Figures
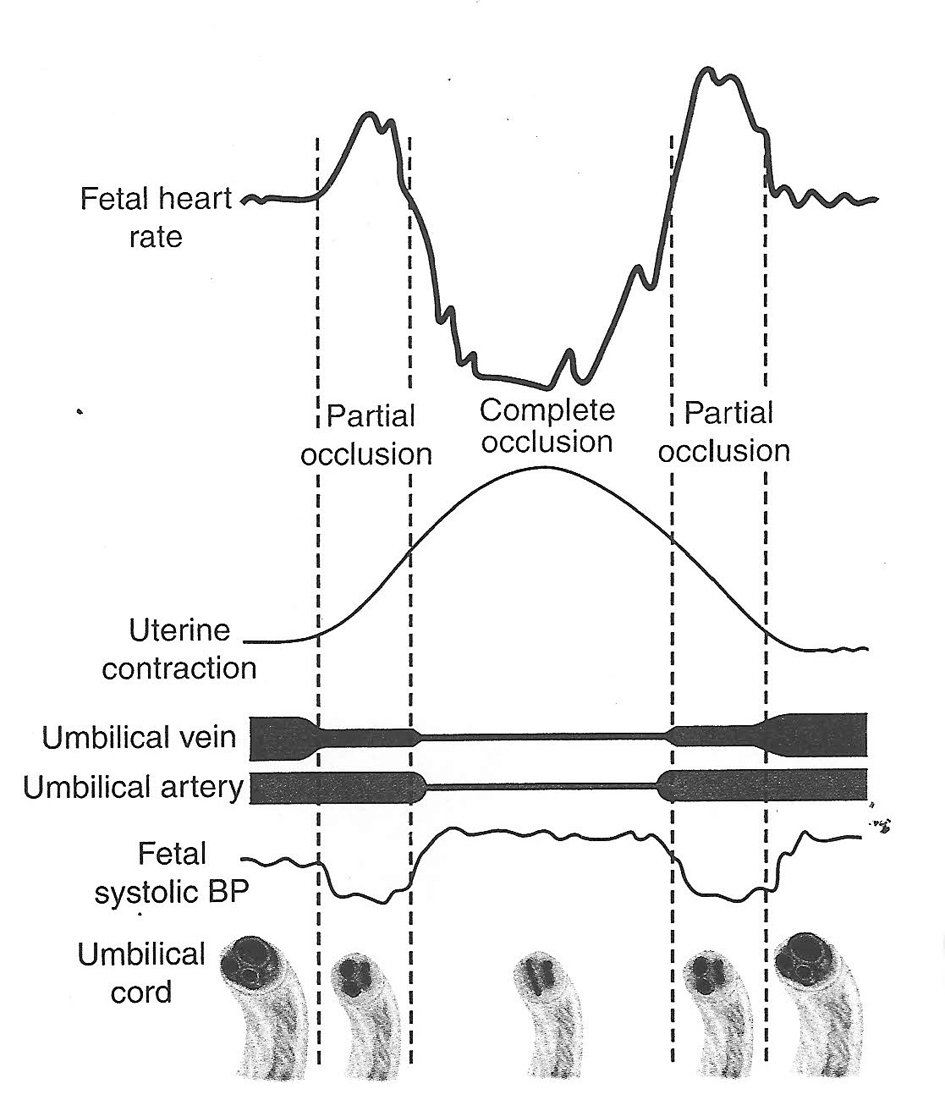
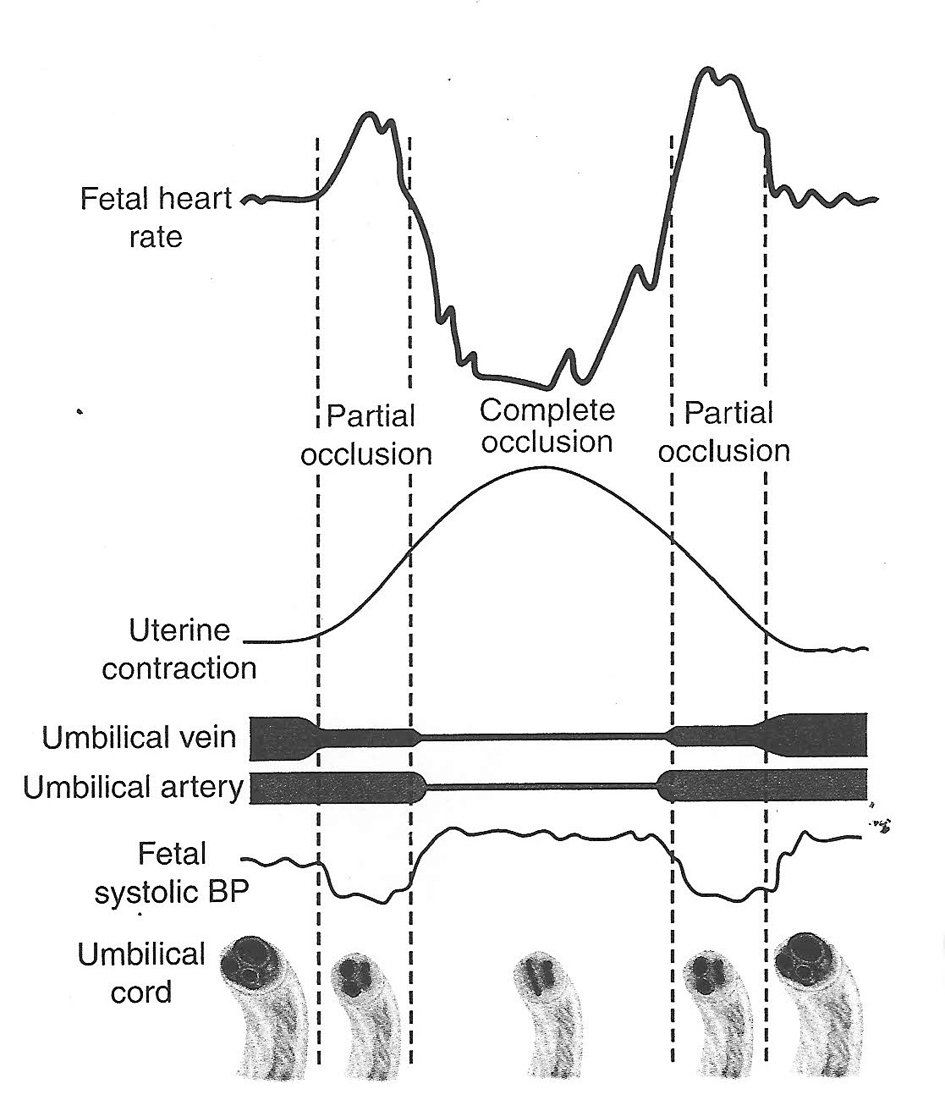
Figure 1. Hypothesis of cord compression and variable deceleration [25, 27, 29, 30] (thankfully reproduced from OJOG 2013;3:362-370, open access) [23]. This hypothesis has major fallacies. Complete cord compression has been postulated for these most common decelerations (CTG paper speed 3 cm/min). The FHR recovery commencing at the height of contraction (where umbilical arterial and venous occlusion is unrelieved) cannot be explained. Instead the deceleration depicted seems consistent with “direct” or “pure” vagal reflex (head compression).
