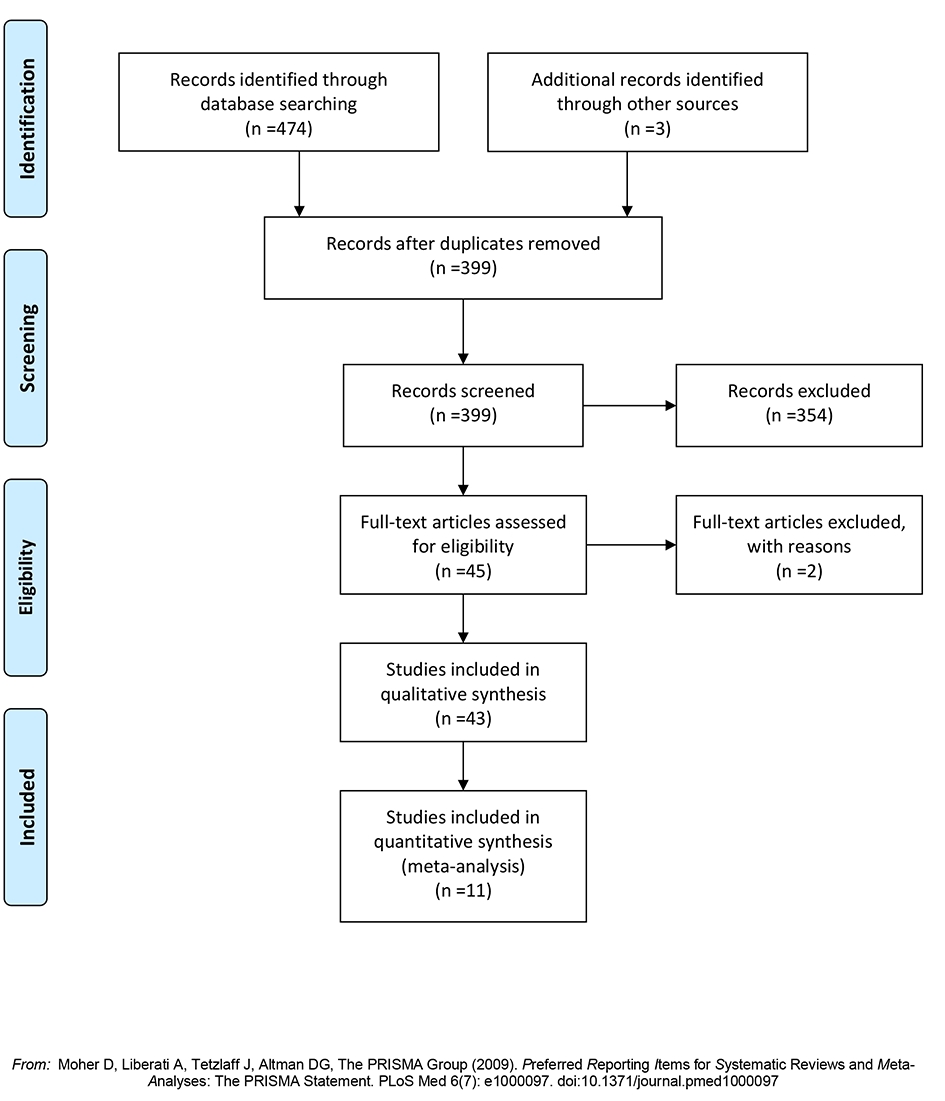
Figure 1. Flow diagram of the search strategy.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 11, Number 8, August 2019, pages 600-608
Gastrectomy Alone or in Combination With Hepatic Resection in the Management of Liver Metastases From Gastric Cancer: A Systematic Review Using an Updated and Cumulative Meta-Analysis
Figures
Table
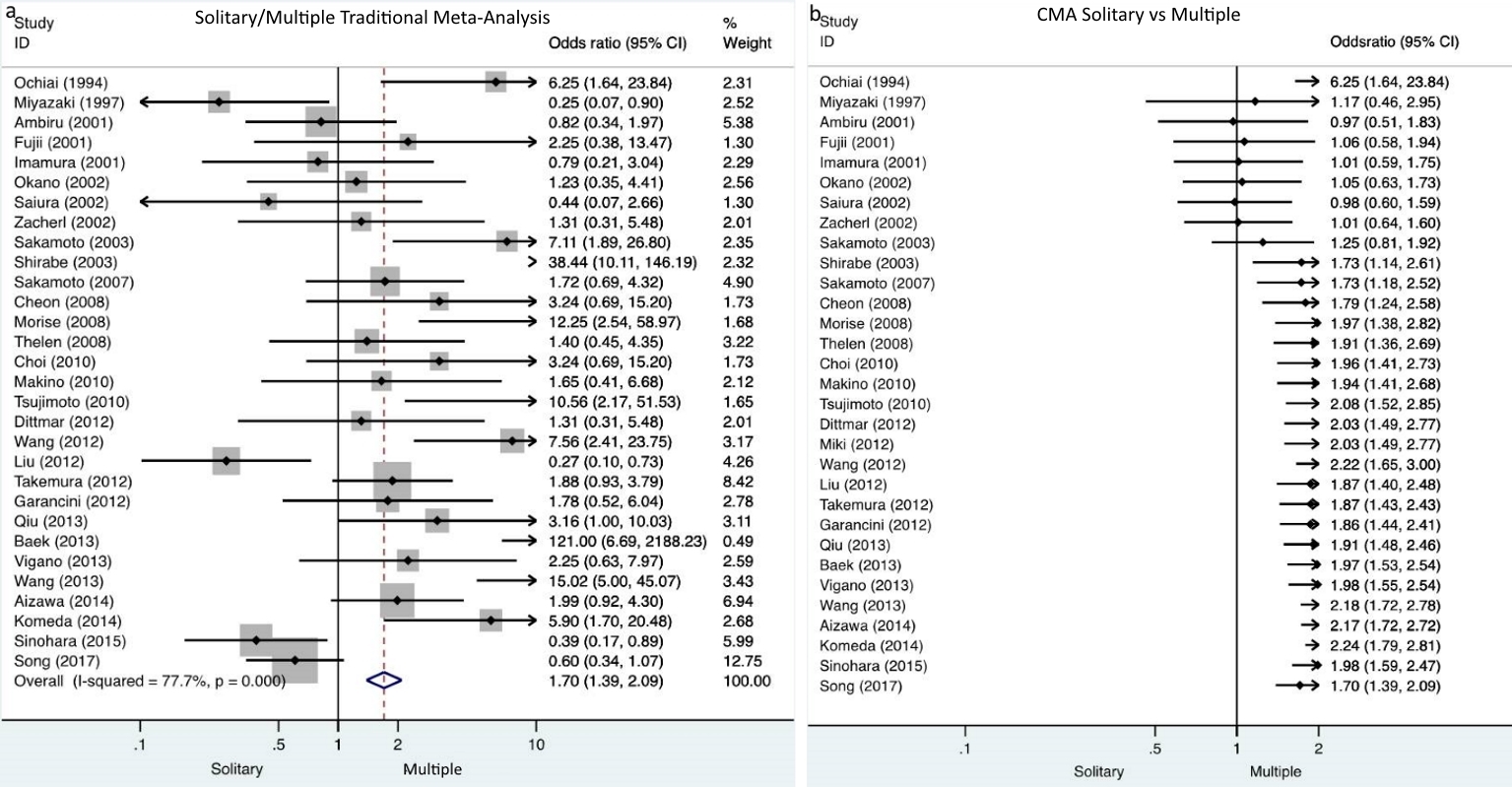
