| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 10, Number 3, March 2018, pages 268-276
Correlation of Clinical and Radiological Outcome After Anterior Cervical Discectomy and Fusion With a Polyetheretherketone Cage
Savvas L. Spanosa, b, h, Ioannis D. Siasiosc, d, e, Vassilios G. Dimopoulosc, d, Konstantinos N. Paterakisa, Dimos S. Mastrogiannisf, Theofanis P. Giannisg, Aggeliki A. Fotiadoua, John Pollinac, d, Kostas N. Fountasa, g
aDepartment of Neurosurgery, School of Medicine, University of Thessaly, Larissa, Greece
bDepartment of Physiotherapy, School of Health and Welfare, Technological Education Institute of Sterea Ellada, Lamia, Greece
cDepartment of Neurosurgery, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, State University of New York, Buffalo, NY, USA
dDepartment of Neurosurgery, Kaleida Health, Buffalo, NY, USA
eDepartment of Neurosurgery, Papageorgiou Hospital, Thessaloniki, Greece
fDepartment of Nursing, School of Health and Welfare, Technological Education Institute of Sterea Ellada, Lamia, Greece
gDepartment of Neurosurgery, University Hospital of Larissa, Larissa, Greece
hCorresponding Author: Savvas Spanos, Department of Physiotherapy, Technological Education Institute of Sterea Ellada, 3rd km Old National Road Lamia-Athens, Lamia 35100, Greece
Manuscript submitted December 16, 2017, accepted January 8, 2018
Short title: Clinical and Radiological Outcome After ACDF
doi: https://doi.org/10.14740/jocmr3326w
| Abstract | ▴Top |
Background: Anterior cervical discectomy and fusion (ACDF) with a polyetheretherketone (PEEK) cage is considered as the gold standard for patients with cervical disc disease. However, there are limited in vivo data on the impact of ACDF on the cervical kinematics and its association with patient-reported clinical outcomes. The purpose of this study was to investigate the impact of altered cervical sagittal alignment (cervical lordosis) and sagittal range of motion (ROM) on patients’ self-reported pain and functional disability, after ACDF with a PEEK cage.
Methods: We prospectively studied 74 patients, who underwent single-, or consecutive two-level ACDF with a PEEK interbody cage. The clinical outcomes were assessed by using the pain numeric rating scale (NRS) and the neck disability index (NDI). Radiological outcomes included cervical lordosis and C2-C7 sagittal ROM. The outcome measures were collected preoperatively, at the day of patients’ hospital discharge, and also at 6 and 12 months postoperatively.
Results: There was a statistically significant reduction of the NRS and NDI scores postoperatively at each time point (P < 0.005). Cervical lordosis and also ROM significantly reduced until the last follow-up (P < 0.005). There was significant positive correlation between NRS and NDI preoperatively, as well as at 6 and 12 months postoperatively (P < 0.005). In regard to the ROM and the NDI scores, there was no correlation preoperatively (P = 0.199) or postoperatively (6 months, P = 0.322; 12 months, P = 0.476). Additionally, there was no preoperative (P = 0.134) or postoperative (6 months, P = 0.772; 12 months, P = 0.335) correlation between the NDI scores and cervical lordosis.
Conclusions: In our study, reduction of cervical lordosis and sagittal ROM did not appear to significantly influence on patients’ self-reported disability. Such findings further highlight the greater role of pain level over the mechanical limitations of ACDF with a PEEK cage on patients’ own perceived recovery.
Keywords: Anterior cervical discectomy and fusion; Cervical ROM; Neck disability index; Numeric rating scale; Pain; PEEK cage; Cervical lordosis
| Introduction | ▴Top |
Anterior cervical discectomy with fusion (ACDF) constitutes one of the most commonly performed procedures in spine surgery, characterized by quite high success and low complication rates. ACDF is regarded as the standard surgical treatment option for cervical spondylosis with myelopathy, radiculopathy and/or symptomatic disc herniation, when conservative management has failed. The reported results for ACDFs are excellent for the patients, as this is generally stated in the pertinent literature [1, 2]. ACDF in the vast majority of cases successfully reduces neck and arm pain, restores both vertebral disc height and foraminal height, and also leads to an osseous fusion [3, 4].