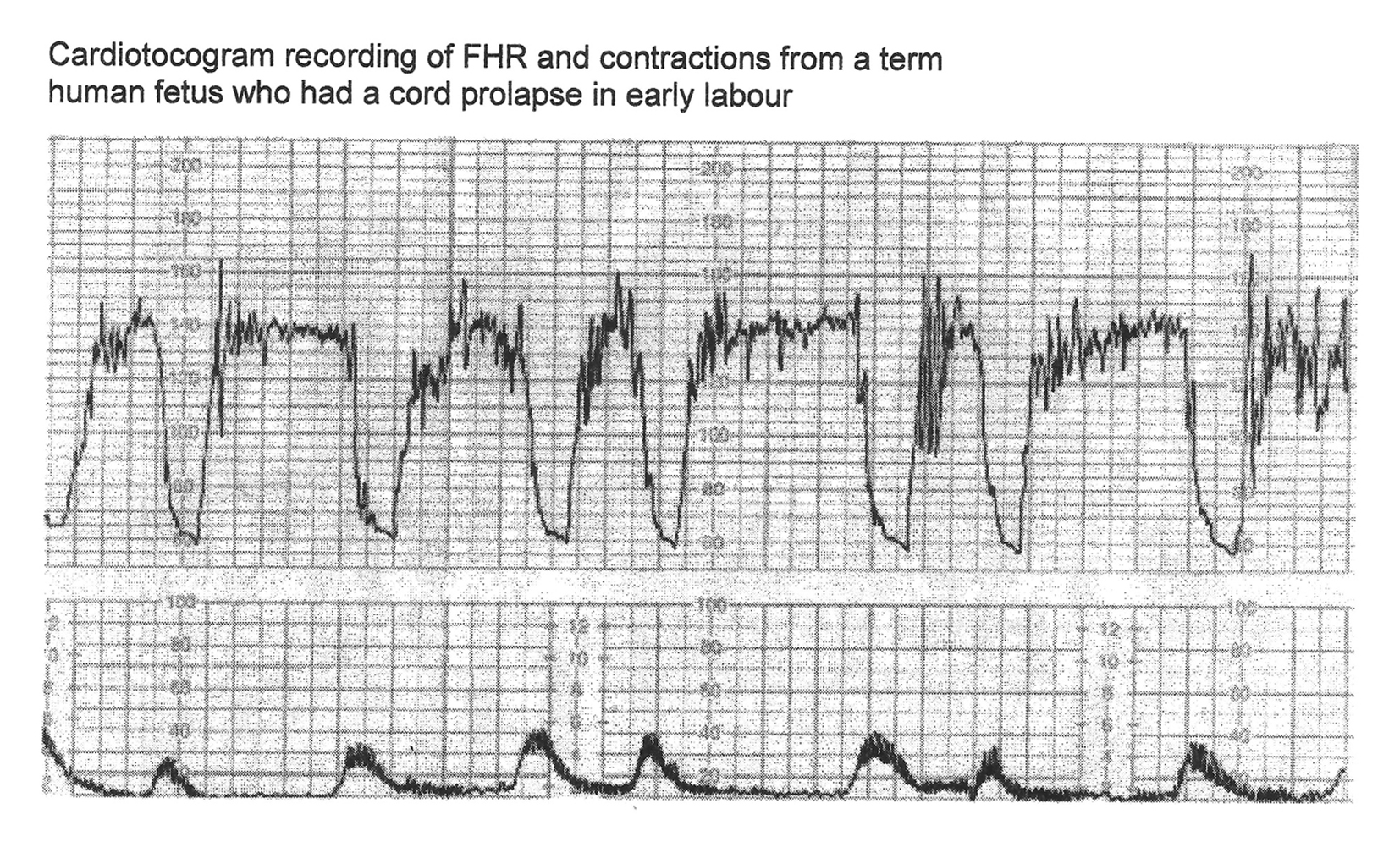
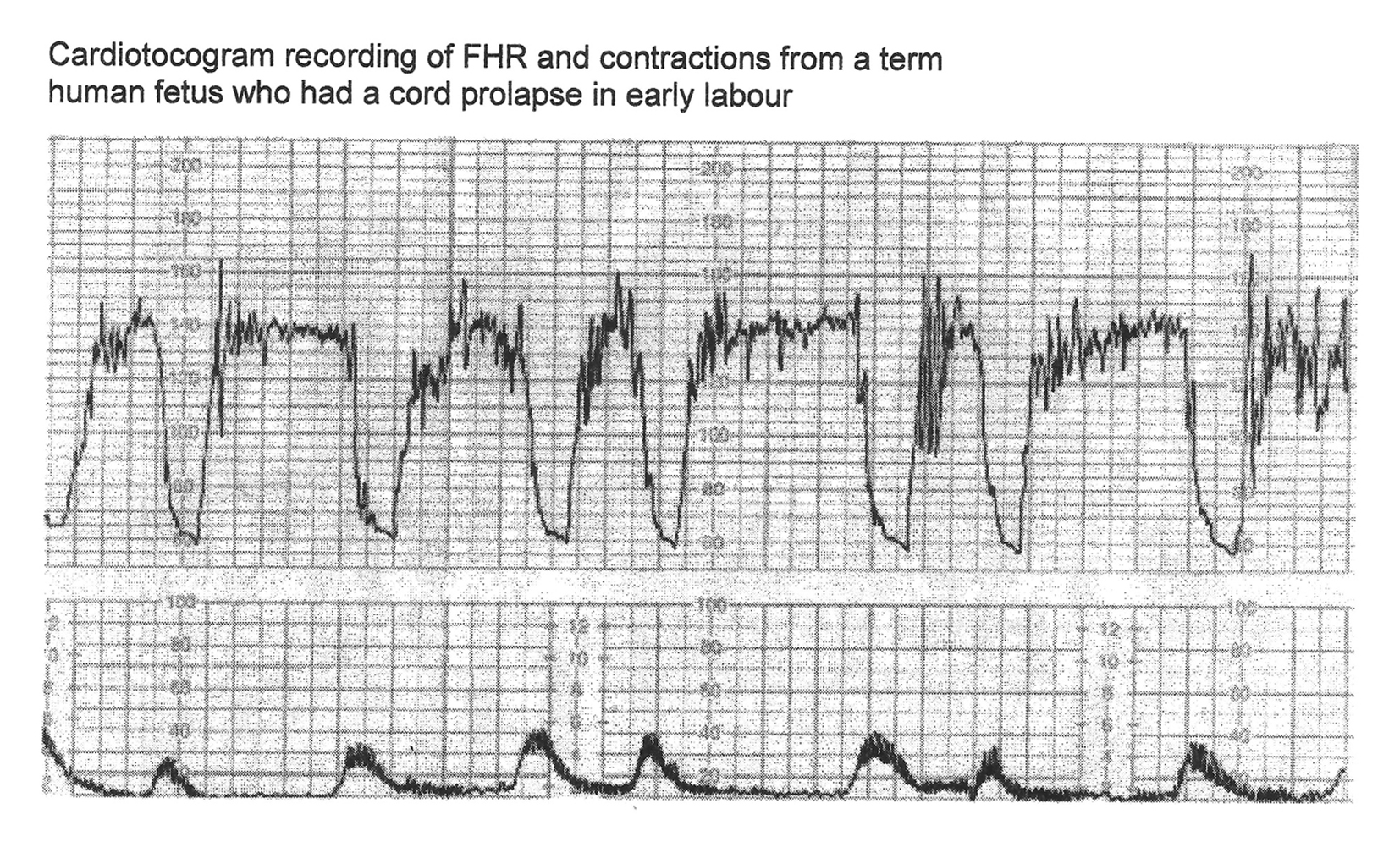
Figure 2. CTG in a case of cord prolapse showing decelerations (mistakenly) classed as “variable” (reproduced with thanks from Westgate et al, AJOG, 2007) [1]. Although these decelerations “look” rapid (paper speed 1 cm/min), the “descent time” is well over 60 s.
