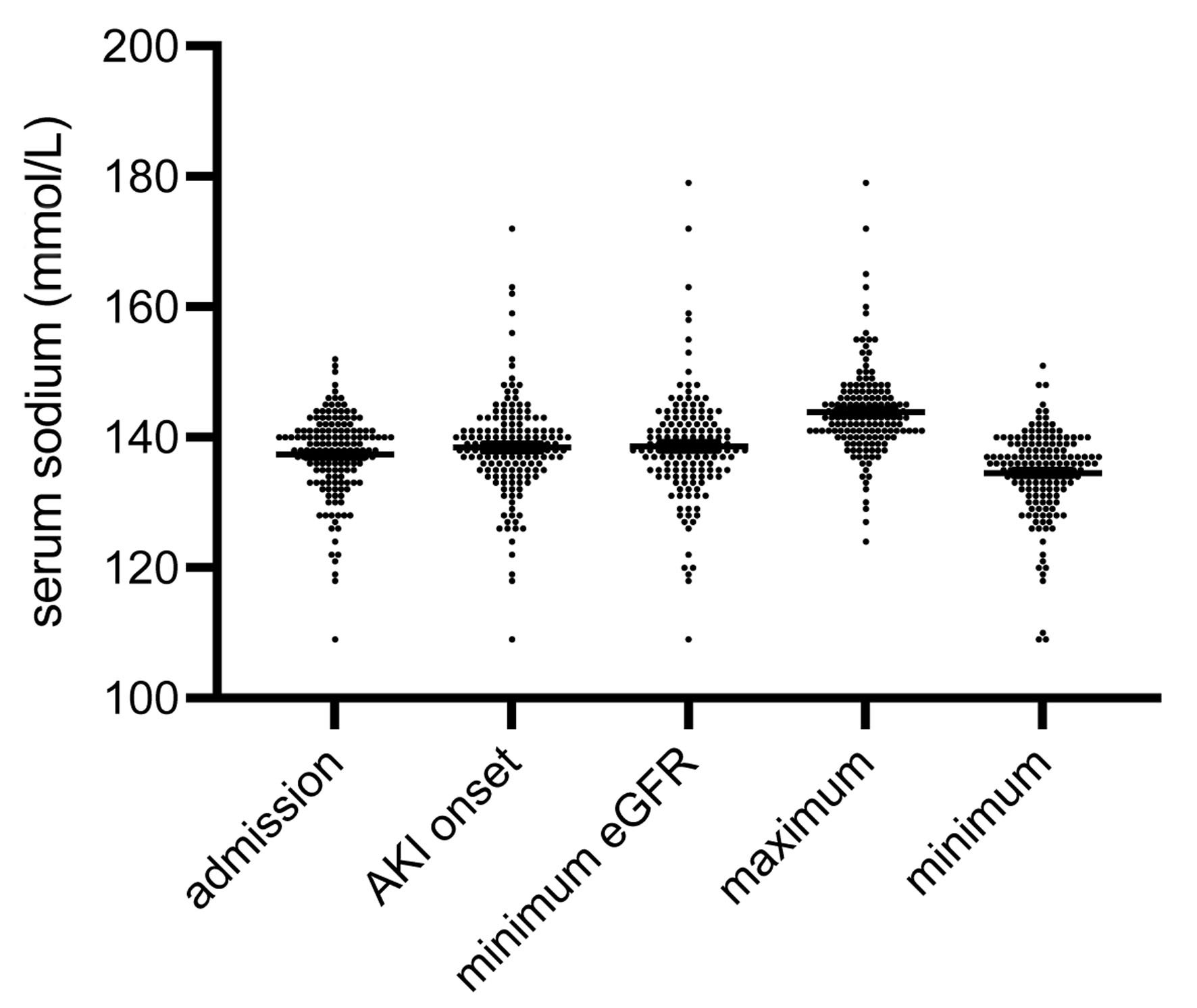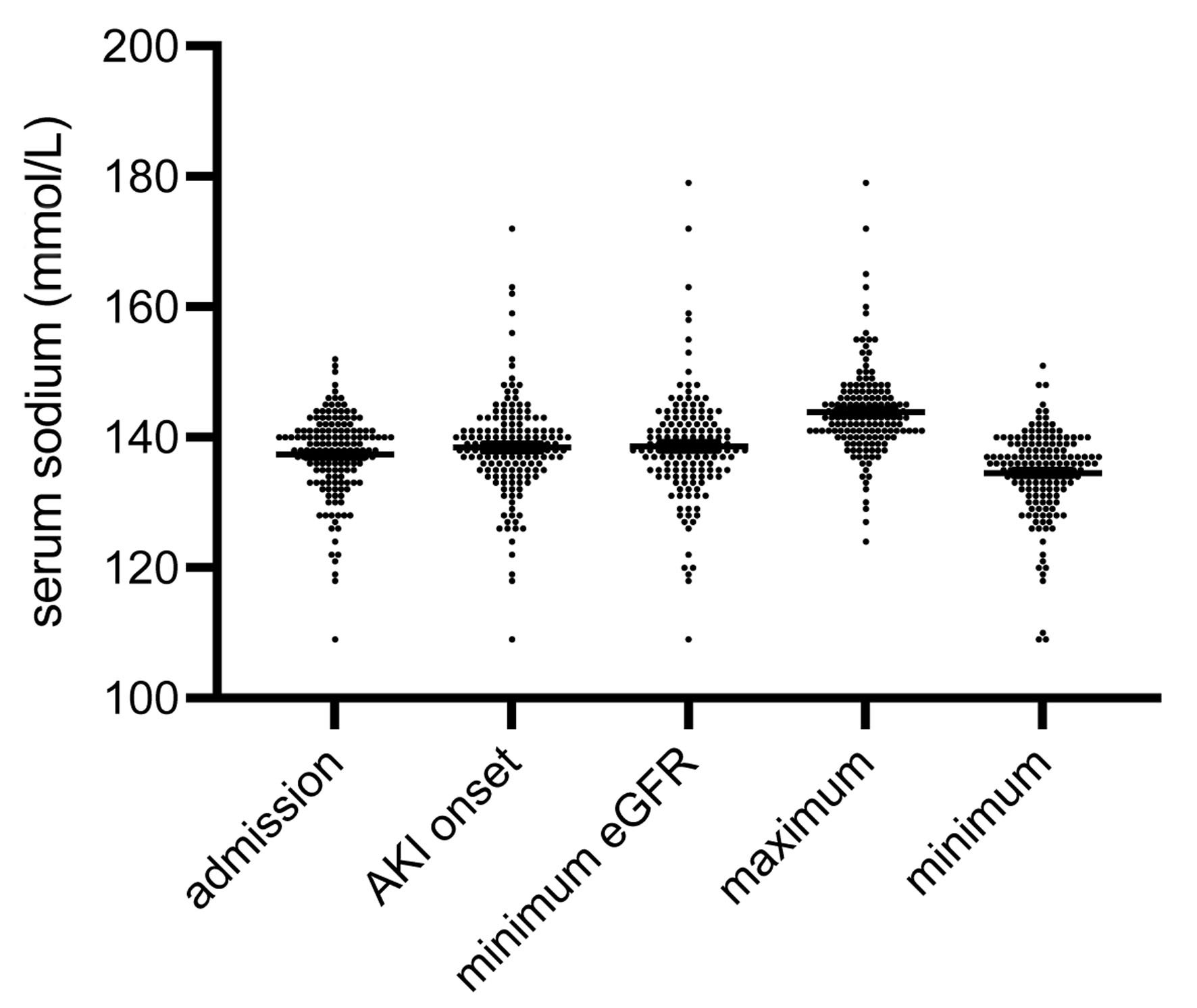
Figure 1. Distribution of serum sodium at five pre-defined time points: admission to the hospital, diagnosis of AKI (AKI onset), minimum eGFR, maximum and minimum of serum sodium, respectively. The medians were not equal (P < 0.001). The numbers of all outliers per group were: admission 1, AKI onset 6, minimum eGFR 6, maximum 5, minimum 3 (data are shown as median ± IQR). AKI: acute kidney injury; eGFR: estimated glomerular filtration rate; IQR: interquartile range.