ACDF using a polyetheretherketone (PEEK) cage is considered by many spinal surgeons, as the gold standard for patients with cervical disc herniation. PEEK is biocompatible, radiolucent, and has a modulus of elasticity similar to that of the bone. PEEK cages may achieve a significant increase in the disc space height and the neural foramina, contributing to nerve root decompression and, thereby, further controlling pain. In addition, the implantation of a PEEK cage is characterized by a significantly lower infection rate, compared to ACDF with an autologous bone graft [5, 6].
On the other hand, partial fusion of the cervical spine inevitably resulted in alternations to the physiological biomechanics of the area [7]. Inadequate cervical lordosis and reduced cervical range of motion (ROM) have been suggested to be significant negative contributors in the outcome of ACDF surgery [8].
Although there are several clinical and radiological studies in the literature regarding the progress of fusion, as well as the clinical improvement of patients undergoing ACDF with a PEEK cage, there are a limited number of studies, investigating the correlation of clinical improvement with cervical lordosis, and also with cervical ROM of such patients.
The purpose of our current study was to investigate the impact of altered cervical sagittal alignment (cervical lordosis) as well as the impact of cervical sagittal ROM changes, on patients’ self-reported pain and functional disability, in patients undergoing ACDF with a PEEK cage.
| Materials and Methods | ▴Top |
This was a prospective, same subjects, repeated-measures study.
Study group
The study group exclusively consisted of patients that fully completed the research protocol (6 and 12 months follow-ups). Therefore we analyzed the clinical and radiological outcomes of 74 patients, who underwent single-, or consecutive two-level ACDF using a PEEK interbody cage filled with allograft. All participants suffered cervical radiculopathy or myelopathy, which had remained unresponsive to any conservative treatment, for at least a 3-month period. The eligibility of the patients was assessed and determined by the same neurosurgeon. Demographic variables such as age, sex, and smoking habits were recorded. Radiological and clinical evaluation of the patients was preoperatively performed, at the day of their hospital discharge, and then at 6 and 12 months postoperatively. A signed informed consent was obtained from all participants before their enrolment in the study. The study protocol was conducted in agreement with the Declaration of Helsinki and approved by the scientific council of our hospital.
Assessment of outcome
Clinical evaluation
Intraoperative and postoperative complications were noted. Numeric rating scale (NRS) and the neck disability index (NDI) were used in order to obtain a time series of self-reported neck/arm pain severity and cervical spine function changes. NRS and NDI are two of the most commonly cited instruments for assessing self-rated pain and disability in patients with neck pain [9]. The above clinical outcome instruments were administered by the single blinded research assistant and without the presence of the treating surgeon.
Radiologic evaluation
The radiologic evaluation of the cervical spine in the pre- and postoperative period included lateral radiographs in neutral, and also in full active flexion-extension, in order to obtain a time series of cervical lordosis and sagittal ROM changes. On the basis of the radiographic images, we calculated the cervical lordosis in neutral and sagittal ROM of C2-C7, using the Cobb method. The Cobb angle was determined as the angle of intersection of two tangential lines drawn along the inferior end plate of the C2 and the inferior end plate of the C7. Lordosis was expressed as a positive value and kyphosis was expressed as a negative value so as sagittal ROM was determined by measuring the difference in alignment between maximum flexion and extension. Radiographic measurement data were collected from an independent observer, who was not involved in the management of these patients. Representations of the clinical and radiologic evaluation are illustrated in Table 1.
 Click to view | Table 1. Evaluation Plan |
Statistical analysis
The collected data were processed using the Statistical Package for the Social Sciences software (SPSS version 20, IBM Corporation, NY, USA). All results are presented as the mean value ± SD. The Friedman’s two-way analysis of variance methodology for non-parametric data, and the repeated measures ANOVA methodology as well as the paired samples t-test methodology for parametric data, were carried out to assess the effect of ACDF on time-related changes (preoperative, postoperative, 6, and 12 months) in cervical lordosis, sagittal ROM, pain NRS and NDI. Pearson product moment correlation coefficient methodology for parametric data and the Spearman rank order correlation coefficient methodology for non-parametric data were also used to determine the relationship between NDI and, NRS, cervical lordosis and sagittal ROM, respectively. Additionally, the statistical significance of the observed differences of the mean between subgroups was calculated by using the independent samples t-test methodology. A P value of < 0.05 was considered to be significant in all the above statistical tests.