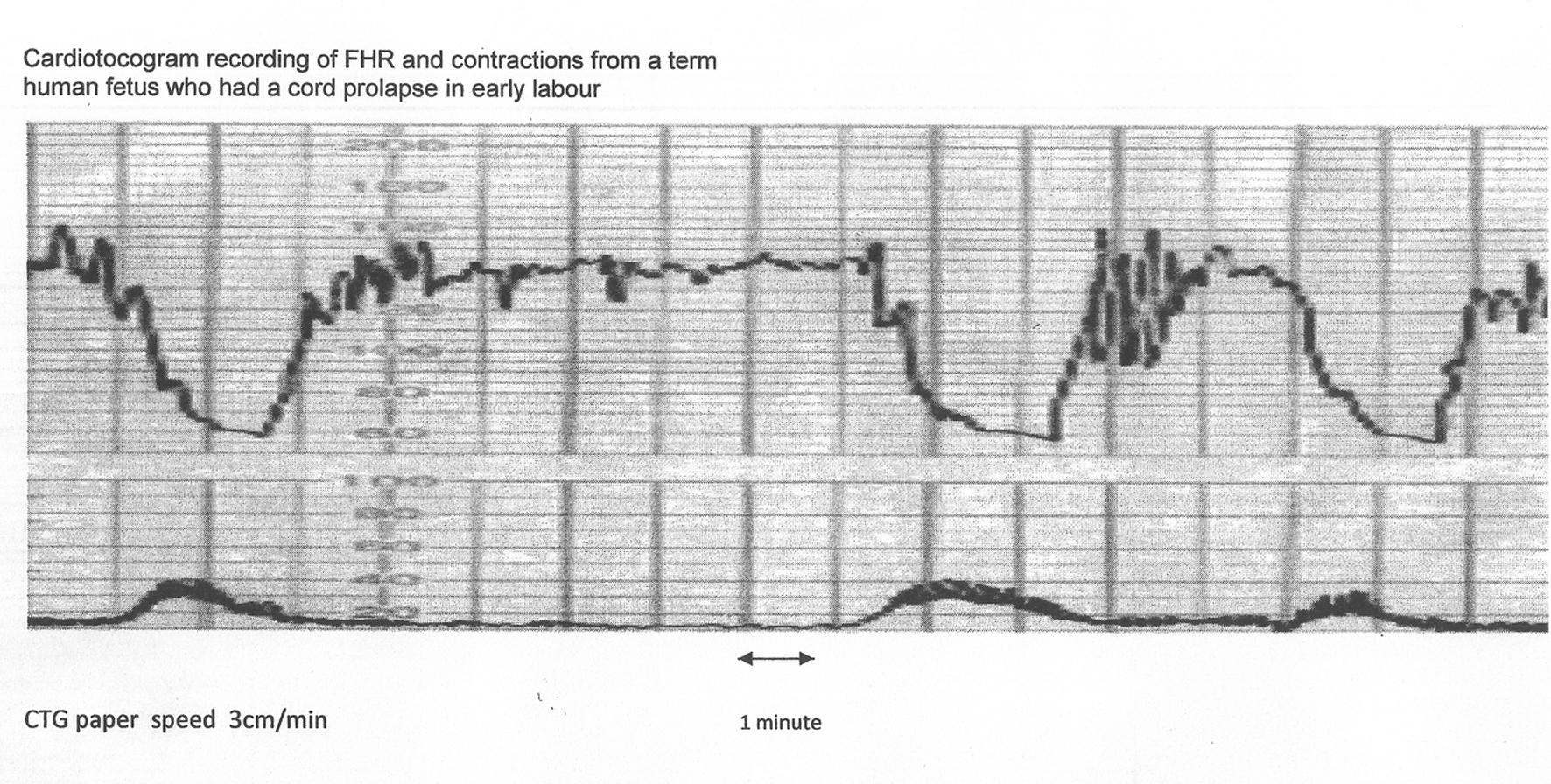
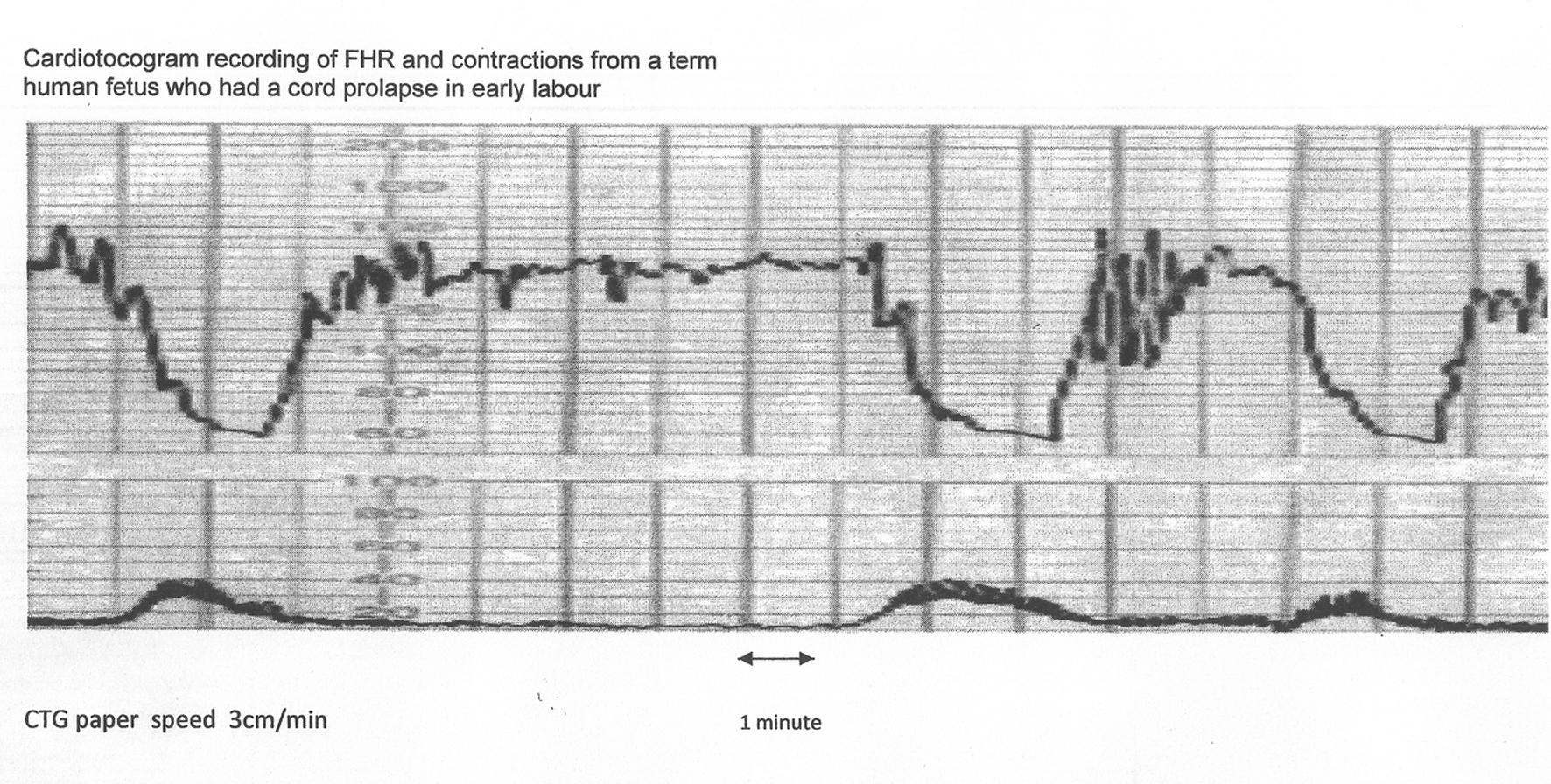
Figure 3. The same CTG from Figure 2 shown with American CTG paper speed of 3 cm/min. Note that the “descent time” is well over 60 s. Hence, based on American definitions [10, 11], these decelerations are “late”, demonstrating that rate/time of descent does not reliably predict etiology.
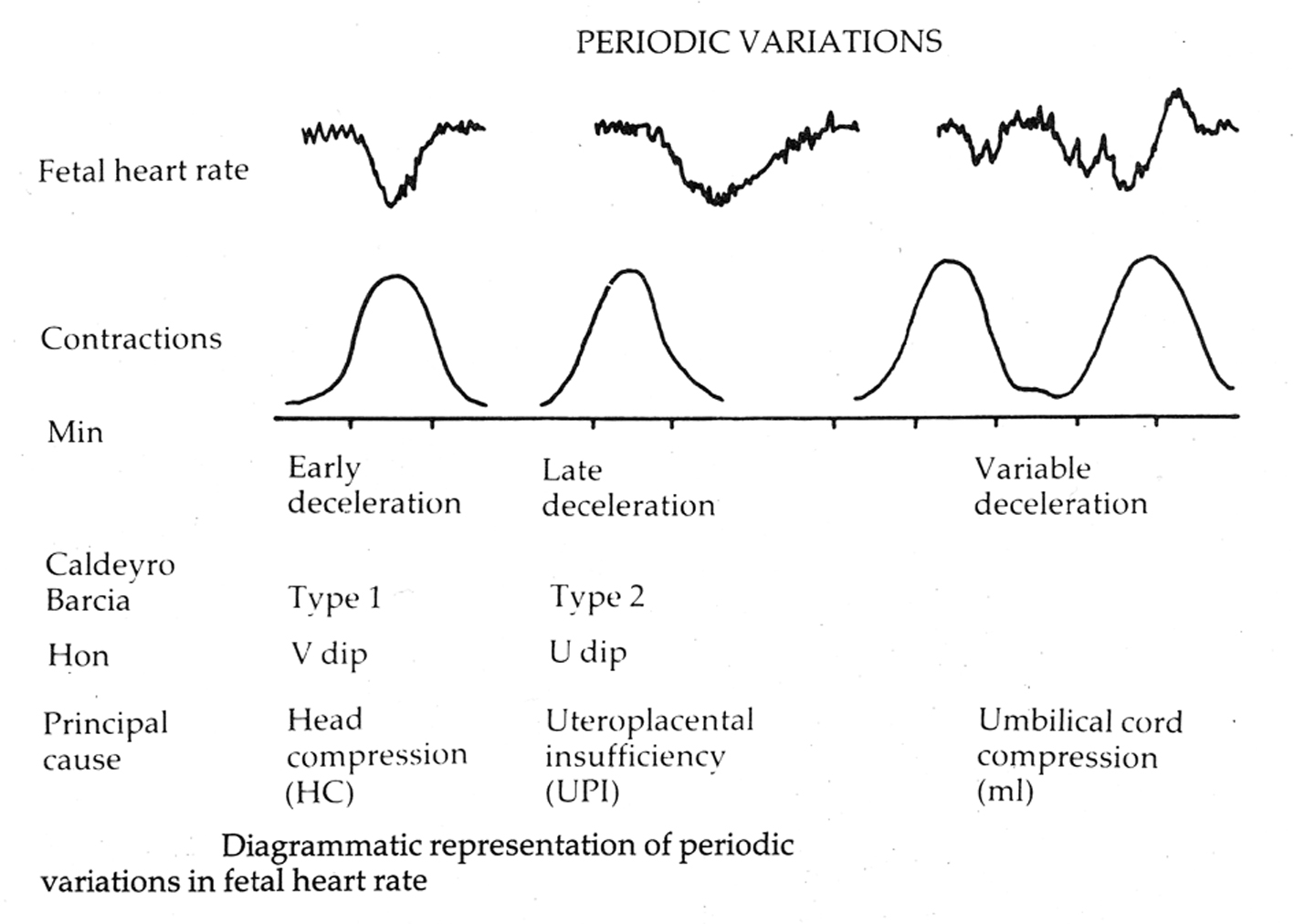
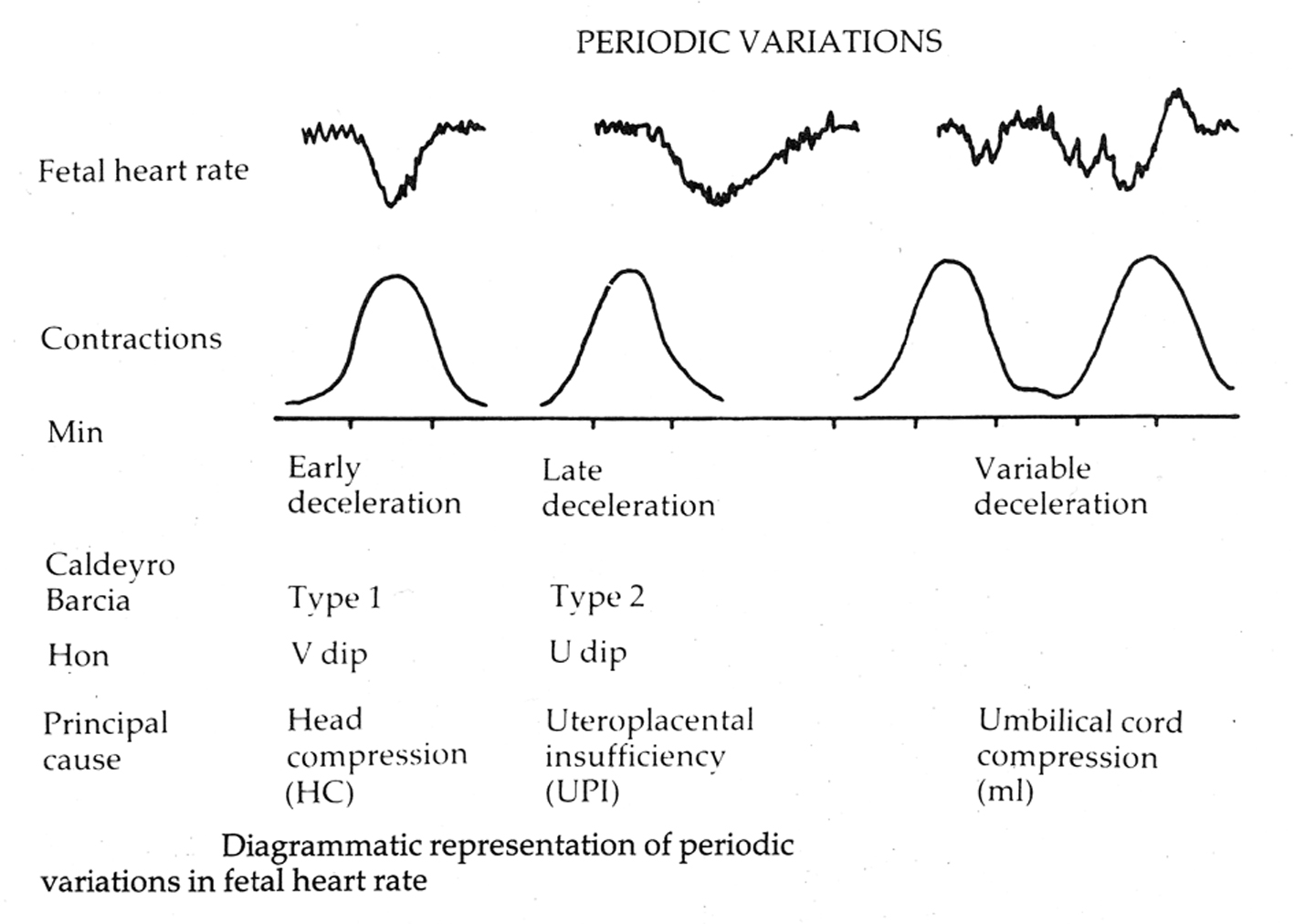
Figure 4. Diagrammatic representation of early, late and variable decelerations as practiced in British Obstetrics before 2007 (reproduced with kind permission