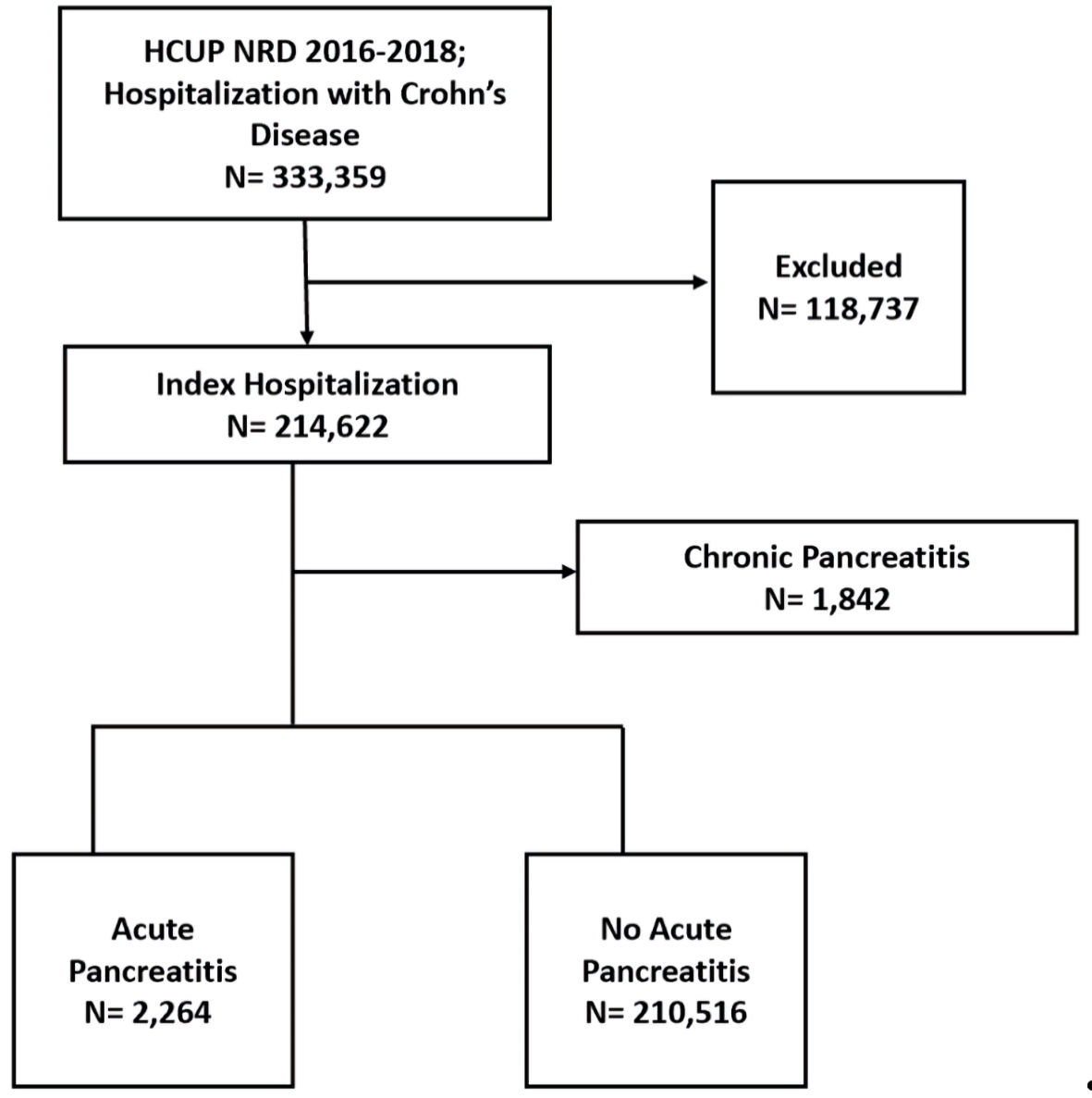
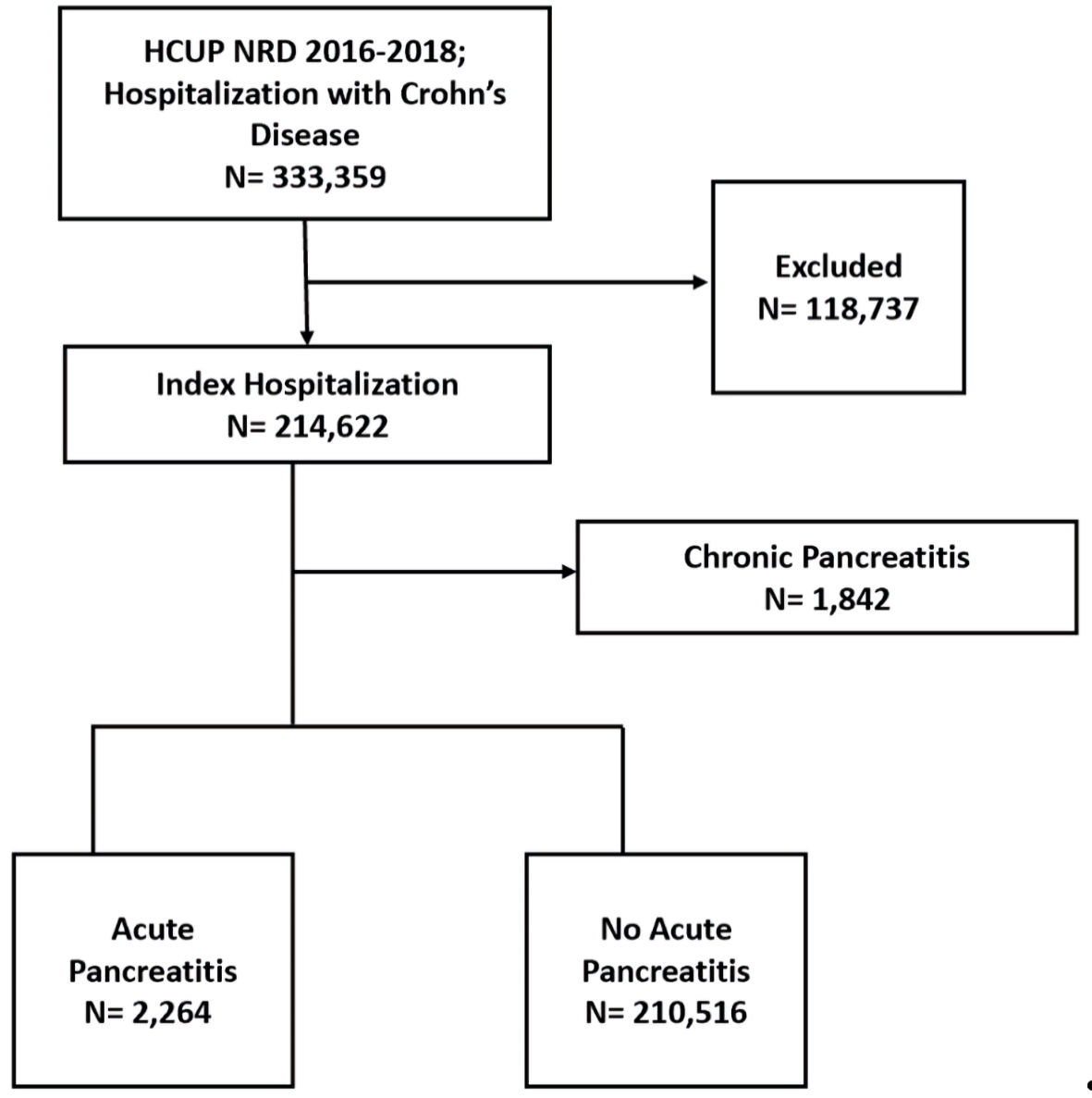
Figure 1. Case selection flowchart. HCUP: the Healthcare Cost and Utilization Project; NRD: Nationwide Readmissions Database.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 8, August 2022, pages 293-299
Prevalence and Impact of Acute Pancreatitis on Hospitalization Outcomes in a Cohort of Patients With Crohn’s Disease
Figure
Tables
| AP absent (n = 210,516) | AP present (n = 2,264) | P value | |
|---|---|---|---|
| AP: acute pancreatitis; IQR: interquartile range; ESRD: end-stage renal disease; NAFLD: nonalcoholic fatty liver disease; PBC: primary biliary cirrhosis; PSC: primary sclerosing cholangitis. | |||
| Median age, n (IQR) | 53 (36 - 68) | 51 (38 - 64) | 0.003 |
| Age group, n (%) | |||
| 18 - 44 | 77,815 (37) | 814 (36) | < 0.001 |
| 45 - 64 | 68,780 (32.7) | 923 (40.8) | |
| 65 or older | 63,921 (30.4) | 527 (23.3) | |
| Sex, n (%) | |||
| Male | 88,798 (42.2) | 972 (42.9) | 0.471 |
| Female | 121,718 (57.8) | 1,292 (57.1) | |
| Median household income for patient’s ZIP code, n (%) | |||
| 0 - 25th percentile | 48,943 (23.2) | 577 (25.5) | 0.015 |
| 26th - 50th percentile | 55,798 (26.5) | 616 (27.2) | |
| 51st - 75th percentile | 55,910 (26.6) | 586 (25.9) | |
| 76th - 100th percentile | 49,865 (23.7) | 485 (21.4) | |
