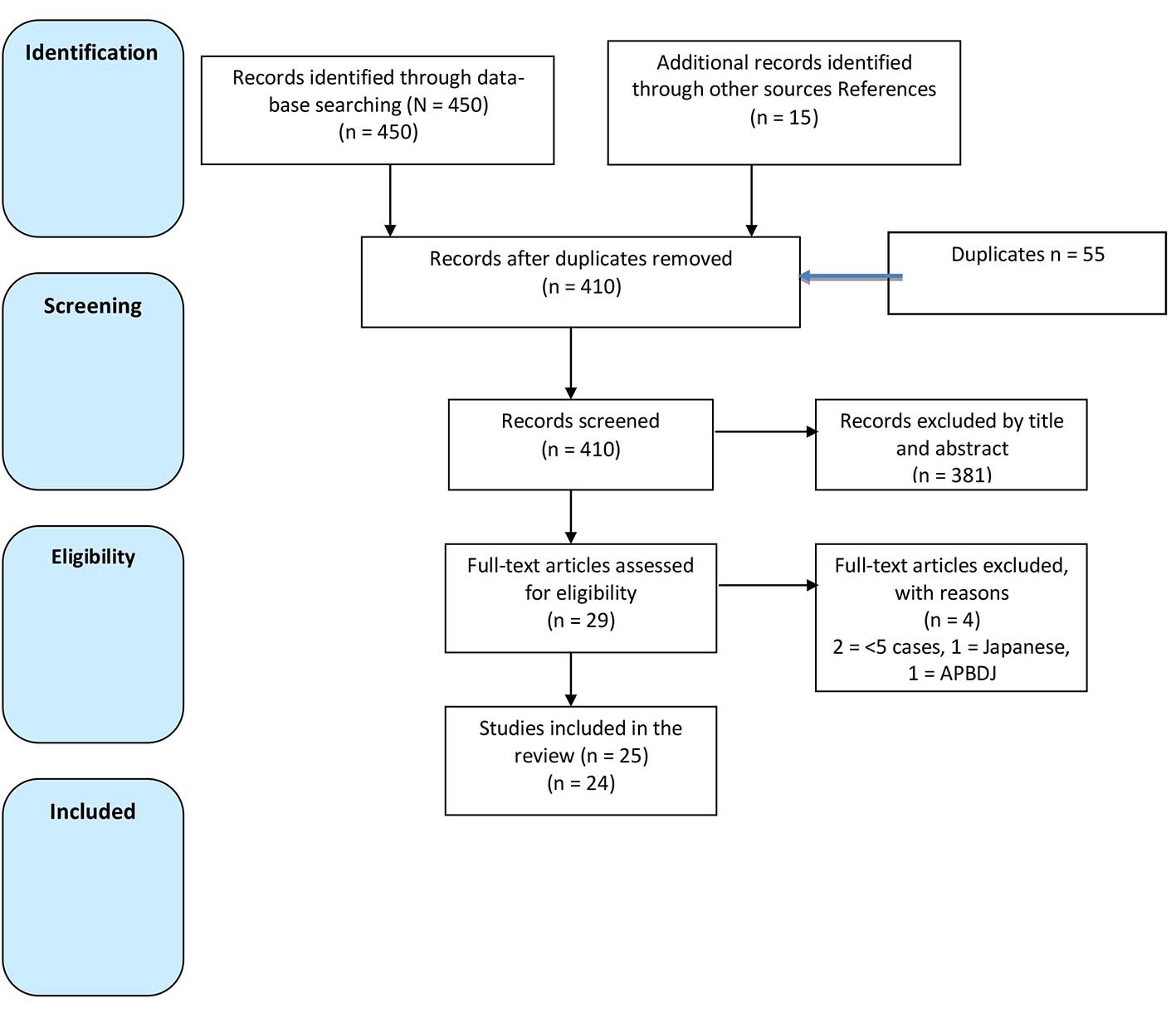
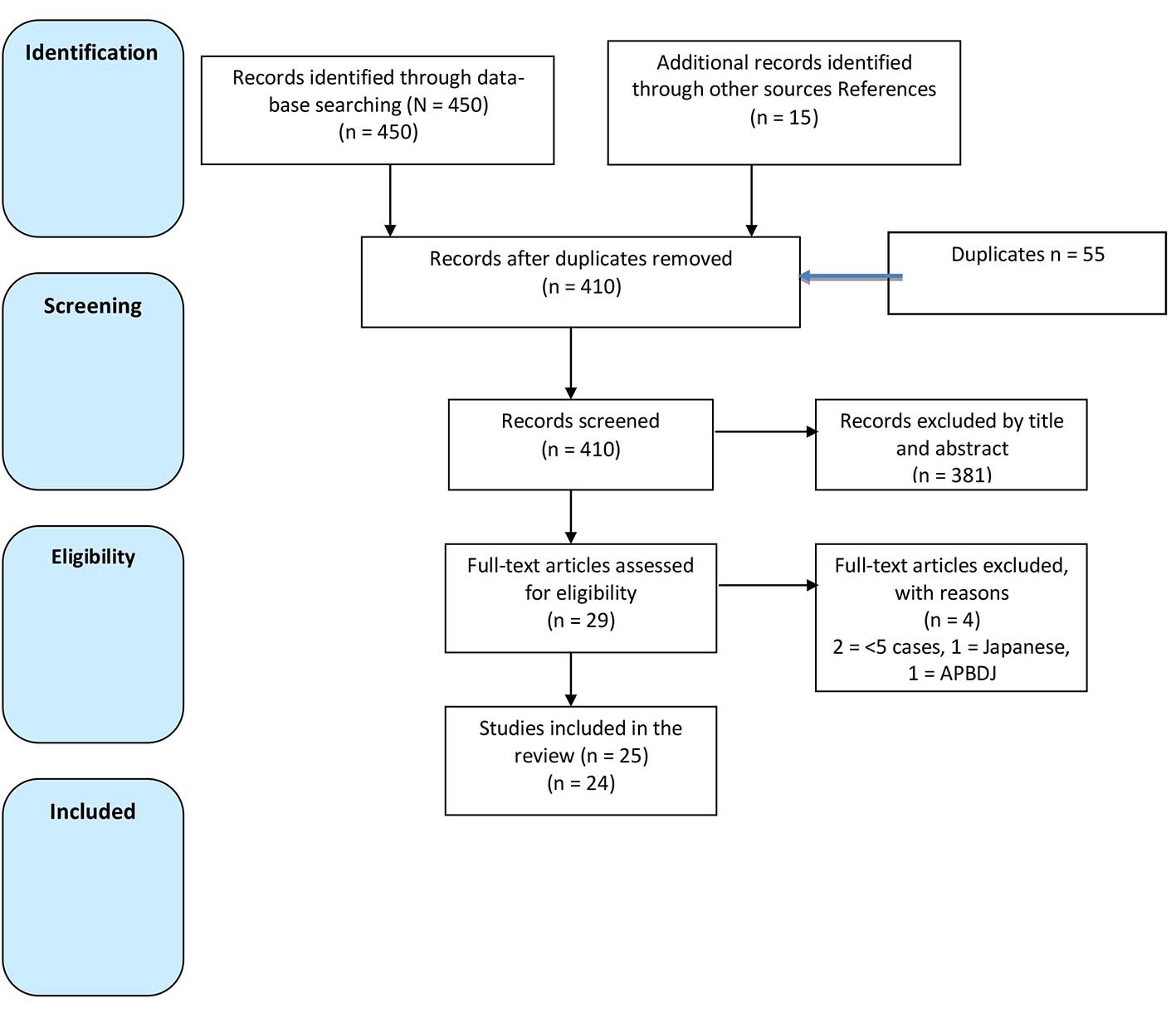
Figure 1. Flow diagram of selected studies.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Review
Volume 9, Number 2, February 2017, pages 81-91
To Resect or Not to Resect Extrahepatic Bile Duct in Gallbladder Cancer?
