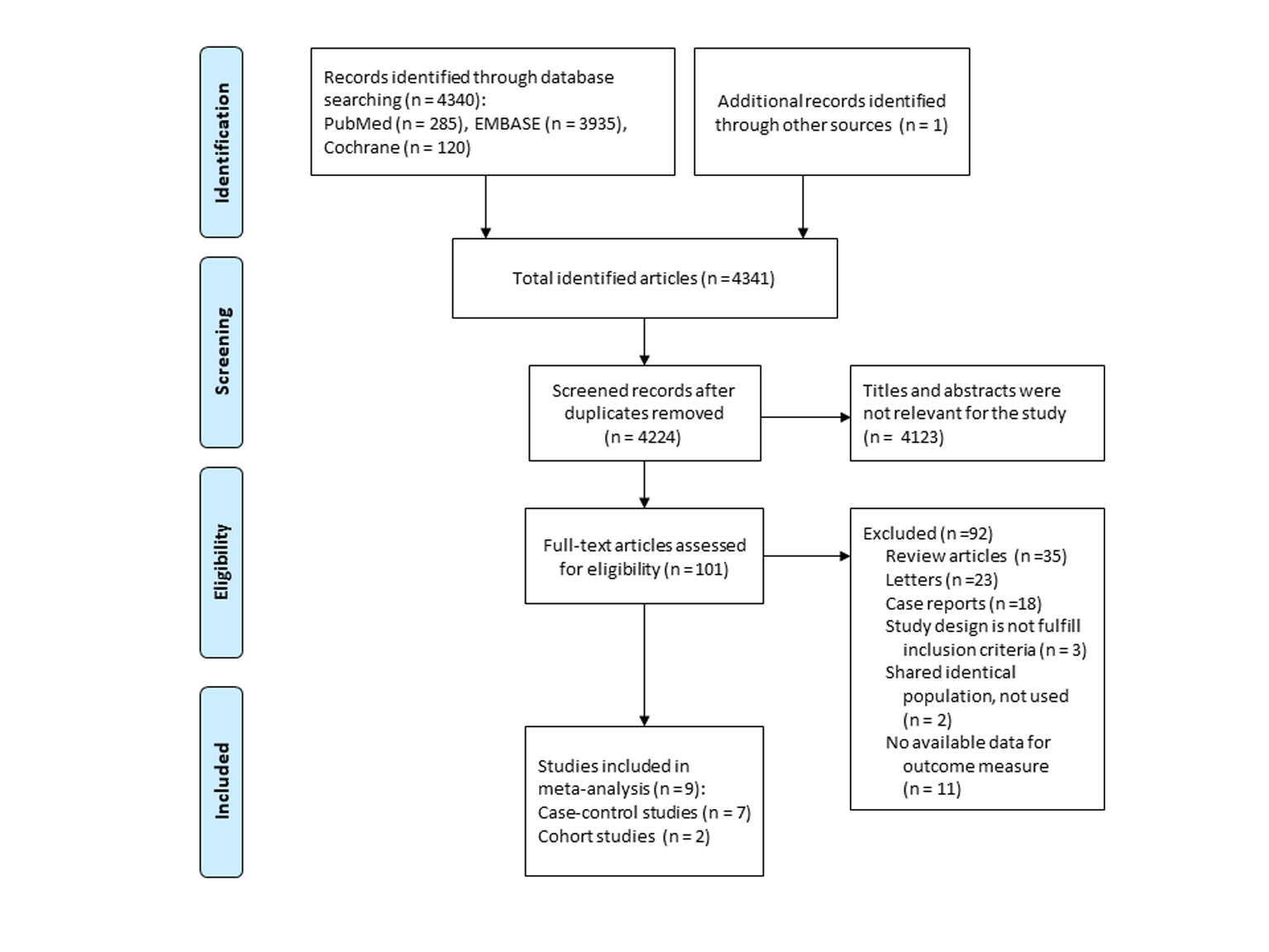
Figure 1. Flow diagram of studies identified and selected.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 11, Number 4, April 2019, pages 247-255
Association Between the Use of Thiazide Diuretics and the Risk of Skin Cancers: A Meta-Analysis of Observational Studies
Figures
Tables
| Study | Country | Study design | Medication | Outcome | Study population (case group or cohort) | Exposed/ unexposed | RR or OR (95% CI) | Adjusted RR or OR (95% CI) | Study period (year) | Adjustment |
|---|---|---|---|---|---|---|---|---|---|---|
| BCC: basal cell carcinoma; SCC: squamous cell carcinoma; MM: malignant melanoma; HCTZ: hydrochlorothiazide; RR: risk ratio; OR: odds ratio; CI: confidence interval; NA: not available; USA: United States of America. | ||||||||||
| Pottegard 2017 | Denmark | Case-control | HCTZ | SCC | Mean age 72, men 67.3% | Cases: 139/494, controls:7,401/55,666 | 2.2 (1.8 - 2.6) | 2.1 (1.7 - 2.6) | 2004 - 2012 | Adjusted for age, gender, calendar time, use of topical retinoids, oral retinoids, tetracycline, macrolides, aminoquinolines, amiodarone, aspirin, non-aspirin