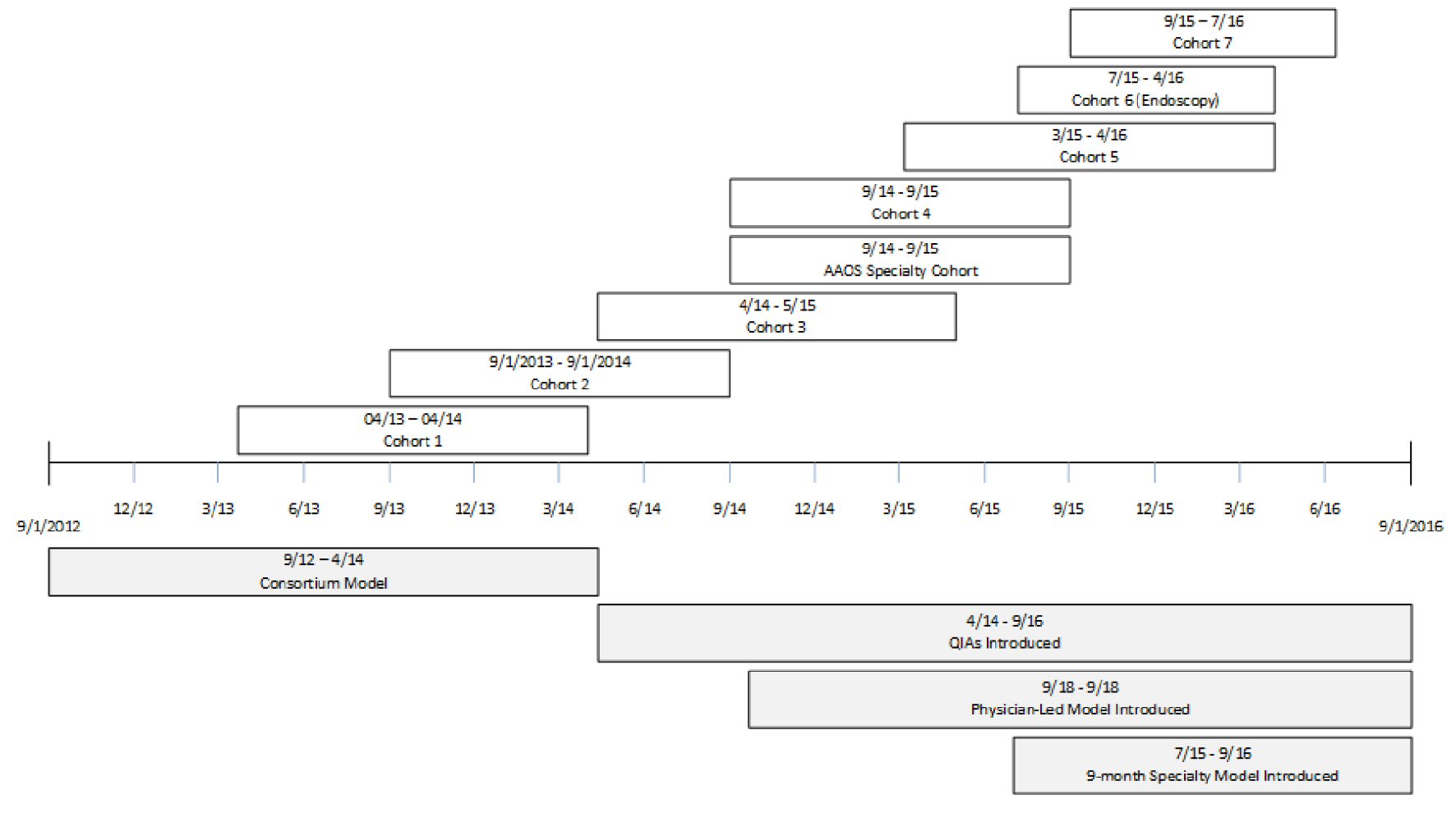
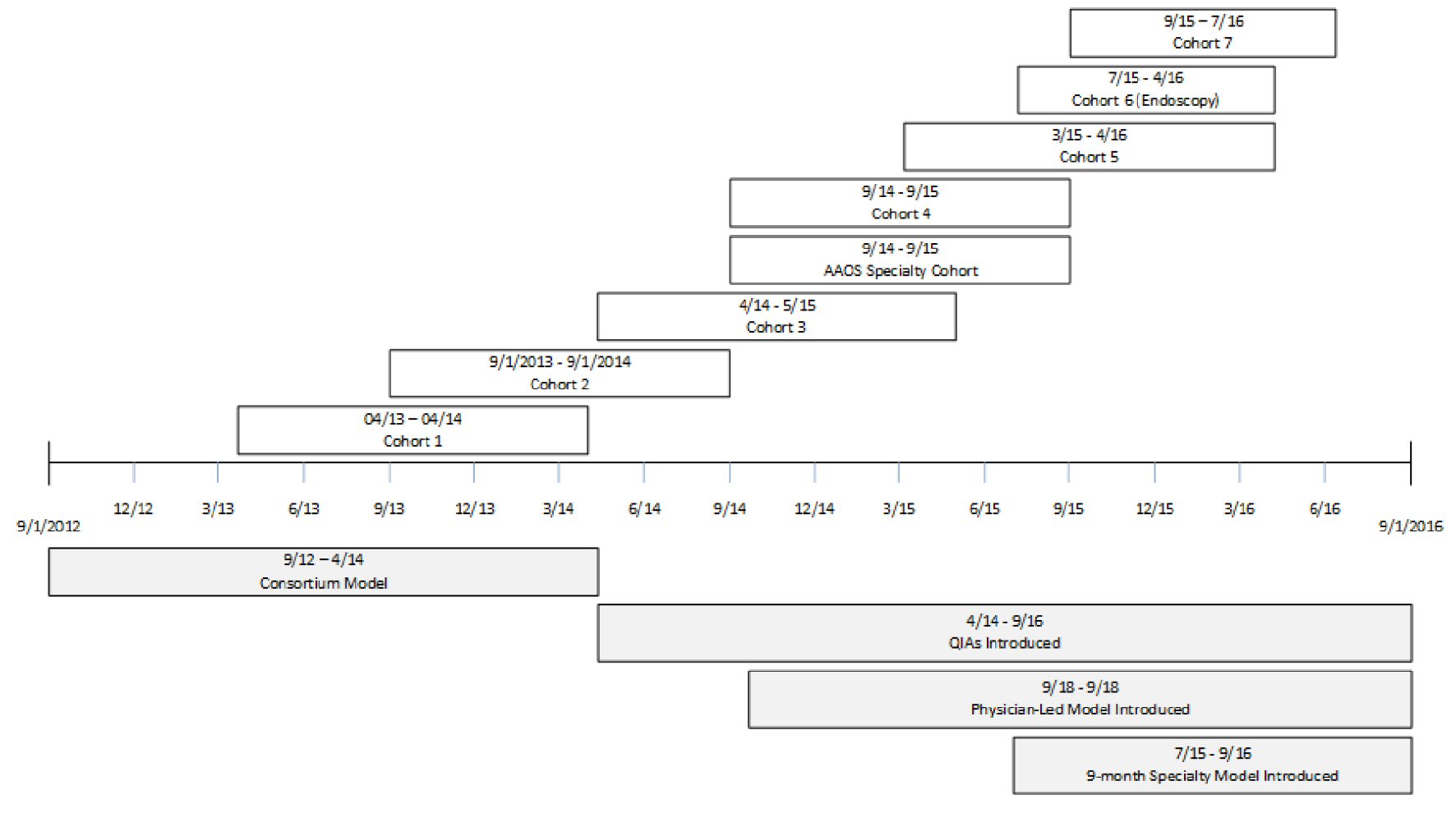
Figure 1. Timeline of events.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 11, Number 1, January 2019, pages 7-14
Quality Improvement in Ambulatory Surgery Centers: A Major National Effort Aimed at Reducing Infections and Other Surgical Complications
Figure
Tables
| Partner |
|---|
| Harvard School of Public Health (HSPH) |
| Ambulatory Surgery Center Association (ASCA) |
| ASC Quality Collaboration (ASC QC) |
| Westat |
| South Carolina Hospital Association (SCHA) |
| Institute for Healthcare Improvement (IHI) |
| Extended faculty network |
| American Academy of Orthopaedic Surgeons (AAOS) |
| American Association of Nurse Anesthetists (AANA) |
| Society for Ambulatory Anesthesiology (SAMBA) |
| Association of periOperative Registered Nurses (AORN) |
| Association for Professionals in Infection Control and Epidemiology, Inc. (APIC) |
| International Association of Healthcare Central Service Material Management (IAHCSMM) |
| Accreditation Association for Ambulatory Health Care (AAAHC) |
| The Joint Commission (TJC) |
| American Society for Gastrointestinal Endoscopy (ASGE) |
| Association for the Advancement of Medical Instruments (AAMI) |
| Representatives from state ambulatory surgery associations and ASC management companies |
| Cohort | # of facilities | Participation dates |
|---|---|---|
| AAOS: American Academy of Orthopaedic Surgeons. | ||
| Cohort 1 | 53 | April, 2013 - April, 2014 |
| Cohort 2 | 109 | September, 2013 - September, 2014 |
| Cohort 3 | 69 | April, 2014 - May, 2015 |
| AAOS specialty Cohort | 12 | September, 2014 - September, 2015 |
| Cohort 4 | 100 | September, 2014 - October, 2015 |
| Cohort 5 | 103 | March, 2015 - April, 2016 |
| Cohort 6 (endoscopy-only) | 119 | July, 2015 - April, 2016 |
| Cohort 7 | 82 | September, 2015 - July, 2016 |
| Components/specifications | Frequency | Description |
|---|---|---|
| Facility demographics | Once, upon enrollment | Facility and staff member demographics |
| Project defined data elements | Surgeries and procedures - types and volume | |
| Current data collection, measurement and monitoring efforts | ||
| Current quality improvement, patient safety and surgical checklist practices | ||
| In-Center outcomes and process measures | Monthly | Wrong site, wrong side, wrong patient, wrong procedure, wrong implant |
| Ambulatory Surgery Center Quality Collaboration (ASC QC) | Hospital transfer / Admission from the ASC | |
| Centers for Medicare and Medicaid Services (CMS) Ambulatory Surgical Center Quality Reporting (ASCQR) Program | Patient burn | |
| Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN) | Patient fall | |
| Prophylactic IV antibiotic timing (if applicable) | ||
| Patient safety culture assessment | Beginning and end of project | Assesses staff perceptions of key patient safety elements such as: |
| Harvard tool designed for South Carolina Safe Surgery 2015 Project | 1. Readiness for improvement | |
| 2. Teamwork and communication in the OR | ||
| 3. Adherence to process measures | ||
| 4. Perceptions of effective use of a safe surgery checklist | ||
| Patient satisfaction | Beginning and end of project | Overall satisfaction with the center and/or likelihood to recommend the center |
| Facility defined |
| Event | Event description | # of occurrences |
|---|---|---|
| *Number of meetings between April 24, 2013 and September 29, 2016. NPT: national project team; EFN: extended faculty network; QIA: quality improvement advisors; QI: quality improvement. | ||
| Milestone meetings | Milestone meetings were held with each cohort as an opportunity to touch base at each stage of the program. These meetings were held both virtually and in person and included a kickoff in the beginning of the program, a midcourse meeting around 6 - 7 months into the program, and a final meeting upon program completion. With program redirection, midcourse meetings were held as needed. | 25 |
| Educational webinars | Educational webinars were 60 min of web-based training that was structured to include 45 min of content and 15 min of question and answer. Webinars were hosted by the NPT and covered topics in the areas of data collection and reporting, checklist and safety, and infection prevention. | 74 |
| Office hours | Office hours were monthly calls facilitated by a member of the NPT and were a platform for participating facilities to discuss their barriers and successes, leverage peer-to-peer experience, and learn how to improve program goals. Office hours educational topics were informed by participants, EFN, and partners through the Office Hours Evaluation Survey as well as feedback from monthly partner and EFN calls. QIAs actively participated in office hours by facilitating discussion, encouraging online peer-to-peer communication, and answering questions. | 35 |
| Learning groups | Learning groups were small group discussions facilitated by QIAs. Benefits of these interactions included creating a sense of community within the program, providing time to share success stories and challenges, and building lasting networking relationships for program participants. Discussion topics included physician engagement, how to conduct the debriefing at the end of a case, administering the culture survey, speaking up using structured language, and use of the QI framework. | 122 |
