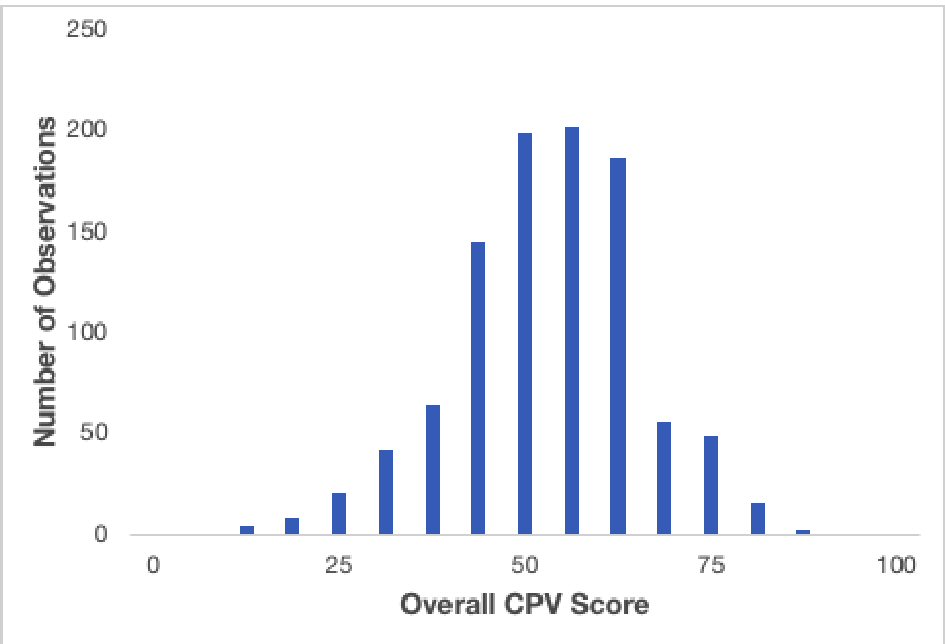
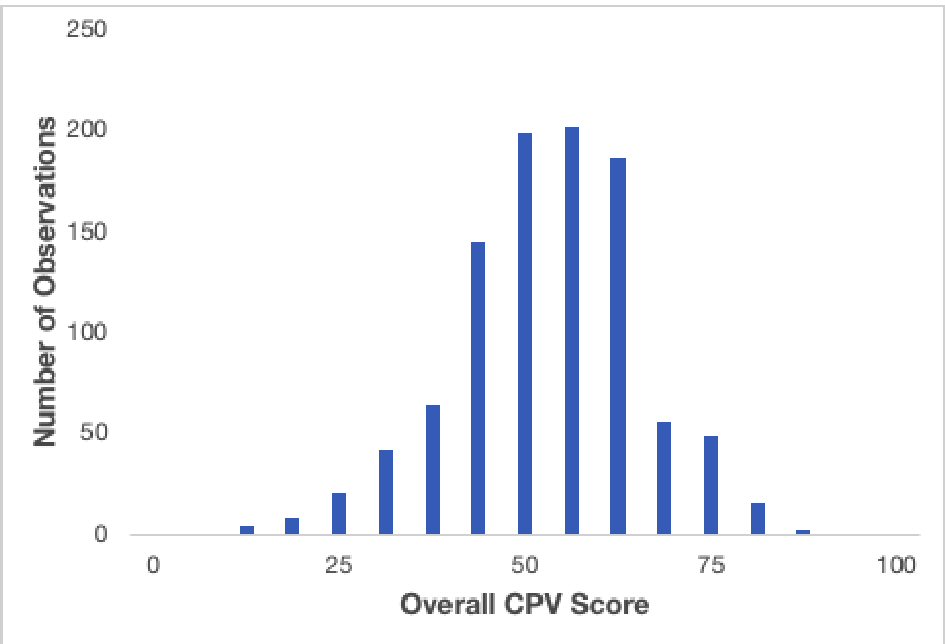
Figure 1. Histogram of overall CPV scores.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 10, Number 11, November 2018, pages 806-814
Drug-Drug Interaction Assessment and Identification in the Primary Care Setting
Figure
Tables
| N = 330 | |
|---|---|
| Male | 76.7% |
| Age | |
| < 40 | 6.4% |
| 40 - 55 | 60.9% |
| > 55 | 32.7% |
| Board certification | |
| Family medicine | 49.1% |
| Internal medicine | 49.7% |
| Both | 1.2% |
| Fellowship | 14.6% |
| Years in practice | 20.1 ± 6.9 |
| Region | |
| Midwest | 22.7% |
| Northeast | 25.5% |
| South | 30.9% |
| West | 20.9% |
| Locale | |
| Urban | 26.7% |
| Suburban | 60.9% |
| Rural | 12.4% |
| Practice type | |
| Solo private | 23.3% |
| Single specialty private | 37.6% |
| Multi-specialty private | 33.0% |
| Hospital | 6.1% |
| Employed by practice (%) | 74.6% |
| Multi-specialty practice | 32.7% |
| Medical practice setting (can choose more than one) | |
| Accountable care organization | 24.2% |
| Solo practice | 23.3% |
| Group practice | 66.4% |
| Hospital-based | 8.2% |
| Integrated delivery system | 11.5% |
| Network model HMO | 1.2% |
| Staff-model HMO (employed) | 1.2% |
| Staff-model HMO (FFS or group, contracted) | 1.2% |
| Other | 1.8% |
| Type of medication reconciliation used (physicians were able to choose > 1 ) | |
| Pharmacy/medication reconciliation | 88.2% |
| Presumptive drug tests | 57.3% |
| Definitive drug tests | 37.3% |
| Digital pills | 0.0% |
| Self-report | 62.7% |
| EMR/automated software | 74.6% |
| None | 1.0% |
| Time since last CME in pain management | |
| ≤ 12 months | 41.5% |
| 13 - 24 months | 17.0% |
| 25 - 36 months | 9.7% |
| > 36 months | 10.9% |
| Never taken | 20.9% |
| Receive quality bonus | 59.7% |
| If yes, metrics for preventive measures | 88.8% |
| Active panel size | 2,542 ± 1,526 |
| Patient panel characteristics | |
| On 5 or more medications | 41.2% |
| On opioid analgesics | 13.9% |
| Consume ≥ 2 alcoholic beverages/month | 55.4% |
| Payer type | |
| Medicare | 34.3% |
| Medicaid | 10.8% |
| Commercial | 48.1% |
| Self | 5.4% |
| Other | 1.4% |
| CPV domain | |
|---|---|
| Overall | 50.5 ± 12.0% |
| History | 64.6 ± 14.1% |
| Physical | 79.2 ± 24.8% |
| Workup | 54.9 ± 41.3% |
| Diagnosis-Treatment | 22.9 ± 16.9% |
| Ordered pharmacy medication reconciliation | 5.6% |
| Ordered presumptive or definitive drug test | 44.7% |
| Primary diagnosis | |