| Results | ▴Top |
Patient demographics and surgical data
Using the inclusion/exclusion criteria presented in Table 2, 74 patients (36 males and 38 females; mean age 50.09 ± 13.54 years) with cervical radiculopathy or myelopathy, were enrolled. There was a minimum (< 20 mL) blood loss in 37 (49.3%) patients, and a mean of 75.66 ± 31.56 mL in the remaining 38 (50.7%) patients. Sixty-five patients (86.7%) used only hard cervical collar postoperatively, while the other 10 (13.3%) used hard and soft collar, sequentially. A summary of the demographics and the surgical details are presented in Table 3.
 Click to view | Table 2. Summary of Inclusion and Exclusion Criteria |
 Click to view | Table 3. Summary of Patients’ Demographic Characteristics, and Surgical Data |
Complications
In one patient (1.35%) an accidental intraoperative esophageal perforation occurred, and a surgical repair of the iatrogenic esophageal tear was performed at a different surgical setting, by a cardiothoracic surgeon. The patient stayed with no oral intake and parenteral alimentation for 6 days after his second surgery, and recovered with no further consequences. His follow-up revealed no dysphagia or any other esophageal motility difficulties. Two patients (2.7%) developed postoperatively a clinically evident soft tissue hematoma, which was conservatively managed with close observation, requiring no surgical evacuation. These two patients recovered with no further consequences. Additionally, three patients (4.05%) experienced postoperatively mild to moderate dysphagia, with one of them simultaneously presenting mild hoarseness. Their symptoms slowly improved within the first 2 - 4 postoperative weeks, and they completely resolved with no further disturbances. The cumulative complication rate in our current series was 8.1% per patient, and 7.31% per surgical level.
Clinical outcome
Neck/arm NRS scores and NDI scores were available from all participants. The difference of the observed mean between subgroups (smokers/non-smokers, myelopathy/radiculopathy, single-level fusion/two-level fusion) was statistically insignificant for any of the explored clinical parameters (Table 4). Therefore, we calculated the sample (n = 74) as homogeneous.
 Click to view | Table 4. Outcomes of Clinical Parameters for Subgroups (Mean ± SD) and the Significance of the Differences Between Subgroups |
Τhe observed mean NRS score immediately after surgery demonstrated a significant reduction from the preoperative one (P = 0.000). This reduction was maintained significant at 6 months (P = 0.000) and 12 months postoperatively (P = 0.000). Moreover, the calculated mean NDI score at the 6-month evaluation showed statistically significant reduction from the preoperative one (P = 0.000) and this reduction was maintained significant at the 12-month follow-up evaluation (P = 0.000). The changes of the clinical outcomes over time are illustrated in Figure 1 and are summarized in Table 5. Additionally, there was significant positive correlation between NRS and NDI preoperatively (r = 0.351, P = 0.001), at the 6-month follow-up evaluation (r = 0.241, P = 0.004), as well as at the 12-month follow-up evaluation (r = 0.250, P = 0.003).