| Bed size of the hospital, n (%) | |||
| Small | 33,286 (15.8) | 421 (18.6) | < 0.001 |
| Medium | 58,752 (27.9) | 689 (30.4) | |
| Large | 118,478 (56.3) | 1,154 (51) | |
| Insurance, n (%) | |||
| Medicare | 84,990 (40.4) | 784 (34.6) | < 0.001 |
| Medicaid | 30,336 (14.4) | 393 (17.4) | |
| Private insurance | 80,711 (38.3) | 904 (39.9) | |
| Self-pay | 7,620 (3.6) | 111 (4.9) | |
| No charge | 5,788 (2.7) | 61 (2.7) | |
| Other | 1,071 (0.5) | 11 (0.5) | |
| Hypertension, n (%) | 63,054 (30) | 774 (34.2) | < 0.001 |
| Diabetes mellitus, n (%) | 32,457 (15.4) | 423 (18.7) | < 0.001 |
| Obesity, n (%) | 24,818 (11.8) | 310 (13.7) | 0.005 |
| Dyslipidemia, n (%) | 44,761 (21.3) | 516 (22.8) | 0.077 |
| ESRD, n (%) | 3,041 (1.4) | 30 (1.3) | 0.635 |
| Acute kidney failure, n (%) | 28,608 (13.6) | 404 (17.8) | < 0.001 |
| NAFLD, n (%) | 4,894 (2.3) | 218 (9.6) | < 0.001 |
| PBC, n (%) | 133 (0.1) | 3 (0.1) | 0.194 |
| PSC, n (%) | 53 (0.03) | 2 (0.1) | 0.063 |
| Gallstone disease, n (%) | 2,467 (1.2) | 121 (5.3) | < 0.001 |
| Hepatic failure, n (%) | 1,604 (0.8) | 41 (1.8) | < 0.001 |
| Thrombocytopenia, n (%) | 7,825 (3.7) | 127 (5.6) | < 0.001 |
| Hypercalcemia, n (%) | 1,029 (0.5) | 24 (1.1) | < 0.001 |
| Hypokalemia, n (%) | 34,391 (16.3) | 606 (26.8) | < 0.001 |
| Etiology | Acute pancreatitis (n = 2,264) |
|---|---|
