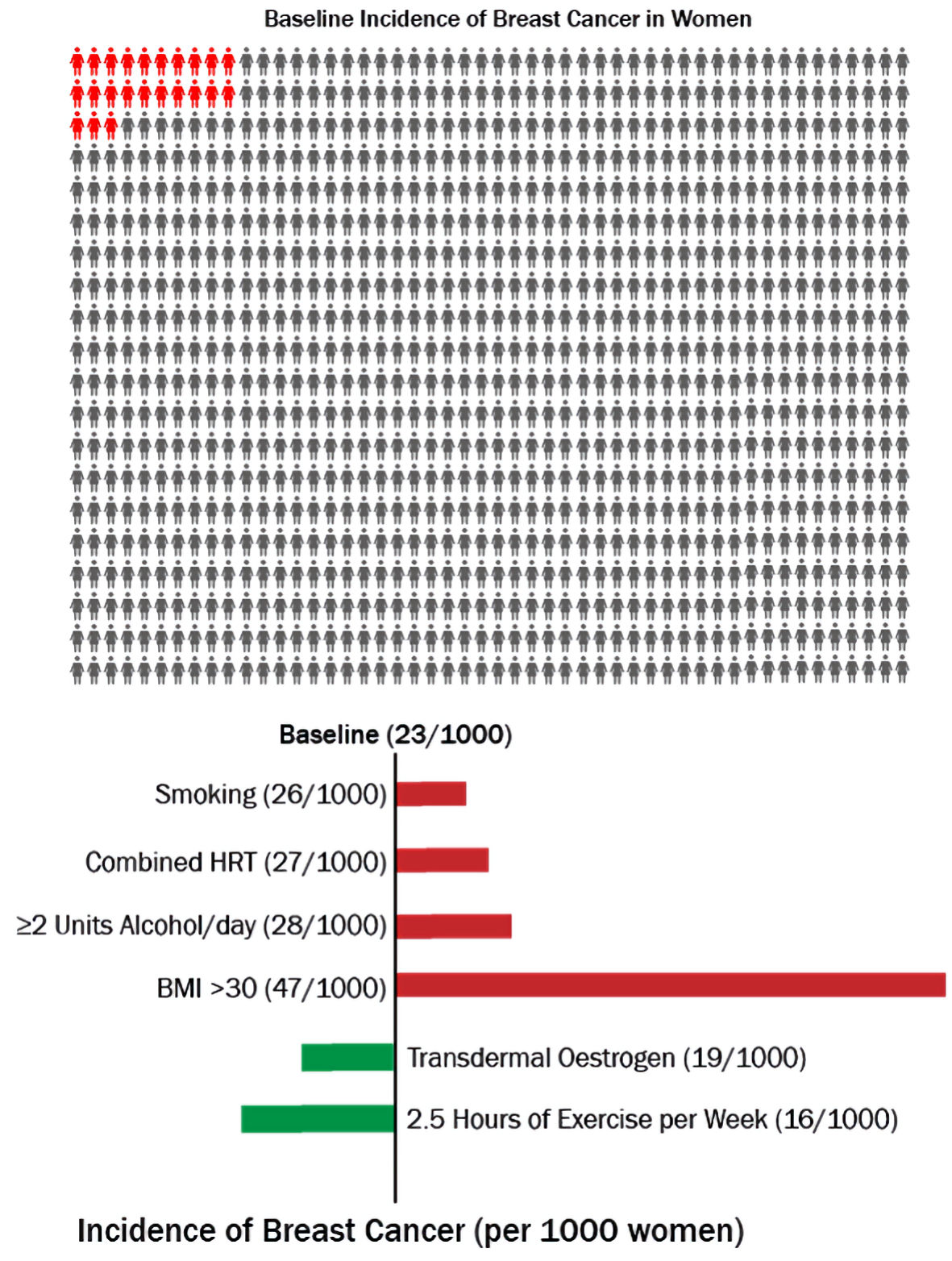
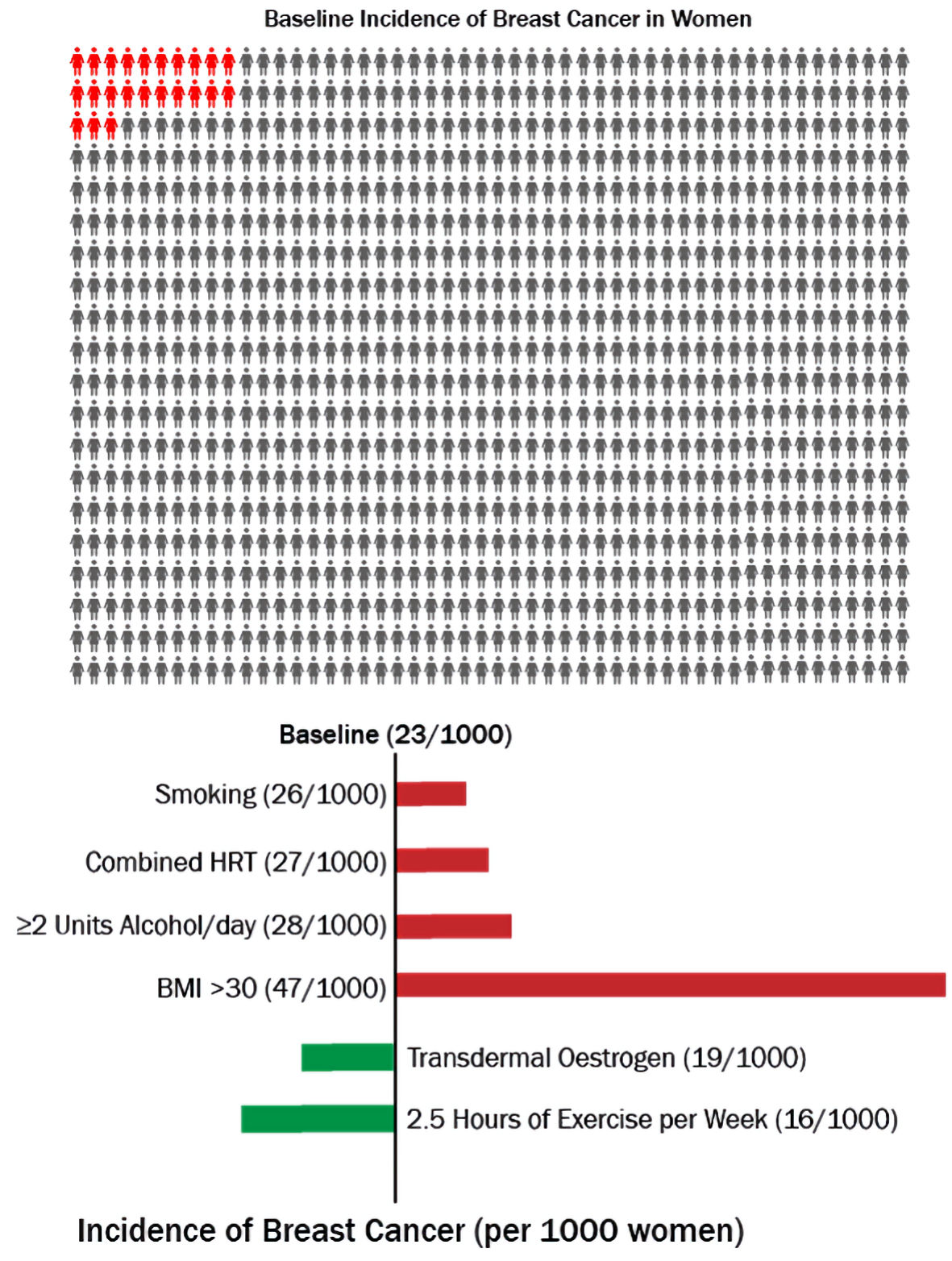
Figure 1. Risk of breast cancer associated with different modifiable risk factors over 5 years in women aged 50 - 59. HRT: hormone replacement therapy; BMI: body mass index.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Review
Volume 14, Number 1, January 2022, pages 1-7
Could Perimenopausal Estrogen Prevent Breast Cancer? Exploring the Differential Effects of Estrogen-Only Versus Combined Hormone Replacement Therapy
Figure
Table
| Study and year | Findings |
|---|---|
| HR: hazard ratio; CI: confidence interval; PE: pulmonary embolism; CHD: coronary heart disease; SD: standard deviation; CEE: conjugated equine estrogen; HR: hazard ratio; RR: risk ratio; MPA: medroxyprogesterone acetate. | |
| Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Beral et al, Collaborative Group on Hormonal Factors in Breast Cancer, 1997 [6] | Among current users of HRT or those who ceased use 1 - 4 years previously, the relative risk of having breast cancer diagnosed increased by a factor of 1.023 (95% CI: 1.011 - 1.036; 2P = 0.0002) for each year of use; the relative risk was 1.35 (1.21 - 1.49; 2P = 0.00001) for women who had used HRT for 5 years or longer (average duration of use in this group 11 years). Cancers diagnosed in women who had ever used HRT tended to be less advanced clinically than those diagnosed in never-users. |
| Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. Rossouw et al, Writing Group for the Women's Health Initiative Investigators, 2002 [9] | After a mean of 5.2 years of follow-up on HRT, results were: estimated HRs (nominal 95% CIs) were as follows: heart disease, 1.29 (1.02 - 1.63) with 286 cases; breast cancer, 1.26 (1.00 - 1.59) with 290 cases; stroke, 1.41 (1.07 - 1.85) with 212 cases; PE, 2.13 (1.39 - 3.25) with 101 cases; colorectal cancer, 0.63 (0.43 - 0.92) with 