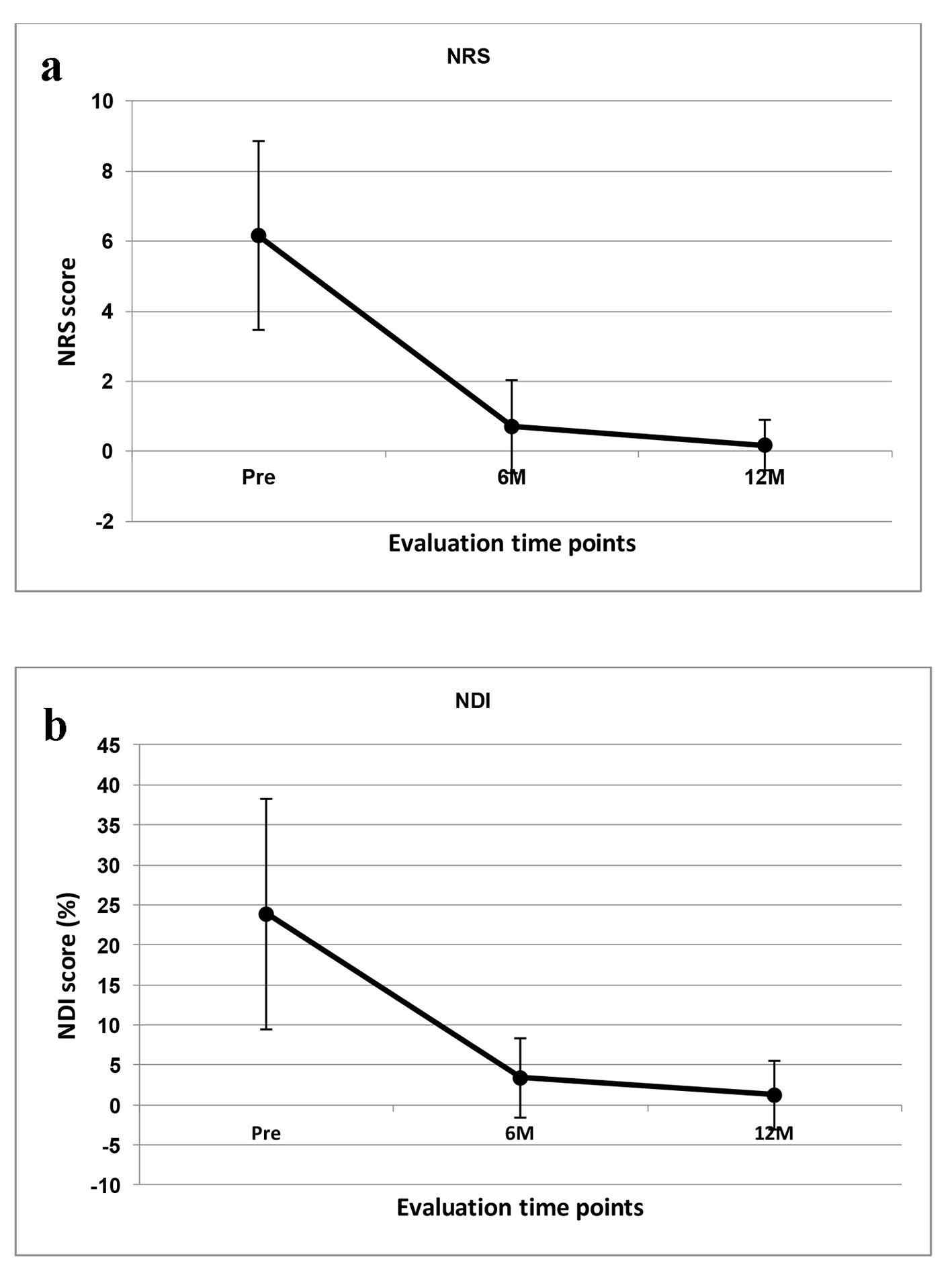 Click for large image | Figure 1. Line graphs illustrating: (a) the pain NRS mean scores and (b) the NDI mean scores preoperatively and then at 6- and 12-month time points. There was significant difference between time points for both instruments. |
 Click to view | Table 5. Outcomes of Clinical and Radiological Parameters for the Sample as a Whole (Mean ± SD) |
Radiological outcome
There was a successful implantation of a PEEK cage in all participants, with no mechanical failures or other implant associated malfunctions. Additionally, there was a successful fusion in all participants, with no pseudoarthrosis at the implantation levels until the last follow-up (12 months). The difference of the observed mean between subgroups was statistically insignificant for any of the explored radiologic parameters (Table 6). Therefore, we calculated the sample (n = 74) as homogeneous, too. A summary of the radiological results is presented in Table 5.