| Identified medical problem | 55.1% |
| Identified drug-drug interaction | 15.3% |
| Identified specific drug-drug interaction | 0.9% |
| Secondary diagnosis | 52.9% |
| Preventive measures | |
| Screening for cancer | 5.0% |
| Advised drug-drug interaction | 5.6% |
| Counseled on smoking cessation | 14.6% |
| Coordinate medications with all patient providers | 16.4% |
| Referral to psychiatrist | 46.6% |
| Referral to pain specialist | 22.4% |
| Number of low-value diagnostic workup ordered, per case | 0.8 ± 1.1 |
| Cost of low-value diagnostic workup ordered, per case | $121 ± $195 |
| Unnecessary measures | |
| Referral to neurology | 9.9% |
| Inappropriate admission to the hospital | 0.0% |
| OR | P-value | 95% CI lower | 95% CI upper | |
|---|---|---|---|---|
| Male | 0.99 | 0.957 | 0.64 | 1.53 |
| Age < 40 | 0.94 | 0.881 | 0.43 | 2.06 |
| South | 1.36 | 0.119 | 0.92 | 2.01 |
| Internal medicine | 1.06 | 0.751 | 0.73 | 1.55 |
| Hospital-based practice | 1.30 | 0.482 | 0.62 | 2.73 |
| Medical reconciliation tools used > 5 | 1.27 | 0.327 | 0.79 | 2.05 |
| More than 35% of patients with 5+ medications | 1.14 | 0.513 | 0.76 | 1.72 |
| Less than 10% of patients on opioids for pain | 1.32 | 0.169 | 0.89 | 1.95 |
| Asks about history of medications | 1.64 | 0.028 | 1.05 | 2.54 |
| Ordering a definitive drug test | 1.62 | 0.013 | 1.11 | 2.36 |
| CPV patient on psychiatric medications | 3.74 | 0.000 | 2.56 | 5.45 |
| CPV patient with polypharmacy/alcohol | 0.65 | 0.037 | 0.43 | 0.97 |
| Constant | 0.04 | 0.000 | 0.02 | 0.09 |
| OR | P-value | 95% CI lower | 95% CI upper | |
|---|---|---|---|---|
| Male | 0.73 | 0.066 | 0.52 | 1.02 |
| Age < 40 | 0.95 | 0.859 | 0.52 | 1.71 |
| South | 1.17 | 0.325 | 0.86 | 1.58 |
| Internal medicine | 0.86 | 0.324 | 0.65 | 1.15 |
| Hospital-based practice | 2.59 | 0.002 | 1.41 | 4.76 |
| Medical reconciliation tools used ≥ 5 | 0.90 | 0.600 | 0.61 | 1.33 |
| More than 35% of patients with 5+ medications | 0.99 | 0.953 | 0.73 | 1.35 |
| Less than 10% of patients on opioids for pain | 1.12 | 0.462 | 0.83 | 1.51 |
| Asks about history of medications | 1.04 | 0.821 | 0.76 | 1.42 |
| Ordering a definitive drug test | 1.51 | 0.006 | 1.13 | 2.02 |
| Identified a drug-drug interaction exists | 3.32 | 0.000 | 2.21 | 4.99 |
| CPV patient on psychiatric medications | 1.86 | 0.000 | 1.36 | 2.53 |
| CPV patient with polypharmacy/alcohol | 0.25 | 0.000 | 0.18 | 0.34 |
| Constant | 0.70 | 0.193 | 0.41 | 1.20 |