112 cases; endometrial cancer, 0.83 (0.47 - 1.47) with 47 cases; hip fracture, 0.66 (0.45 - 0.98) with 106 cases; and death due to other causes, 0.92 (0.74 - 1.14) with 331 cases. Absolute excess risks per 10,000 person-years attributable to estrogen plus progestin were seven more CHD events, eight more strokes, eight more PEs, and eight more invasive breast cancers, while absolute risk reductions per 10,000 person-years were six fewer colorectal cancers and five fewer hip fractures. The absolute excess risk of events included in the global index was 19 per 10,000 person-years. |
| Breast cancer and hormone-replacement therapy in the Million Women Study. Million Women Study Collaborators, 2003 [7] | Half the women in study had used HRT; and 9,364 incident invasive breast cancers and 637 breast cancer deaths were registered after an average of 2.6 and 4.1 years of follow-up, respectively. Current users of HRT at recruitment were more likely than never users to develop breast cancer (adjusted relative risk 1.66 (95% CI: 1.58 - 1.75), P < 0.0001) and die from it (1.22 (1.00 - 1.48), P = 0.05). Incidence was significantly increased for current users of preparations containing estrogen only (1.30 (1.21 - 1.40), P < 0.0001), estrogen-progestogen (2.00 (1.88 - 2.12), P < 0.0001), and tibolone (1.45 (1.25 - 1.68), P < 0.0001), but the magnitude of the associated risk was substantially greater for estrogen-progestogen than for other types of HRT (P < 0.0001). |
| Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Collaborative Group on Hormonal Factors in Breast Cancer, 2019 [8] | During prospective follow-up, 108,647 postmenopausal women developed breast cancer at mean age 65 years (SD: 7); 55,575 (51%) had used HRT. Among women with complete information, mean hormone therapy duration was 10 years (SD: 6) in current users and 7 years (SD: 6) in past users, and mean age was 50 