 Click to view | Table 6. Outcomes of Radiological Parameters for Subgroups (Mean ± SD) and the Significance of the Differences Between Subgroups |
Cervical lordosis
The mean postoperative Cobb angle from the C2 to the C7 in neutral (index of the cervical lordosis) was found to be slightly increased compared to the preoperative one. However, this difference was statistically insignificant (P = 0.429). Interestingly, the mean Cobb angle at 6 months postoperatively was lower than the respective preoperative one. However, this difference was statistically insignificant (P = 0.0095) (a P value of < 0.0083 was considered to be significant due to Bonferroni correction). At the 12-month postoperative evaluation, the mean Cobb angle was again lower than the preoperative one, and this difference reached the levels of statistical significance (P = 0.008). Additionally, there was no significant correlation between the NDI scores and the Cobb angle preoperatively (r = 0.175, P = 0.134), at 6 months postoperatively (r = 0.034, P = 0.772), and also at 12 months (r = -0.113, P = 0.335) postoperatively.
C2-C7 sagittal ROM
The 6-month follow-up mean sagittal ROM was significantly reduced compared to the preoperative one (P = 0.000) and the observed difference remained significant (P = 0.000) at the 12-month follow-up evaluation. Further processing of our data demonstrated that this reduction of the ROM was more prominent in patients undergoing two-level ACDF than those undergoing single-level ACDF (Fig. 2, Table 6). Additionally, in regard to the calculated ROM and NDI scores, there was no correlation preoperatively (r = 0.099, P = 0.199), at 6 months (r = 0.056, P = 0.322) and also at 12 months (r = -0.007, P = 0.476) postoperatively.
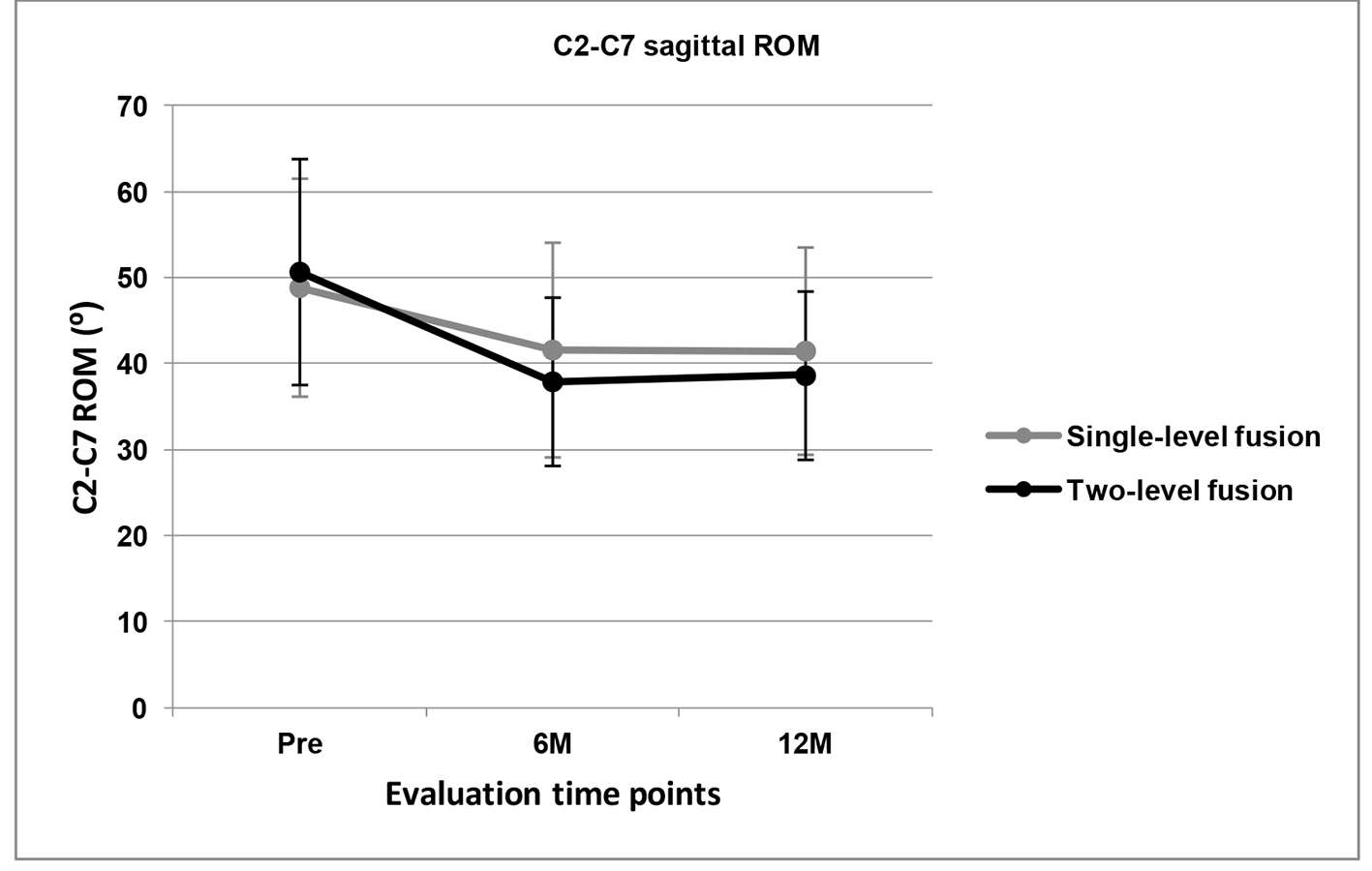 Click for large image | Figure 2. Line graphs illustrating C2-C7 ROM for the single- and two-level ACDF groups preoperatively and then at 6- and 12-month time points. There was significant difference between time points for both conditions. |
| Discussion | ▴Top |
To our knowledge, there is limited number of studies to evaluate the association of cervical lordosis and ROM with patient-reported functional disability. Contrary to the generally accepted clinical deduction, the results of the current study indicated that cervical lordosis and ROM do not exert a significant impact on patient-reported functional capacity. On the other hand, our results indicated that pain level exerts a significant impact on patient-reported functional capacity.