non-steroidal anti-inflammatory drugs, statins, history of heavy alcohol consumption, diabetes, or chronic obstructive pulmonary disease, non-melanoma skin cancer, Charlson Comorbidity Index score, and highest achieved education |
| Nardone 2017 | USA | Cohort | Thiazides | BCC | Age 18 - 89, men 37.5%, white 34% | Cases: 262/457, controls: 15,166/45,498 | 1.73 (1.49 - 2.02) | 2.11 (1.60 - 2.79) | 2004 - 2014 | Matched for age and time to follow-up, and adjusted for age, gender, race, and the Charlson Comorbidities Index |
| SCC | Cases: 130/132, controls: 15,166/45,498 | 2.97 (2.33 - 3.79) | 4.11 (2.66 - 6.35) | |||||||
| MM | Cases: 99/145, controls:15,166/45,498 | 2.06 (1.59 - 2.66) | 1.82 (1.01 - 3.82) | |||||||
| Schmidt 2015 | Denmark | Case-control | Thiazides | BCC | Median age 67, men 50% | Cases: 2,710/10,473, controls: 26,504/107,016 | NA | 1.05 (1.00 - 1.11) | 1991 - 2010 | Matched for birth year, sex and county of residence, and adjusted for Charlson Comorbidity Index score, hospital-diagnosed obesity and use of systemic glucocorticoids, aspirin, non-aspirin non-steroidal, anti-inflammatory drugs and statins |