Figure
Tables
| Author, year, country, study type | Number of patients (n) | Age (range) | Gender M/F | Definitions | EHBDR, n (%) | 5-years OS |
|---|---|---|---|---|---|---|
| AJCC: American Joint Committee on Cancer; APBDJ: Anomalous pancreatobiliary duct junction; BDI: bile duct invasion; EHBDR: extrahepatic bile duct resection; DFS: disease free survival; EHBDNR: extrahepatic bile duct non-resection; JSBS: Japanese Society of Biliary Surgery; HDL: hepatoduodenal ligament; PBM: pancreatobiliary maljunction; UICC: union for international cancer control; RA: retrospective analysis; R: resected; NR: non-resected; St: stage; SS: subserosal; w/o: without. | ||||||
| Pandey et al [17] | 17 | 51 (35 - 62) | 5/12 | AJCC seventh | 17 (100) | 26 months |
| 2015 | ||||||
| India | ||||||
| RA | ||||||
| He et al [10] | 152 | 68 (29 - 89) | 61/91 | AJCC seventh | 57 total | 26% |
| 2015 | St I = 6 (33) | |||||
| China | St II = 9 (36) | |||||
| Telephone FU RA | St III = 42 (55) | |||||
| Hwang et al [28] | 103 | 61.6 ± 10 (35 - 84) | 36/67 | AJCC seventh | 28 (28) | T3N0 = 58% |
| 2015 | T1N1 = 15% | |||||
| Korea | T2N1 = 29% | |||||
| RA | T3N1 = 5% | |||||
| Choi et al [19] | 71 | 64 (22 - 82) | 32/39 | AJCC seventh | 30 (42.25) | R pT2 = 56% |
| 2013 | NR pT2 = 76% | |||||
| Korea | R pT3 = 39% | |||||
| RA | NR pT3 = 54% | |||||
| Gwark et al [23] | 48 | 63 ± 83.3 | 23/25 | NR | 16 (33) | 62% |
| 2012 | ||||||
| Korea | ||||||
| RA | ||||||
| Shirai et al [25] | 145 | 66.5 (43 - 84) | 42,430 | AJCC seventh | 52 (36) | 65% |
| 2012 | ||||||
| Japan | ||||||
| RA | ||||||
| Nasu et al [14] | 38 | 71 (58 - 83) | 13/14 | AJCC seventh | 27 (71) | 34% |
| 2012 | ||||||
| Japan | ||||||
| RA | ||||||
| Nishio et al [15] | 100 | 63 (37 - 79) | 30/43 | AJCC seventh | 87 (87) | 36% |
| 2011 | ||||||
| Japan | ||||||
| RA | ||||||
| Lim et al [30] | 10 | 58 ± 10.4 (27 - 72) | AJCC sixth | 10 (100) | 10% | |
| 2012 | ||||||
| Korea | ||||||
| RA | ||||||
| Agarwal et al [16] | 14 | 49 (21 - 68) | 42,677 | AJCC sixth | 14 (100) | OS: not given |
| 2007 | DFS: 24 months | |||||
| India | ||||||
| RA | ||||||
| Fuks et al [31] | 218 | 64 (31 - 88) | 67 - 151 | AJCC seventh | 63 (43) | 41% |
| 2011 | ||||||
| France | ||||||
| RA | ||||||
| Araida et al [18] | 4,243 | EHBDNR = 68 ± 12.5 | BDNR = 160/233; BDR = 67/127 | JSBS fifth edition | 2,897 (68) 838 pT2,3,4 w/o HDL and cystic duct invasion | R = 75% |
| 2009 | EHBDR = 65.2 ± 11.2 | NR = 65% | ||||
| Japan | ||||||
| RQS multicentre study | ||||||
| Kohya et al [22] | 84 | 67.6 (45 - 87) | 27 - 57 | AJCC sixth | 30 (36) | 100% in ss min and med, ssmas = 59.7% |
| 2010 | ||||||
| Japan | ||||||
| RA | ||||||
| Kayahara et al [7] | 4,424 | Cholelithiasis = 66.9 | 1,608 M/2,816 | AJCC fifth | 2,141 (48) | < 60 years 34% - > 60 years 28% |
| 2008 | APBDJ = 58.6 | |||||
| Japan | De novo = 65.8 | |||||
| Retrospective survey | ||||||
| You et al [20] | 290 | 60.9 ± 9.4 | 25 - 27 | AJCC fifth | 17 (6) | T1b = 96% |
| 2008 | ||||||
| Korea | ||||||
| RA | ||||||
| Yokomizo et al [27] | 94 | 68.6 (48 - 91) | 39 - 55 | JSBS fifth edition | 11 (12) | EBDR = 67% |
| 2007 | EHBDNR = 81% | |||||
| Japan | ||||||
| RA | ||||||
| Sakamoto et al [24] | 110 | 67 (32 - 80) | 41 - 59 | UICC sixth | 58 (53) | Perineural(+)EHBDR = 46% |
| 2006 | EHBDNR = 0% | |||||
| Japan | ||||||
| RA | ||||||
| Yagi [33] | 63 | 66 (48 - 84) | 30 - 33 | UICC fourth | 12 (19) | St I = 100% |
| 2006 | ST II = 68% | |||||