The essential purpose of ACDF with a PEEK cage is to decompress the spinal cord and other neural structures whilst to maintain the stability of the cervical spine. Additionally, there is strong body of evidence that PEEK cage implantation restores and successfully maintains the intervertebral disc height and also the neural foramina height, postoperatively [4, 10-12]. Therefore, the achieved mechanical decompression of the compressed cervical roots and the possible restoration of the local micro-circulation may result in pain reduction [13]. Consistent with other clinical series [4, 10, 11, 14-16], our current data clearly indicated that there was a statistically significant reduction of neck/arm pain among our patients at their discharge from the hospital. This effect was maintained during their 12-month follow-up period.
In accordance to other clinical series with similar samples and follow-up periods [17-19], our data demonstrated that there was statistically significant postoperative improvement of the NDI score. It has been postulated that the postoperative pain reduction is strongly associated with the patient’s satisfaction [14, 20]. Additionally, it is well known that NDI was designed to measure disability in activities of daily living due to neck pain [21, 22]. The above would be an explanation of our findings regarding the parallel significant reduction in neck/arm pain mean scores and NDI mean scores (Table 5, Fig. 1). There are several studies supporting the concept that NDI reduction is associated to pain reduction through the postoperative period [10, 16, 23-25] and our study results strongly support this. More specifically, there was statistically significant correlation between these variables (NDI and NRS) in the preoperatively obtained scores as well as in the postoperatively obtained scores (6- and 12-month).
It is well known that lordotic sagittal alignment of the cervical spine is absolutely necessary, in order the spine to sustain the mechanical stresses of daily-living activities. McAviney et al [26] reported statistically significant correlation between neck pain and cervical lordosis less than 20°. Additionally, according to Wu et al [27], the restoration or the maintenance of acceptable cervical lordosis after ACDF affects the long-term clinical outcome. Decreased cervical lordotic angle seems to be associated with earlier adjacent degenerative changes [28]. There are several studies in the literature examining the effect of ACDF with a PEEK cage in the management of cervical lordosis. They resulted in significant lordosis restoration postoperatively that was maintained throughout the final follow-up (12 - 24 months) [16-19]. Contrariwise, our results showed that there was a slight increase of the mean Cobb angle in neutral immediately after surgery, which however was lost during the 12-month follow-up period (Table 5). Unfortunately, we cannot identify any factors for explaining these findings in our series. An explanation for this would be the possible adjacent level degeneration [28, 29], a factor that we did not explore. Nevertheless, our current Cobb angle measurements are into acceptable limits, since the reported in the pertinent literature predictable lordotic angle values are 13.90±12.30° for healthy subjects, while 11.40±9.80° for myelopathic patients [30].