from “Principles of Obstetrics” by Bryan Hibbard, 1988) [20]. Note the apparent rapid descent of early decelerations.
Tables
Table 1. A Large Study by Cahill et al (2012) Showing That 91% of Acidemic Babies Displayed Moderate Variability During the 30 Min Before Delivery [12]
| FHR pattern | pH ≤ 7.10 (57 newborns) | pH > 7.10 (5,331 newborns) | P value |
|---|
| There were hardly any “early” decelerations in this large study, not because head compression does not cause decelerations, but very likely because of accident of (flawed) definitions. Late decelerations of duration < 60 s (i.e. descent time < 30 s) may have been wrongly classed as “variable”. |
| Moderate baseline variability | 91.2% | 87.2% | - |
| Minimal baseline variability | 8.8% | 12.5% | 0.41 |
| Baseline tachycardia | 12.3% | 4.5% | - |
| Repetitive late decelerations | 15.8% | 7.3% | 0.05 |
| Repetitive variable decelerations | 49.1% | 32.5% | 0.03 |
| Early decelerations | None | None | - |
Table 2. Proposed Physiological Categorization of FHR Decelerations [6, 26]
| The confusing term “uniform” is avoided. #“Recurrent” - associated with more than 50% contractions [11]. *The 20 s lag-time is based on expert consensus [24] and seems practically useful. |
| Early decelerations | Recurrent# slowing of FHR with onset early in the contraction and return to baseline at the end of contraction. |
| Late decelerations | Recurrent slowing of FHR with onset mid to end of contraction and nadir more than 20 s* after peak of contraction and ending after the contraction. If baseline variability is less than 5 beats/min, then the definition would include decelerations less than 15 beats/min. |
| Variable decelerations | Recurrent slowing of FHR with varying time relationship to the contraction cycle. They tend to markedly vary in shape. |