years (SD: 5) at menopause and 50 years (SD: 6) at starting HRT. Every HRT type, except vaginal estrogens, was associated with excess breast cancer risks, which increased steadily with duration of use and were greater for estrogen-progestogen than estrogen-only preparations. Among current users, these excess risks were definite even during years 1 - 4 (estrogen-progestogen RR: 1.60, 95% CI: 1.52 - 1.69; estrogen-only RR: 1.17, 1.10 - 1.26), and were twice as great during years 5 - 14 (estrogen-progestogen RR: 2.08, 2.02 - 2.15; estrogen-only RR: 1.33, 1.28 - 1.37). |
| Association of menopausal hormone therapy with breast cancer incidence and mortality during long-term follow-up of the Women’s Health Initiative randomized clinical trials. Chlebowski et al, 2020 [10] | Among 27,347 postmenopausal women who were randomized (baseline mean (SD) age, 63.4 years (7.2 years)), after more than 20 years of median cumulative follow-up, mortality information was available for more than 98%. Estrogen (CEE) 0.625 mg daily alone compared with placebo among 10,739 women with a prior hysterectomy was associated with statistically significantly lower breast cancer incidence with 238 cases (annualized rate: 0.30%) vs. 296 cases (annualized rate: 0.37%; HR: 0.78; 95% CI: 0.65 - 0.93; P = 0.005) and was associated with statistically significantly lower breast cancer mortality with 30 deaths (annualized mortality rate: 0.031%) vs. 46 deaths (annualized mortality rate: 0.046%; HR: 0.60; 95% CI: 0.37 - 0.97; P = 0.04). In contrast, CEE 0.625 mg daily plus progestogen (MPA) 2.5 mg daily compared with placebo among 16,608 women with a uterus was associated with statistically significantly higher breast cancer incidence with 584 cases (annualized rate: 0.45%) vs. 447 cases (annualized rate: 0.36%; HR: 1.28; 95% CI: 1.13 - 1.45; P < 0.001) and no significant difference in breast cancer mortality. |