| Master trainer events | The master trainer events occurred annually throughout the project. These events focused on several train-the-trainer educational events on the topics of coaching, TeamSTEPPS teamwork and communication tools, and patient and family engagement within ambulatory settings. | 4 |
| Components/specification | Frequency | Description |
|---|---|---|
| ASC: ambulatory surgery center; ED: emergency department; SSI: surgical site infection; AAOS: the American Academy of Orthopaedic Surgeons | ||
| Unexpected events | As they occur, C3 and beyond | For each event listed below, facilities provide additional information including the procedure that took place in the ASC, date of the event, date of the procedure, reason for transfer/admission, and how the facility found out about the event: |
| 1. Wrong side, site, patient, procedure, implant | ||
| 2. Hospital transfer/admission from the ASC | ||
| 3. Hospitalization or ED visit within 48 h of discharge from ASC | ||
| 4. Reoperation within 48 h of discharge from ASC | ||
| 5. SSI | ||
| 6. Other infection (Non-SSI) | ||
| 7. Cancelled procedure | ||
| 8. Other unexpected event | ||
| In addition, cohort specific events include: | ||
| 1. Wrong side, site anesthesia block (AAOS cohort) | ||
| 2. Unplanned intervention- resolved in the ASC (endoscopy cohort) | ||
| Event description | Number of events reported | Percent of all events reported |
|---|---|---|
| The highest number of events was related to same day cancellations, hospital transfer/admission, and hospital/ED visit within 48 h, and “other”. The most common reasons for hospital transfer/admission from the ASC were unstable vital signs, airway management concerns, and cardiac issues. The most common reasons for “other” were unexpected preoperative findings such as high blood pressure, fever, high glucose and patients unprepared for procedure. | ||
| Same day cancelled procedure (Cohort 6 only) | 2,602 | 54% |
| Other | 748 | 16% |
| Hospital transfer/admission from the ASC | 552 | 12% |
| Hospital admission/ED visit within 48 h of discharge from the ASC | 479 | 10% |
| Surgical site infection | 143 | 3% |
| Unplanned intervention resolved in the ASC | 92 | 2% |
| Cancelled surgery due to medical reason (Cohort 7 only) | 104 | 2% |
| Reoperation within 48 h of discharge from the ASC | 57 | 1% |
| Other infection (Non-SSI) | 17 | 0% |