| SCC | Median age 77, men 63% | Cases: 447/1,135, controls: 4,458/12,007 | NA | 1.03 (0.91 - 1.17) | ||||||
| MM | Median age 58, men 46% | Cases: 403/2,648, controls: 3,786/26,686 | NA | 1.11 (0.97 - 1.25) | ||||||
| Robinson 2013 | USA | Case-control | HCTZ or combination | SCC | Age 25 - 74, men 61.7% | Cases: 1,599 in total, controls: 1,906 in total | NA | 1.3 (0.7 - 2.4) | 1993 - 2009 | Matched for age and sex, and adjusted for age, sex, and number of previous painful sunburns |
| de Vries 2012 | Europe (multi-center) | Case-control | Thiazides | BCC | Median age 72, men 59.6% | Case: 94/508, control: 136/1,414 | 1.92 (NA) | 1.27 (0.92 - 1.75) | NA | Matched for age and sex, and adjusted for age, sex, skin photo-type and country |
| SCC | Median age 76, men 70.2% | Case: 99/310, control: 136/1,414 | 3.32 (NA) | 1.66 (1.16 - 2.37) | ||||||
| MM | Median age 62, men 54.4% | Cases: 33/327, control: 136/1,414 | 1.05 (NA) | 1.22 (0.77 - 1.93) | ||||||
