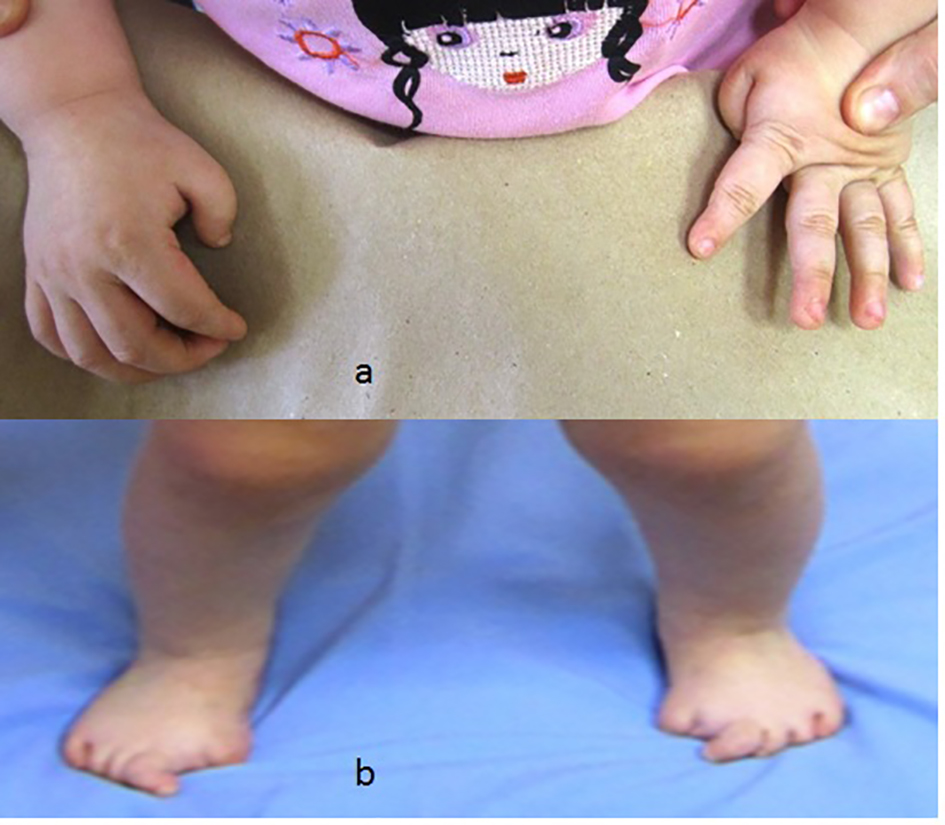
| Patient 1 | 6 months old, female | - | Congenital halux valgus | + | - | Negative for ACVR1 gene mutation | Normal | None | 1) Congenital flexion deformity of the thumbs
2) Unusual stiffness of the spine |
| Two patients of same age group | 6 - 11 months old, two males | - | Congenital hallux valgus | + | - | Positive ACVR1 mutation (R206H) | Normal | None | Congenital flexion deformity of the thumbs |
| Patient 4 | 5 years old, female | Three years | Congenital hallux valgus | + | ++ | Was tested primarily for FBN1 gene which was negative. Then, positive for ACVR1 gene mutation (R206H) | Two times greater than normal | None | Marfanoid habitus |
| Two patients same age group | 7 - 8 years old, two males | Four years | Congenital hallux valgus | - | +++ | Was tested primarily for FBN1 gene and showed negative results | Two times greater than normal | None | Marfanoid habitus with extreme stiffness of the spine and pain |