| Outcome of interest | Number of studies and patients (%; events/total) | Statistical method, estimated effect, 95% CI | P value | I2 (%) |
|---|---|---|---|---|
| OS: overall survival; MD: mean difference; HR: hazard ratio; OR: odds ratios. | ||||
| Age | 4, 244 | MD = -2.40 (-6.13 to 1.34) | 0.23 | 57 |
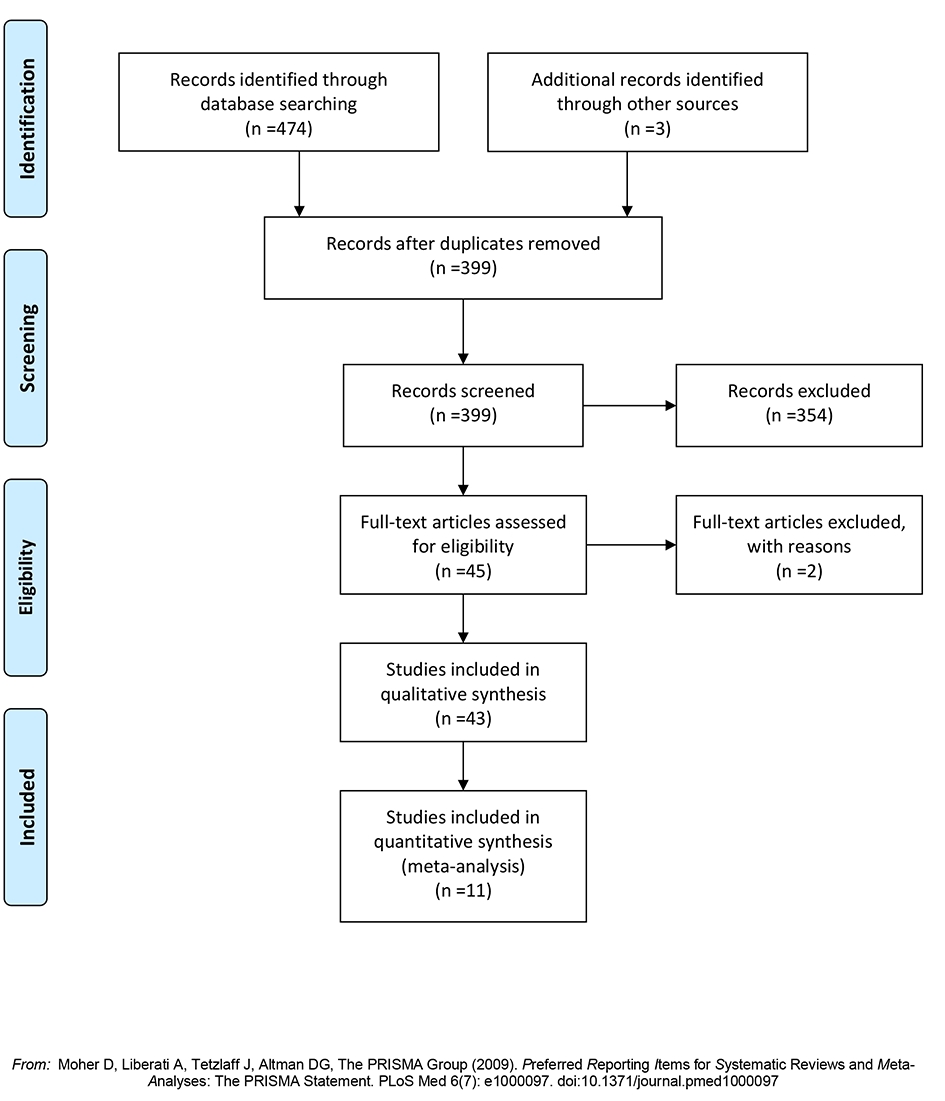
| Synchronous metastases | 4, 206 (54%; 56/104) (51%; 52/102) | OR = 0.42 (0.02 to 8.50) | 0.57 | 89 |