| Idiopathic acute pancreatitis | 89 (3.9%) |
| Biliary acute pancreatitis | 360 (15.9%) |
| Alcohol-induced acute pancreatitis | 252 (11.1%) |
| Drug-induced acute pancreatitis | 183 (8.1%) |
| Unspecified acute pancreatitis | 1,380 (61%) |
| 30-day readmission primary diagnosis | Rate |
|---|---|
| Acute pancreatitis | 27.1 |
| Crohn’s disease | 13 |
| Sepsis | 9.7 |
| Acute kidney failure | 5.8 |
| Clostridium difficile enterocolitis | 1.9 |
| Pseudocyst of pancreas | 1.4 |
| Ileus | 1.4 |
| Dehydration | 1.4 |
| Urinary tract infection | 1 |
| Peritoneal adhesions | 1 |
| Predictor | P value | Odds ratio | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| CI: confidence interval; NAFLD: nonalcoholic fatty liver disease. | ||||
| Age (years) | ||||
| 18 - 44 | Reference | |||
| 45 - 64 | 0.404 | 1.045 | 0.944 | 1.155 |
| ≥ 65 | < 0.001 | 0.639 | 0.567 | 0.72 |
| Diabetes mellitus | 0.002 | 1.196 | 1.069 | 1.337 |
| Hypertension | < 0.001 | 1.199 | 1.092 | 1.316 |
| Gallstone disease | < 0.001 | 4.047 | 3.343 | 4.9 |
| NAFLD | < 0.001 | 3.568 | 3.08 | 4.133 |
| Hepatic failure | 0.014 | 1.505 | 1.086 | 2.086 |
| Acute kidney failure | < 0.001 | 1.288 | 1.149 | 1.444 |
| Hypercalcemia | 0.001 | 1.964 | 1.302 | 2.965 |
| Hypokalemia | < 0.001 | 1.741 | 1.583 | 1.915 |
| Thrombocytopenia | 0.031 | 1.236 | 1.024 | 1.49 |