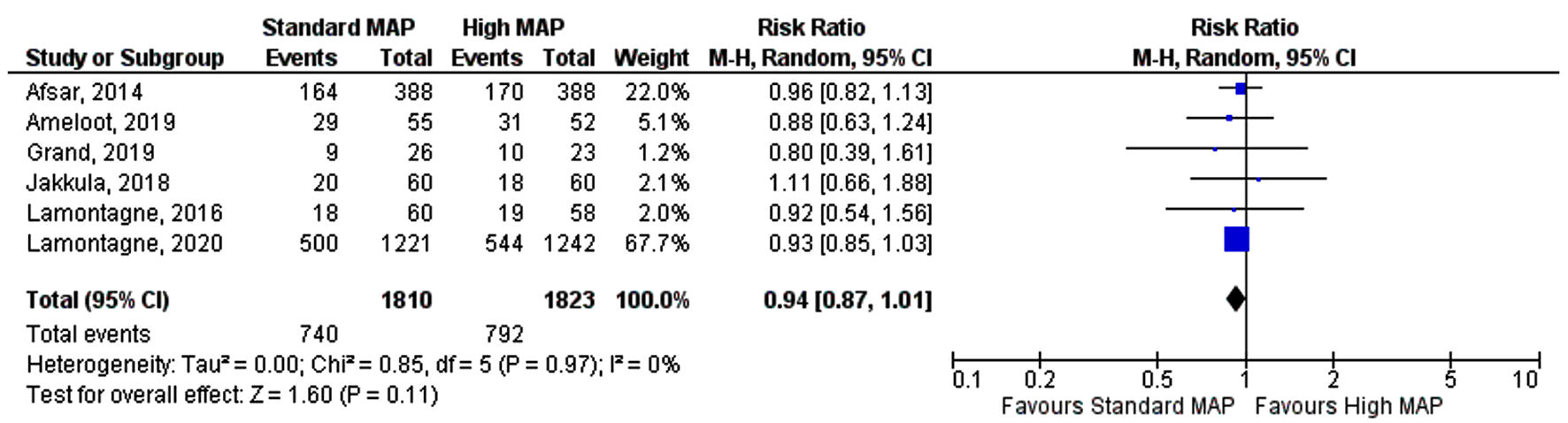
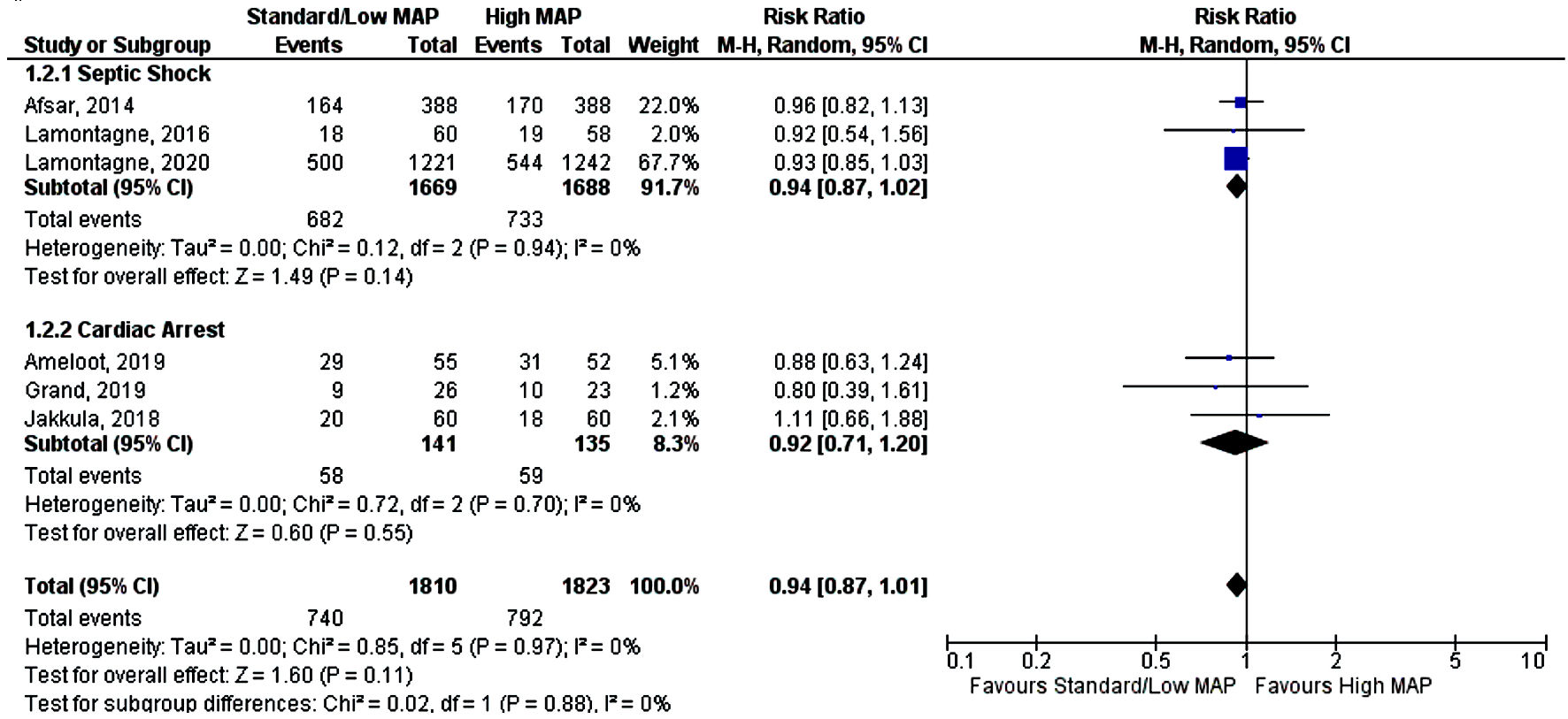
Figure 1. Forest plot showing risk ratio of overall mortality. MAP: mean arterial pressure; CI: confidence interval.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 5, May 2022, pages 196-201
Mean Arterial Pressure Goal in Critically Ill Patients: A Meta-Analysis of Randomized Controlled Trials
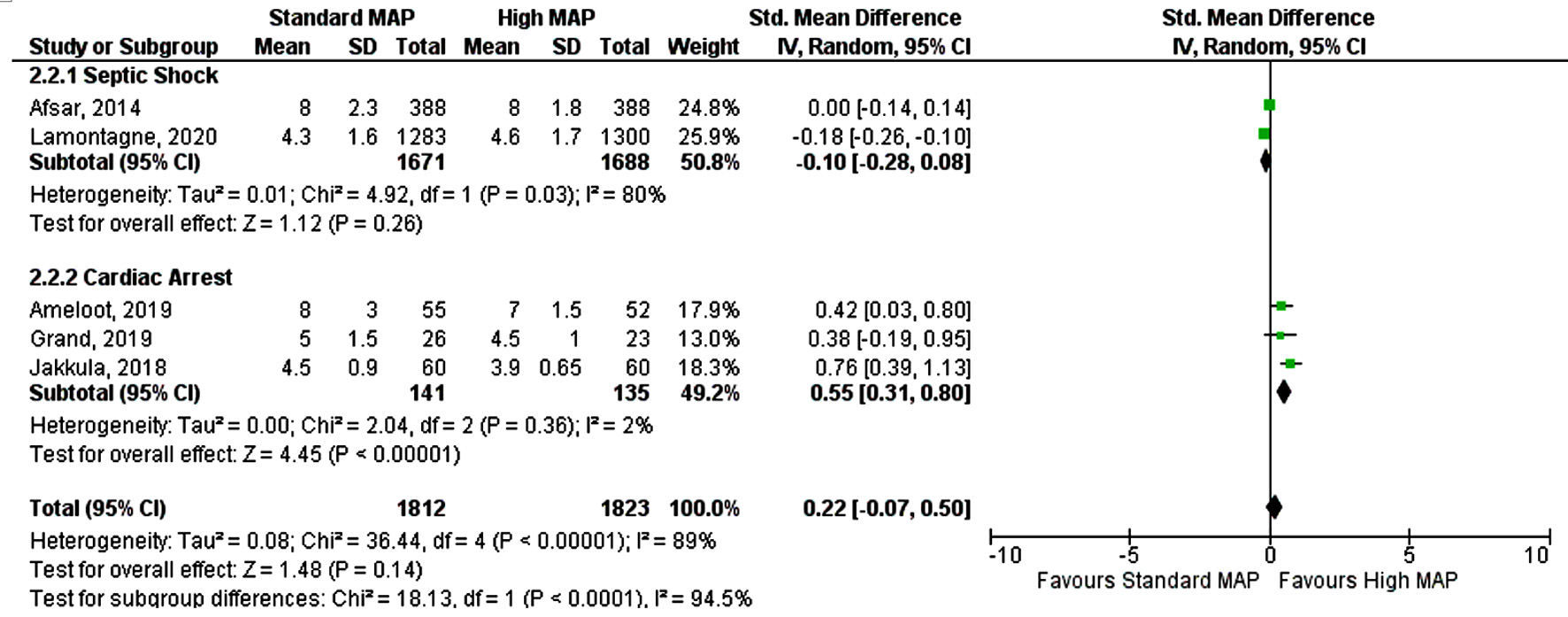
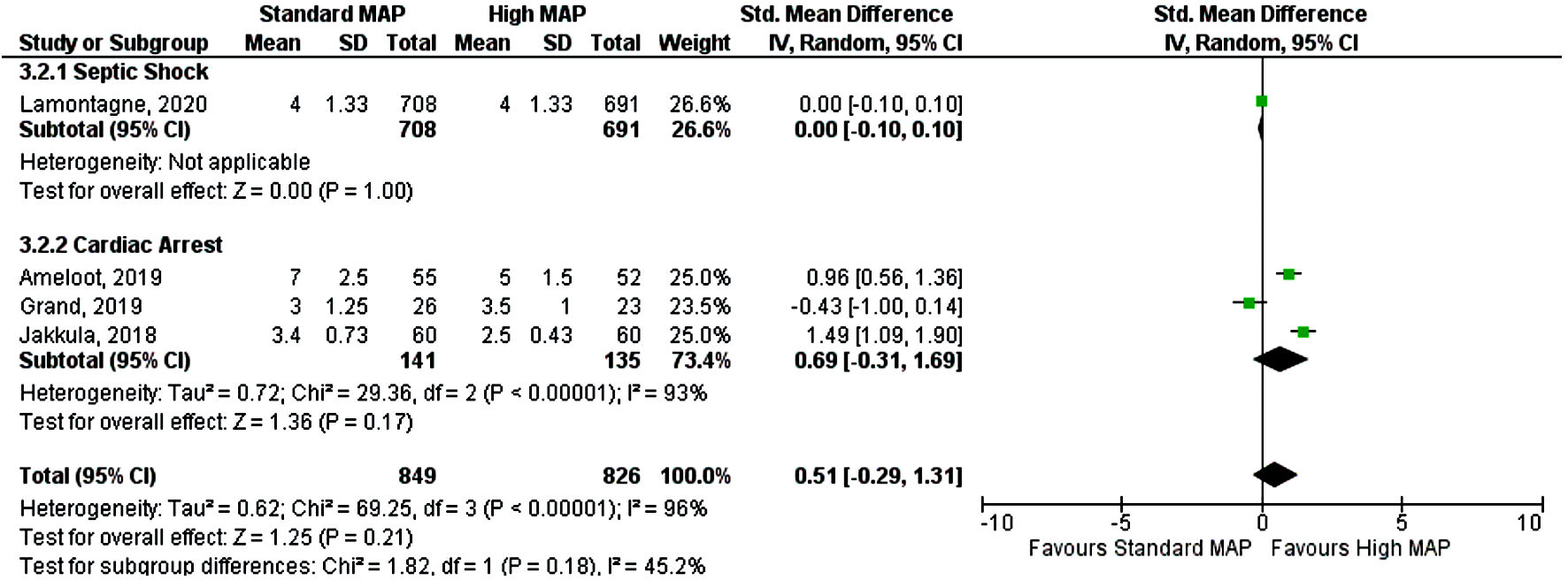
Figures
Table
| Study (year) | N (patientsa) | Follow-up (months) | Major inclusion criteria | Major exclusion criteria | Age (years ± SD)/range | MAP target (mm Hg) |
|---|---|---|---|---|---|---|
| a)Number of patients include all the patients initially randomized in trial. H: high mean arterial pressure; S: standard mean arterial pressure; OHCA: out-of-hospital