| Friedman 2012 | USA | Case-control | HCTZ or combination | SCC | Mean age 68, men 74.4%, non-Hispanic white 100% | Cases: 103/609, controls: 1,896/21,008 | 2.22 (1.76 - 2.79) | 2.19 (1.74 - 2.76) | 1994 - 2008 | Matched for age, sex, and year of entry into the cohort, and adjusted for smoking |
| Ruiter 2010 | Netherlands | Cohort | Thiazides | BCC | Mean age 69, men 40% | 137/385 | NA | 1.00 (0.95 - 1.05) | 1991 - 2007 | Adjusted for age and gender, and none of the potential covariates was a confounder |
| Jensen 2008 | Denmark | Case-control | HCTZ | BCC | Mean age 69 | Cases: 542/5,422, controls: 2,059/21,797 | NA | 1.05 (0.95 - 1.16) | 1989 - 2003 | Matched for age and sex, and adjusted for prior hospitalization for selected chronic diseases and use of glucocorticoids |
| SCC | Mean age 77 | Cases: 159/910, controls: 427/4,089 | NA | 1.58 (1.29 - 1.93) | ||||||
| MM | Mean age 59 | Cases: 98/912, controls: 303/3,737 | NA | 1.32 (1.03 - 1.70) | ||||||
| Westerdahl 1996 | Sweden | Case-control | Thiazide | MM | Age 15 - 75, men 46.6% | Cases: 20/328, controls: 25/535 | 1.4 (0.7 - 2.7) | 1.4 (0.7 - 2.8) | 1988 - 1990 | Matched for sex, age, parish, and adjusted for history of sunburns and host factors (hair color, number of raised naevi) |