| Japan | St IIA = 0% | |||||
| RA | St IIB = 17% | |||||
| St III = 25% | ||||||
| St IV = 15% | ||||||
| Shimizu et al [11] | 50 | 67 ± 8 (44 - 84) | 18 - 32 | UICC fifth | 50 (100) | Mean = 14 months |
| 2004 | ||||||
| Japan | ||||||
| RA | ||||||
| Suzuki et al [26] | 20 | 63.5 (40 - 80) | 42,125 | UICC sixth | 12 (60) | 77% |
| 2004 | Mean survival = 64 months | |||||
| Japan | ||||||
| RA | ||||||
| Kaneoka et al [12] | 59 | 65.6 | 14 - 45 | UICC fifth | 59 (100) | No survivors with BDI |
| 2003 | ||||||
| Japan | ||||||
| RA | ||||||
| Toyonaga et al [32] | 73 | 65.7 | 33 - 40 | AJCC fifth | 18 (25) | pT2 = 54% |
| 2003 | pT3 = 0% | |||||
| Japan | ||||||
| RA | ||||||
| Kondo et al [29] | 72 | 69.5 (53 - 79) | 22 - 50 | UICC fifth | 54 (75) | 0% |
| 2003 | ||||||
| Japan | ||||||
| RA | ||||||
| Wakai et al [21] | 126 | 69 (38 - 94) | 39 - 87 | AJCC fifth | 35 (28) | Direct invasion = 57% |
| 2003 | Portal tract = 17% | |||||
| Japan | ||||||
| RA | ||||||
| Tashiro et al [34] | 1,627 | PBM type A = 24 ± 23.9 (5 - 83) | Type A= 1/3.2 | The Japanese Study Group Pancreatobiliary Maljunction | Type A = 837 (78) | NR |
| 2003 | Type B = 90 (45) | |||||
| Japan | PBM type B = 47 ± 19.3 (6 months - 80 years) | Type B = 1/2.7 | Total = 927 (57) | |||
| Retrospective nationwide survey | ||||||
| Total | 12,251 | 6,722 (55) | ||||
| Topic | Findings | Reference |
|---|---|---|
| Pancreatobiliary maljunction and gallbladder cancer | APBDJ with dilatation: cholecystectomy and EHBDR recommended APBDJ without dilatation: EHBDR contentious, no consensus | [34] |
| Cancer survival: all stages | All stages survival rate in Japan 9-83%, in west 2.7-15% | [7-9] |
| Hepatoduodenal ligament invasion | Types of HDL invasion: Type I: direct Extramural spread Type II: continuous intramural spread Type III: distant spread separated from the primary tumor Type IV: spread of cancer cells from metastatic lymph nodes | [11-13, 35] |
| HDL = LNI + BDI | ||
| Histologic patterns of BDI and occurrence rate: Direct 52% Lymphatic and/or venous 28% Perineural 84% | ||
| New classification of cystic duct cancer into: Hepatic hilum Cystic confluence | ||
| Modes of Hepatic spread: Direct Portal tract invasion Hepatic metastatic nodules | ||
| Outcome in EHBDR and EHBDNR | Patients undergoing EHBDR had similar survival to those that did not (EHBDNR) in pT2, T3, T4 R0 resections. Routine use of EHBDR in this group is unsupported by the literature | [18, 19] |
| pT1b tumors | Operative strategy: T1a: Simple cholecystectomy T1b: No clear agreement in terms of operative strategy | [20] |
| pT2 tumors | Subserosal invasion: Is an important factor in incidental GB cancer survival Radical cholecystectomy is indicated in incidental T2 tumors if > 2 mm serosal invasion is present Classification Minimal Medium Massive Perineural invasion and LN metastases correlates with medium and massive invasion Survival: No survival benefit between LN(+) and LN(-). Profit of radical intervention only if < 2 LNs are positive | [21, 22, 25] |
| T3/T4 tumors | Prognosis: stage T3N1 has worse prognosis than stage IVB even after R0 resection. Hepatopancreatoduodenectomy (HPD): Morbidity 91.3% Mortality 13% 5-year survival: 10% Indications of HPD: Direct invasion of the duodenum, pancreas, liver Hilar involvement and peripancreatic lymph node metastases Karnofsky score 70. | [28, 30] |
| Incidental GB cancer | Re-operation increases survival in pT2,T3 | [31, 32] |