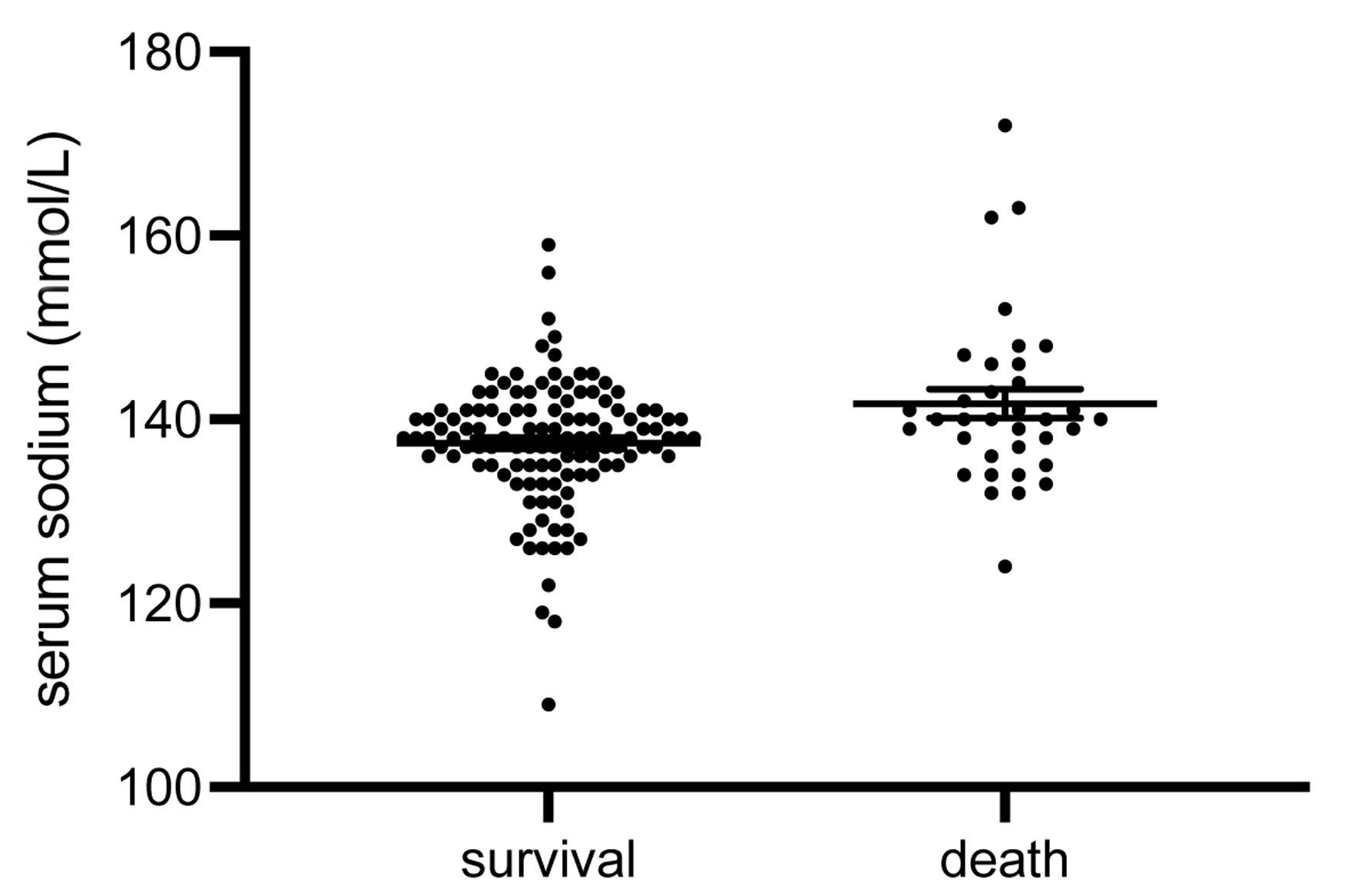
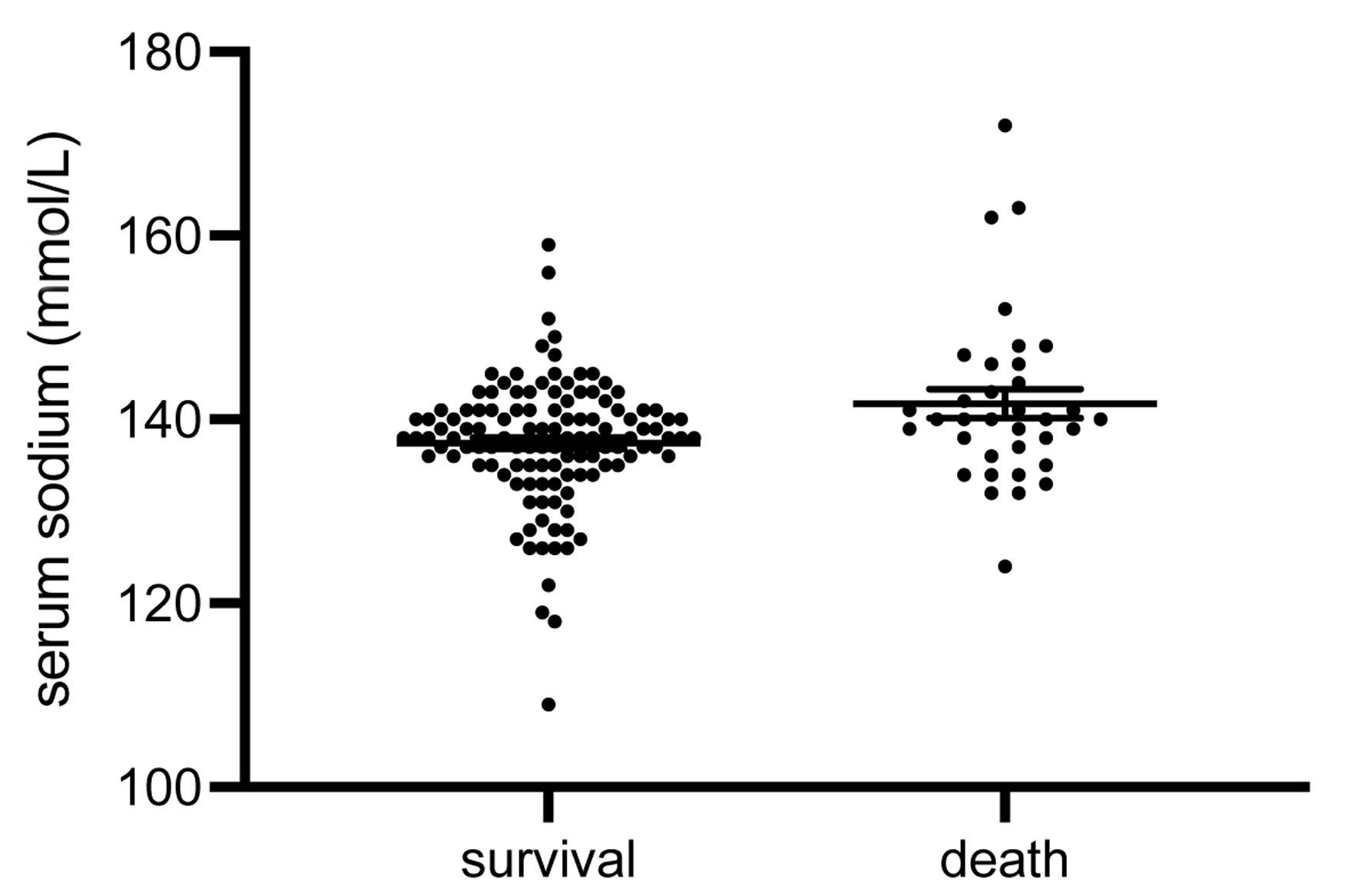
Figure 2. Serum sodium at AKI diagnosis. Subjects that did not survive the in-hospital treatment period showed significantly higher serum sodium levels at AKI onset (P = 0.003). The numbers of all outliers per group were: survival 4, death 1 (data are shown as median ± IQR). AKI: acute kidney injury; IQR: interquartile range.