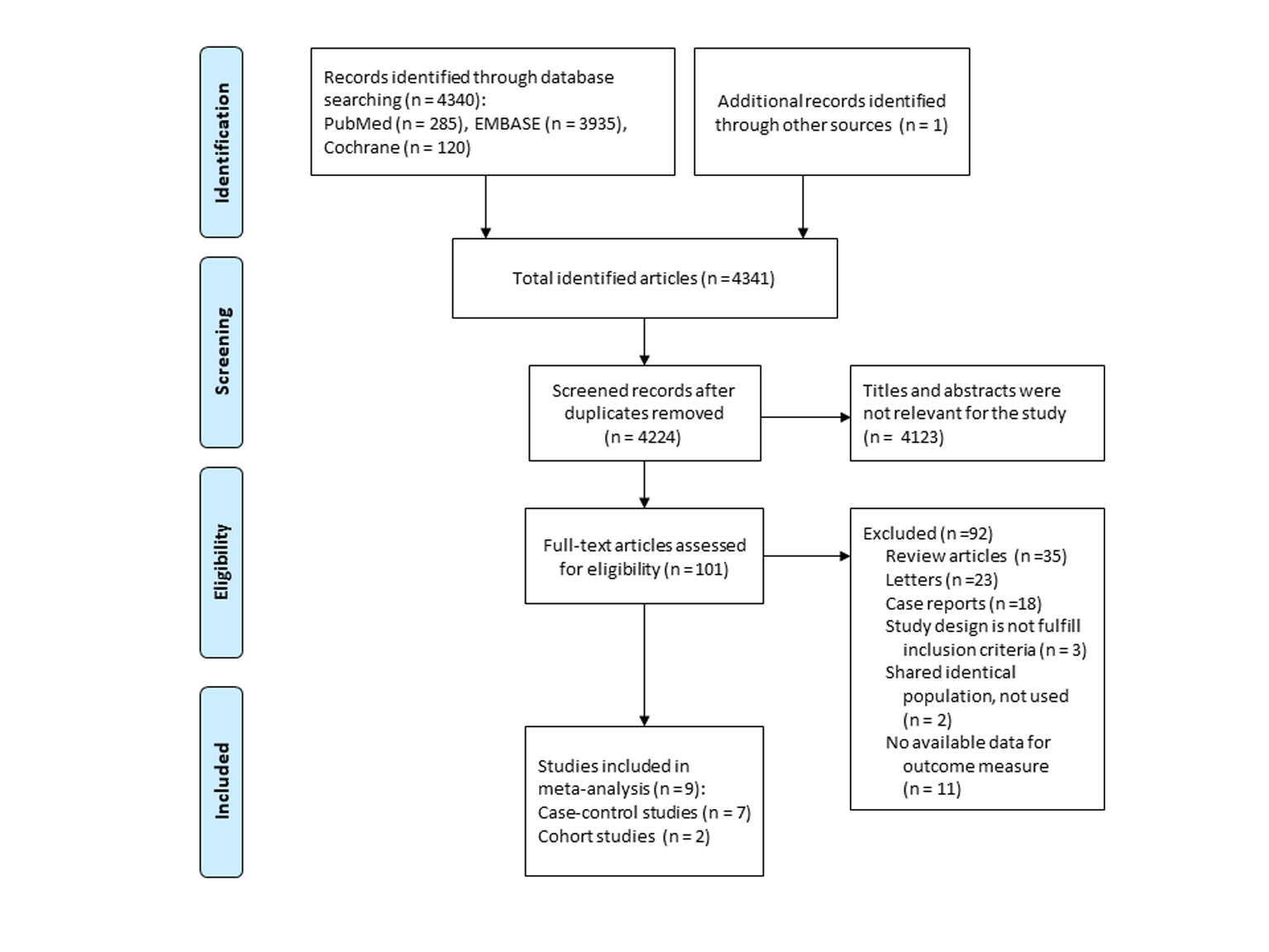
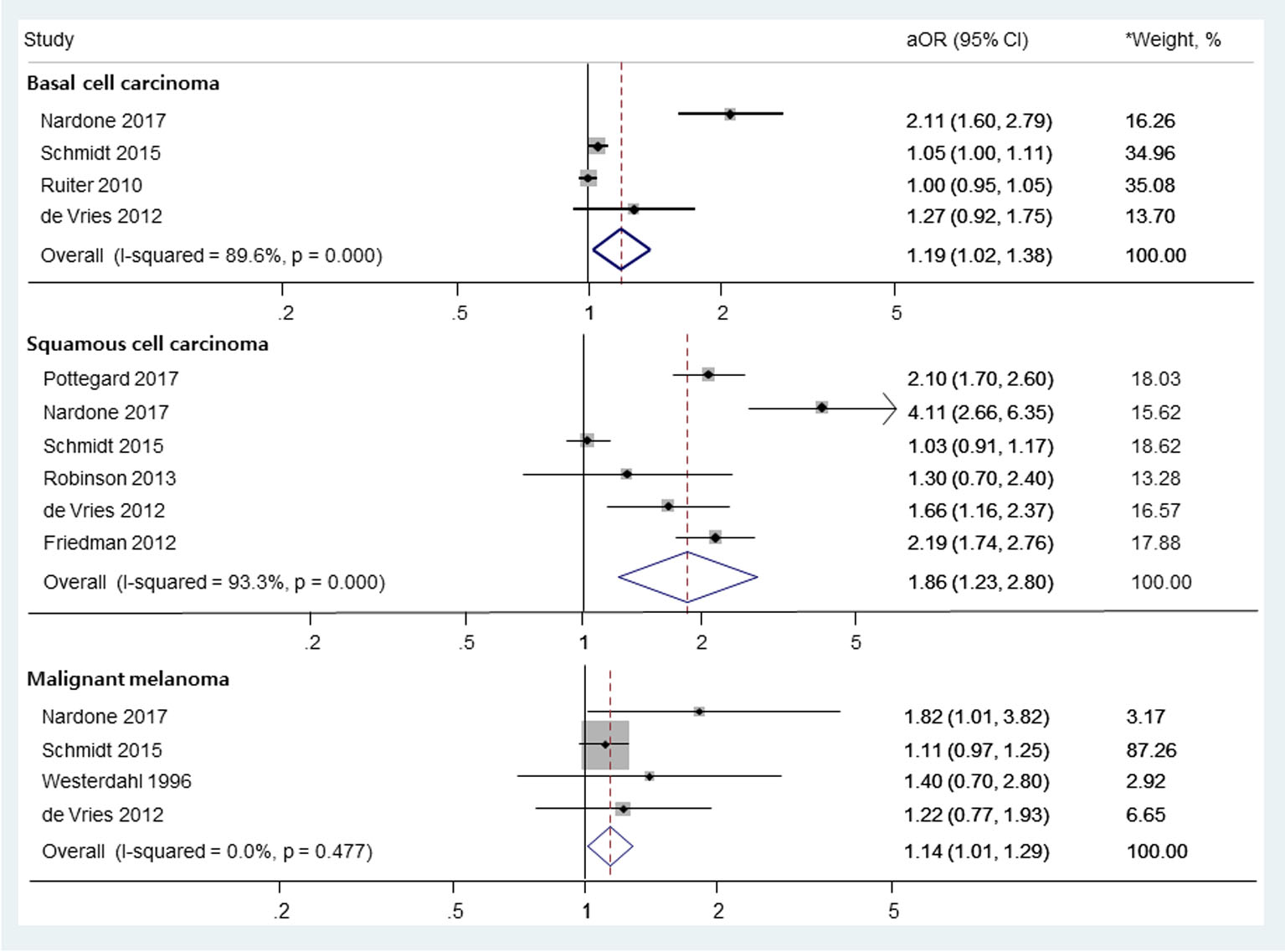
| No. of studies | OR (95% CI) | I2 (%) | Q-statistics | P value | |
|---|---|---|---|---|---|
| I2: Higgins score; NA: not available. *More than 4.5 years. | |||||
| Basal cell carcinoma | |||||
| Duration of use, long-term use* | 2 | 1.10 (0.96 - 1.25) | 0.0 | 0.0 | 1.000 |
| Study design | |||||
| Case-control | 2 | 1.08 (0.95 - 1.23) | 89.6 | 1.3 | 0.252 |
| Cohort | 2 | 1.43 (0.69 - 2.98) | 96.3 | 26.8 | < 0.001 |
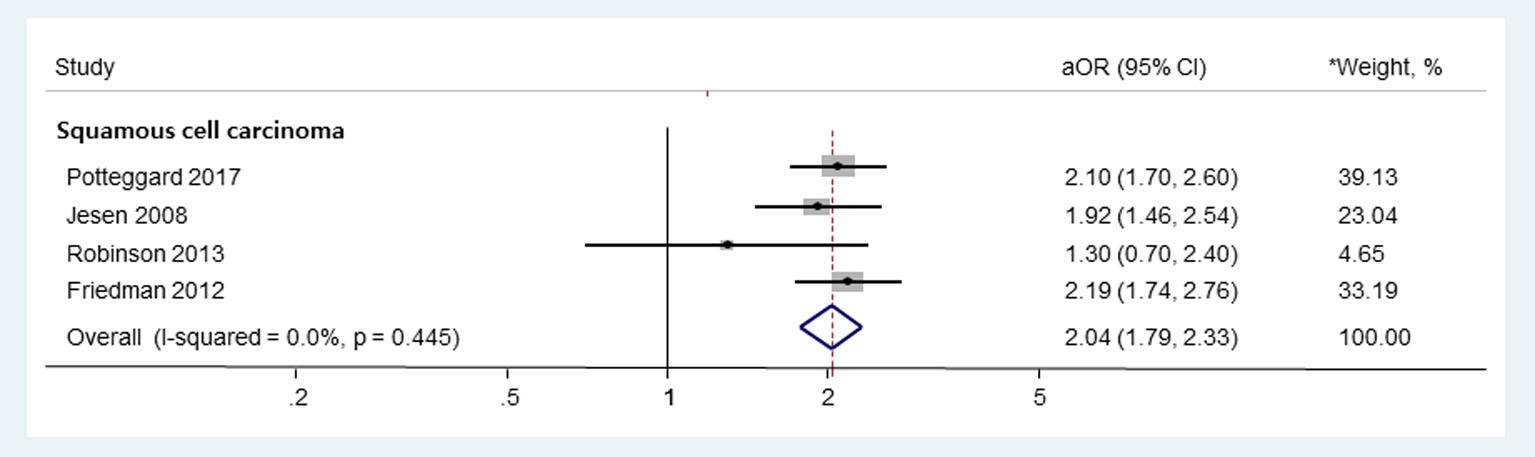
| Squamous cell carcinoma | |||||
| Duration of use, long-term use* | 3 | 3.30 (1.85 - 5.89) | 90.7 | 21.4 | < 0.001 |
| Study design | |||||
| Case-control | 5 | 1.61 (1.08 - 2.38) | 92.3 | 52.3 | < 0.001 |
| Cohort | 1 | NA | NA | NA | NA |
| Malignant melanoma | |||||
| Duration of use, long-term use* | 1 | NA | NA | NA | NA |
| Study design | |||||
| Case-control | 3 | 1.13 (1.00 - 1.27) | 0.0 | 0.6 | 0.761 |
| Cohort | 1 | NA | NA | NA | NA |