| Patient 7 | 7 years old, female | Three years | Congenital hallux valgus | None | Torticollis associated with swellings over the neck | Positive ACVR1 gene mutation (R206H) | Three times greater than normal | None | Marfanoid habitus associated with painful hips and knees |
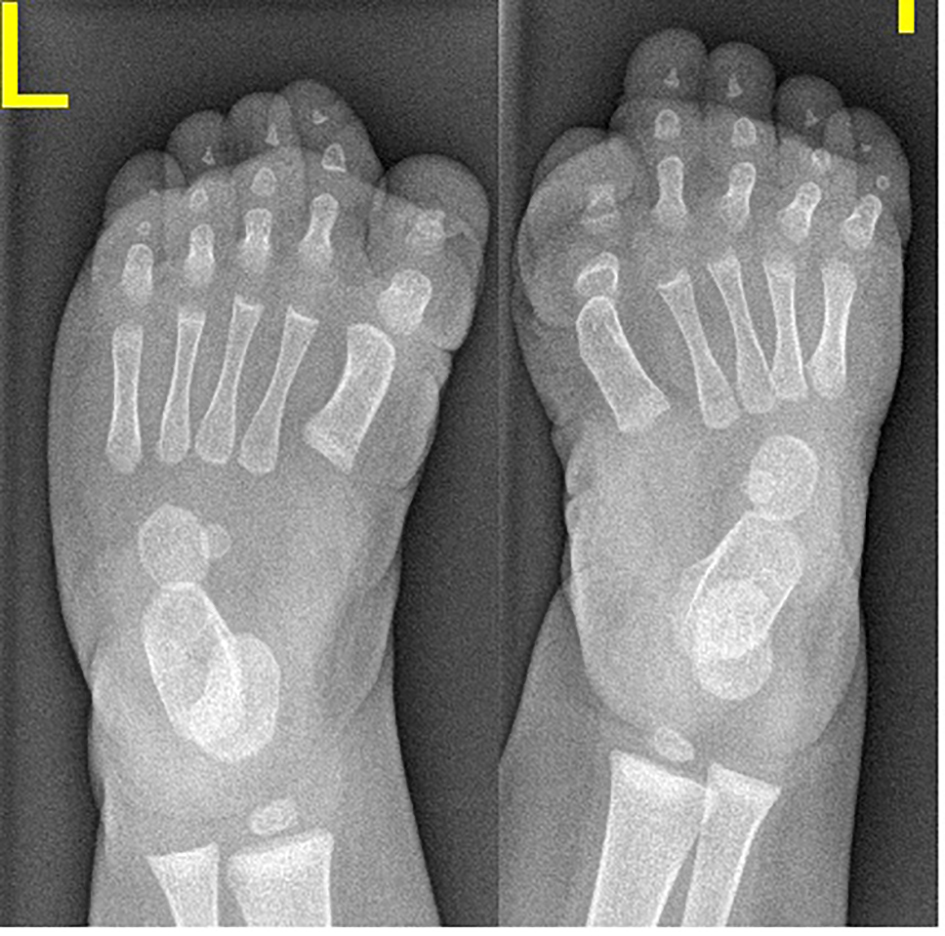
| Patient 8 | 14 years old, female | Seven years | Monophalangia of the big toes | Monophalangia of the big toes | ++ | No genetic tests performed | Three times greater than normal | None | Painful ankylosis of all major joints |
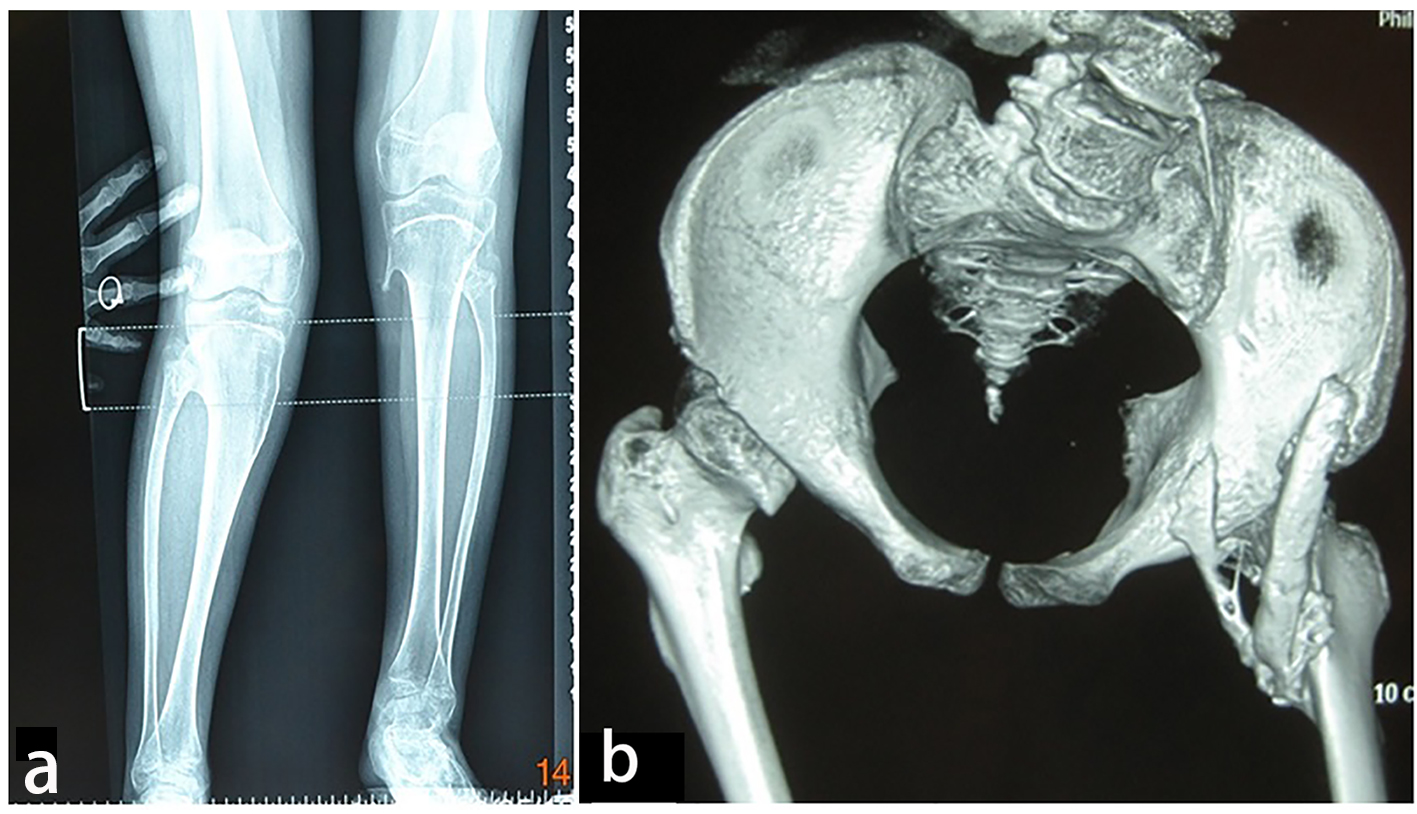
| Patient 9 | 13 years old, female | Ten years | Monophalangia of the big toes | Monophalangia of the big toes | ++ | Positive ACVR1 gene mutation (R206H) | Three times greater than normal | None | Extra-articular ankylosis of the left knee |