In agreement with previous studies [31, 32], patients underwent ACDF in the current study demonstrated a statistically significant reduction of the C2-C7 sagittal ROM postoperatively (6-months follow-up) which remained reduced at the 12-month follow-up evaluation (Table 5). This reduction was more prominent among patients undergoing two-level ACDF (Fig. 2, Table 6). This is in contrast with previous findings, which have reported a significant improvement in ROM following ACDF, even in those with multilevel fusions [14, 33, 34]. According to Chien et al [31], one plausible explanation for the discrepancies may lie with the differences in the method of how the ROM was obtained. Results presented in our study were based on radiographs measured through C2-C7, where the other studies have utilized external wearable devices such as a helmet with goniometers or inclinometers to obtain the global ROM. Such devices commonly include the ROM contributed from the upper cervical and cranial junction [31]. Another plausible explanation is that in the patients who underwent ACDF for radiculopathy, a pathological condition in which the pain cause reduced ROM, decreased radicular pain postoperatively results into improved postoperative ROM. Finally, on the basis of the results of the current study and known in vitro data, ACDF with a PEEK cage is likely to be associated with a reduction of sagittal ROM, which is potentially correlated with the number of fused levels [31].
A cumulative interpretation of our data indicates that our patients had improved self-reported pain intensity (NRS) and disability (NDI) profile, maintained their C2-C7 lordosis at predictable values, while they had reduced sagittal cervical ROM. Similarly, Seng et al [32] documented postoperative reduction of patient-reported pain intensity and disability, along with sagittal cervical ROM reduction. It has been previously stated that there is a relation between cervical ROM, pain and finally, disability [33]. Moreover, it has been postulated that postoperative restoration of the cervical lordosis influences the overall, long-term, clinical outcome. Based on these hypotheses, the observed improvement of patient-reported disability (NDI) in our current study should be accompanied by a restored cervical lordosis postoperatively, as well as by an increased, or at least unchanged, sagittal cervical ROM. However, in contrast to the observed positive association between patient-reported functional disability and calculated cervical lordosis and ROM in conservatively managed patients [35], our results, in accordance to other studies [33], indicated that in ACDF patients, pain levels are more strongly associated with the reported disability levels than the reduction of cervical lordosis as well as the loss of ROM. Chien et al [31] may provide an explanation for our findings, since they claim that patients tend to use their perceived pain levels instead of available ROM when attempting to determine their own functional disability levels. Therefore, such finding highlights the importance of adequate pain management postoperatively. On the other hand, pain-aggravating physical therapy techniques aiming to improve ROM may have an opponent effect on patient-perceived functional disability and should be better respected by clinicians at postoperative periods.
Limitations
One notable limitation of our study involves the possibility of deficiencies in our method of measuring cervical ROM. Cervical movement is multidirectional, but in our study, radiographic analysis of ROM in only one plane was calculated. Multidirectional movements, including rotational motion and lateral bending, were not considered.
Conclusions
Despite the inherent limitations, this study extends our current knowledge base on how changes on pain intensity and also kinematical changes after ACDF influence on patient-reported outcomes. Our results suggest that the employment of ACDF with a PEEK cage successfully reduced the preoperative neck/radicular pain, as well as the patient’s preoperative associated disability. At the same time, it reduced cervical lordosis (however at predictable values), and decreased the sagittal cervical ROM postoperatively. Nevertheless, reduction of cervical lordosis and sagittal ROM did not appear to significantly influence on patients’ self-reported disability. Finally, such findings further highlight the greater role of pain level over the mechanical limitations of ACDF with a PEEK cage on patients’ own perceived recovery.
Competing Interests
The authors declare that they have no competing interests.
Grant Support
None.