| Metachronous metastases | 4, 206 (28%; 29/104) (29%; 30/102) | OR = 1.72 (0.86 to 3.43) | 0.12 | 85 |
| Unilobar metastases | 6, 430 (58%; 92/159) (25%; 67/271) | OR = 3.88 (2.43 to 6.19) | < 0.001 | 0 |
| Bilobar metastases | 6, 430 (26%; 41/159) (49%; 133/271) | OR = 0.27 (0.08 to 0.91) | 0.04 | 83 |
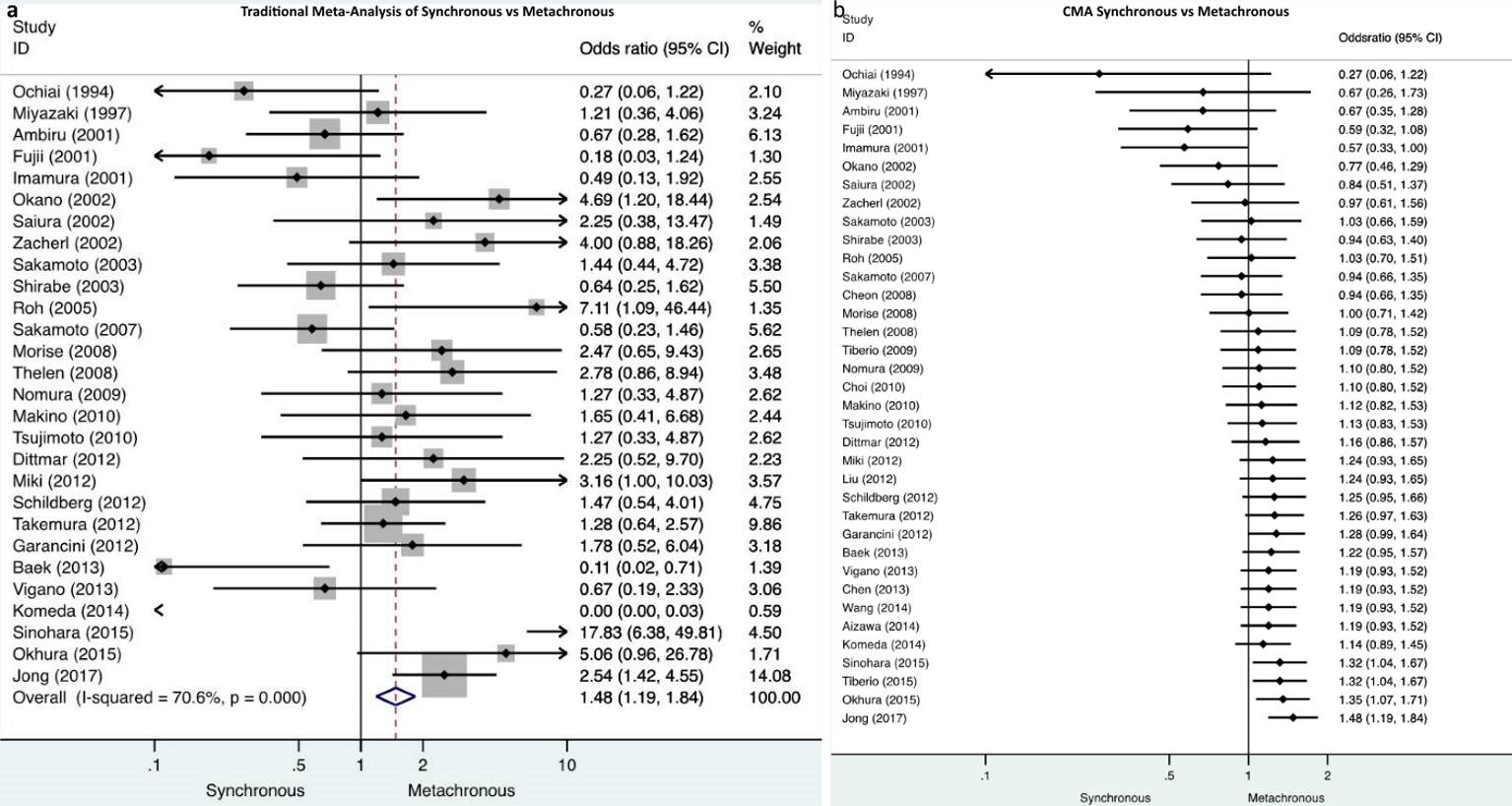
| Solitary metastases | 5, 320 (52%; 64/124) (36%; 71/196) | OR = 2.98 (0.95 to 9.37) | 0.06 | 70 |
| Multiple metastases | 5, 320 (33%; 41/124) (66%; 129/196) | OR = 0.17 (0.04 to 0.80) | 0.02 | 83 |