cardiac arrest; VT: ventricular tachycardia; VF: ventricular fibrillation; MAP: mean arterial pressure; SD: standard deviation; CABG: coronary artery bypass grafting. | ||||||
| Afsar et al, 2014 (SEPSISPAM) [13] | H: 388 | 3 | Septic shock refractory to fluid resuscitation, vasopressor use < 6 h | Pregnancy, decision not to resuscitate | H: 65 ± 13 | H: 80 - 85 |
| S: 388 | S: 65 ± 15 | S: 65 - 70 | ||||
| Lamontagne et al, 2016 (OVATION) [14] | H: 58 | 1 | Vasodilatory shock, adequate fluid resuscitation, vasopressor use ≥ 6 h | Vasopressors ≥ 24 h, expected to die within 48 h, other shock etiology | H: 63 ± 13 | H: 75 - 80 |
| S: 60 | S: 66 ± 13 | S: 60 - 65 | ||||
| Lamontagne et al, 2020 (65 Trial) [15] | H: 1,300 | 3 | Vasodilatory shock, adequate fluid resuscitation, vasopressor use ≥ 6 h | Vasopressors use for bleeding, cardiac failure, post-CABGs vasoplegia, brain or spinal cord injury | H: 74.8 (70.1 - 80.8) | H: > 70 |
| S: 1,283 | S: 75.2 (70.4 - 80.5) | S: 60 - 70 | ||||
| Jakkula et al, 2018 (COMACARE) [17] | H: 60 | 6 | Resuscitation after VT or VF OHCA | Intracranial pathology, severe respiratory failure | H: 58 ± 14 | H: 80 - 100 |
| S: 60 | S: 61 ± 11 | S: 65 - 75 | ||||
| Ameloot et al, 2019 (Neuroprotect) [16] | H: 52 | 6 | Resuscitated OHCA from presumed cardiac cause | Intracranial pathology, refractory shock on vasopressors | H: 64 ± 12 | H: 85 - 100 |
| S: 55 | S: 65 ± 13 | S: 65 | ||||
| Grand et al, 2020 [18] | H: 23 | 6 | Resuscitated OHCA from presumed cardiac cause | Unwitnessed OHCA asystole primary rhythm, intracranial pathology | H: 63 ± 10 | H: 72 |
| S: 26 | S: 59 ± 13 | S: 65 | ||||