| Patient 10 | 14 years old, female | Seven years | Malformed big toes with superimposed ankyloses of the proximal phalanx with the metatarsal of the first digit of the foot | Severe microdactyly of the big toes | ++ | Was tested primarily for FBN1 gene and showed negative | Alkaline phosphatase levels were four times greater than normal in the period of 10 weeks after the inciting trauma | None | Clinically diagnosed as Marfan syndrome |
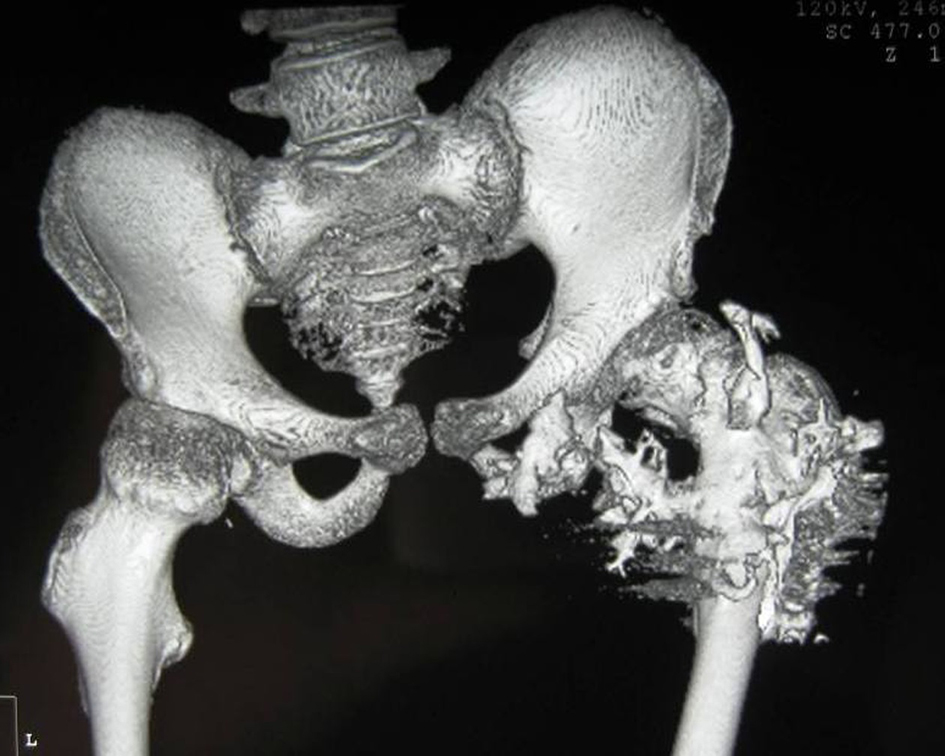
| Patient 11 | 16 years old, female | Ten years | Congenital hallux valgus associated with Marfanoid habitus | ++ | - | Positive ACVR1 gene mutation (R206H) | Alkaline phosphatase levels were four times greater than normal in the period of 12 weeks after the inciting trauma | None | Massive heterotopic ossification around the pelvis and the upper shaft of the left femur and the ischium pubis with eventual development of extra-articular ankyloses |