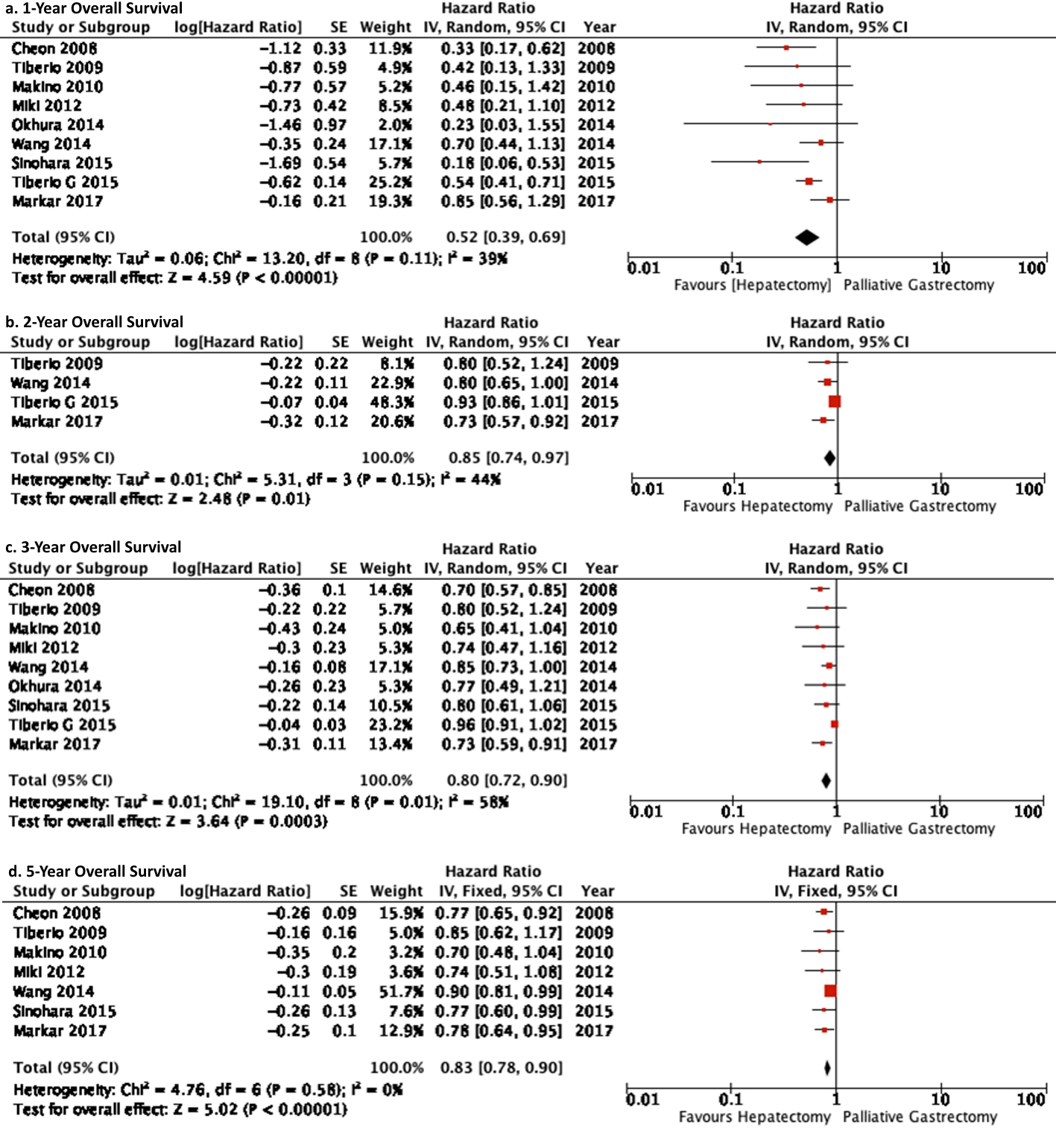
| 1-year OS | 9, 637 | HR = 0.52 (0.39 to 0.69) | < 0.001 | 39 |
| 2-year OS | 4, 397 | HR = 0.85 (0.74 to 0.97) | 0.01 | 44 |
| 3-year OS | 9, 637 | HR = 0.80 (0.72 to 0.90) | 0.003 | 58 |
| 5-year OS | 7, 452 | HR = 0.83 (0.78 to 0.90) | < 0.001 | 0 |
| Subgroup analysis East versus West | ||||
| 1-year OS East | 6, 306 | HR = 0.42 (0.28 to 0.65) | < 0.001 | 34 |
| 1-year OS West | 3, 331 | HR = 0.63 (0.43 to 0.91) | 0.01 | 47 |
| 2-year OS West | 3, 331 | HR = 0.85 (0.71 to 1.01) | 0.07 | 53 |
| 2-year OS East | 1, 66 | HR = 0.80 (0.65 to 1.00) | 0.05 | 0 |
| 3-year OS East | 6, 306 | HR = 0.78 (0.70 to 0.86) | < 0.001 | 0 |
| 3-year OS West | 3, 331 | HR = 0.85 (0.69 to 1.05) | 0.13 | 67 |
| 5-year OS East | 5, 272 | HR = 0.84 (0.78 to 0.91) | < 0.001 | 5 |
| 5-year OS West | 2, 180 | HR = 0.80 (0.68 to 0.94) | 0.008 | 0 |