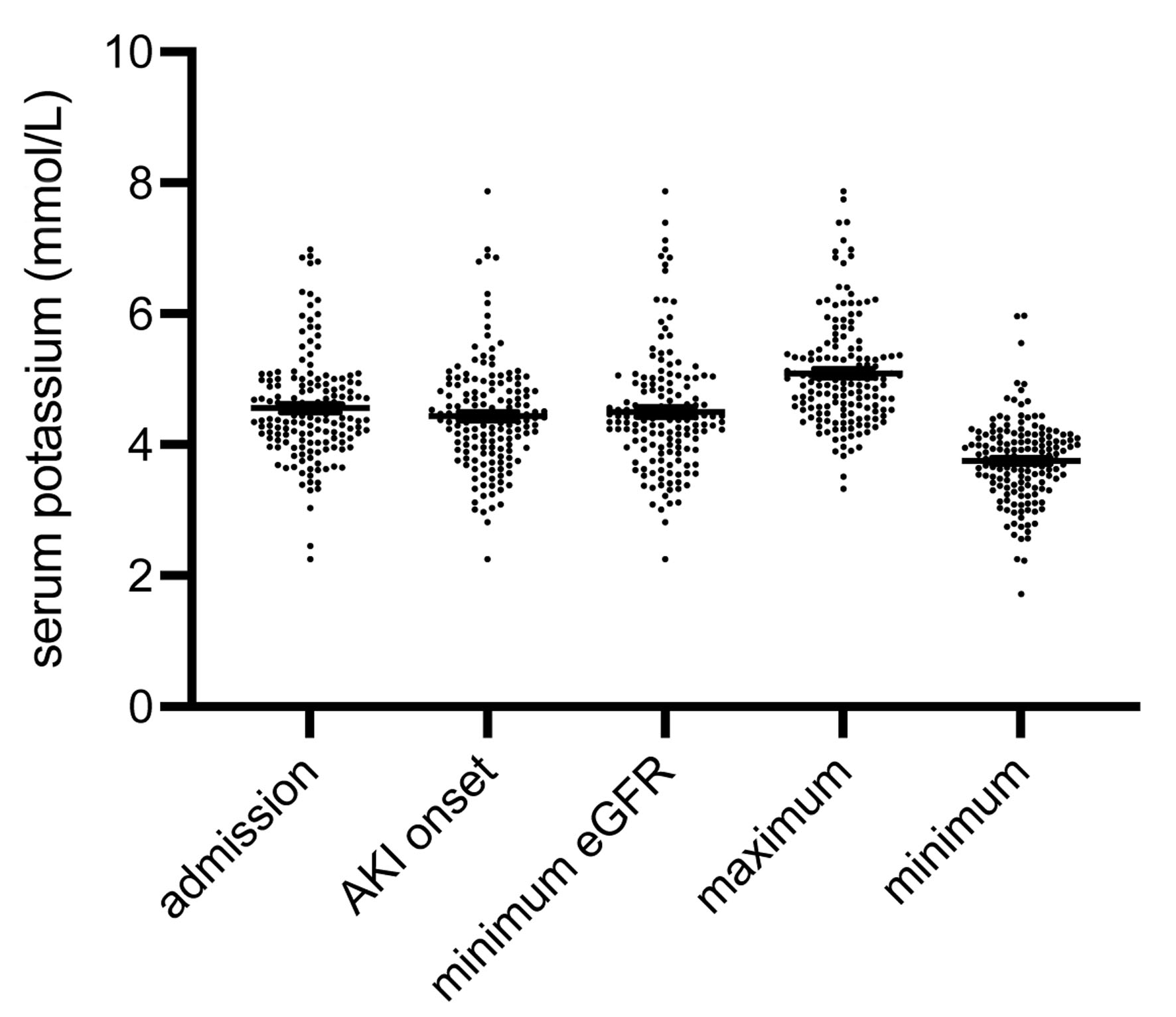
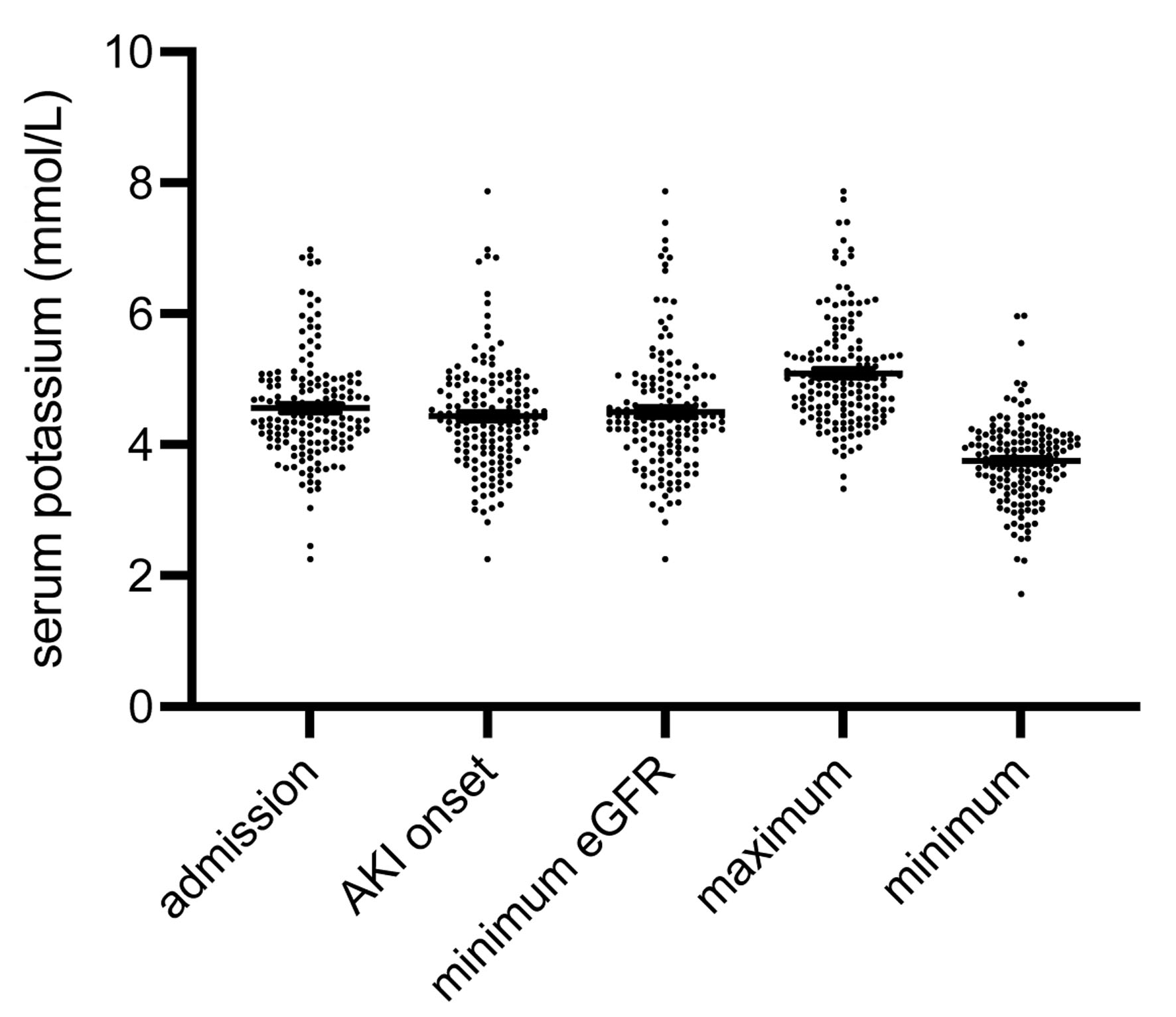
Figure 4. Distribution of serum potassium at the five time points (Fig. 2). Comparable to serum sodium, the respective medians were not equal (P < 0.001). The numbers of all outliers per group were: admission 5, AKI onset 1, minimum eGFR 2, maximum 2, minimum 3 (data are shown as median ± IQR). AKI: acute kidney injury; eGFR: estimated glomerular filtration rate; IQR: interquartile range.