Financial Disclosure
None.
| References | ▴Top |
- Schroeder GD, Kurd MF, Millhouse PW, Vaccaro AR, Hilibrand AS. Performing an anterior cervical discectomy and fusion. Clin Spine Surg. 2016;29(5):186-190.
pubmed - Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, Lee GP, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007;32(21):2310-2317.
doi pubmed - Xie JC, Hurlbert RJ. Discectomy versus discectomy with fusion versus discectomy with fusion and instrumentation: a prospective randomized study. Neurosurgery. 2007;61(1):107-116; discussion 116-107.
- Gok H, Onen MR, Yildirim H, Gulec I, Naderi S. Empty bladed PEEK cage for interbody fusion after anterior cervical discectomy. Turk Neurosurg. 2016;26(1):105-110.
pubmed - Park HW, Lee JK, Moon SJ, Seo SK, Lee JH, Kim SH. The efficacy of the synthetic interbody cage and Grafton for anterior cervical fusion. Spine (Phila Pa 1976). 2009;34(17):E591-595.
doi pubmed - Landriel FA, Hem S, Goldschmidt E, Ajler P, Vecchi E, Carrizo A. Polyetheretherketone interbody cages versus autogenous iliac crest bone grafts with anterior fixation for cervical disc disease. J Spinal Disord Tech. 2013;26(2):61-67.
doi pubmed - Nunley PD, Jawahar A, Kerr EJ, 3rd, Gordon CJ, Cavanaugh DA, Birdsong EM, Stocks M, et al. Factors affecting the incidence of symptomatic adjacent-level disease in cervical spine after total disc arthroplasty: 2- to 4-year follow-up of 3 prospective randomized trials. Spine (Phila Pa 1976). 2012;37(6):445-451.
doi pubmed - Miyazaki M, Hymanson HJ, Morishita Y, He W, Zhang H, Wu G, Kong MH, et al. Kinematic analysis of the relationship between sagittal alignment and disc degeneration in the cervical spine. Spine (Phila Pa 1976). 2008;33(23):E870-876.
doi pubmed - Cleland JA, Fritz JM, Whitman JM, Palmer JA. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine (Phila Pa 1976). 2006;31(5):598-602.
doi pubmed - Park JH, Roh SW. Anterior cervical interbody fusion using polyetheretherketone cage filled with autologous and synthetic bone graft substrates for cervical spondylosis: comparative analysis between PolyBone(R) and iliac bone. Neurol Med Chir (Tokyo). 2013;53(2):85-90.
doi - Guven M, Cosar M, Alkan B, Aras AB, Akman T, Safak O, Karaarslan O, et al. Comparison of anterior cervical discectomy fusion techniques: bladed and non bladed PEEK cages. Turk Neurosurg. 2016;26(3):404-410.
pubmed - Toth JM, Wang M, Estes BT, Scifert JL, Seim HB, 3rd, Turner AS. Polyetheretherketone as a biomaterial for spinal applications. Biomaterials. 2006;27(3):324-334.
doi pubmed - Jacobs W, Willems PC, van Limbeek J, Bartels R, Pavlov P, Anderson PG, Oner C. Single or double-level anterior interbody fusion techniques for cervical degenerative disc disease. Cochrane Database Syst Rev. 2011;1:CD004958.
- Hessler C, Boysen K, Regelsberger J, Vettorazzi E, Winkler D, Westphal M. Patient satisfaction after anterior cervical discectomy and fusion is primarily driven by relieving pain. Clin J Pain. 2012;28(5):398-403.
doi pubmed - Han SY, Kim HW, Lee CY, Kim HR, Park DH. Stand-alone cages for anterior cervical fusion: are there no problems? Korean J Spine. 2016;13(1):13-19.
doi pubmed - Faldini C, Chehrassan M, Miscione MT, Acri F, d’Amato M, Pungetti C, Luciani D, et al. Single-level anterior cervical discectomy and interbody fusion using PEEK anatomical cervical cage and allograft bone. J Orthop Traumatol. 2011;12(4):201-205.
doi pubmed - Chen Y, Lu G, Wang B, Li L, Kuang L. A comparison of anterior cervical discectomy and fusion (ACDF) using self-locking stand-alone polyetheretherketone (PEEK) cage with ACDF using cage and plate in the treatment of three-level cervical degenerative spondylopathy: a retrospective study with 2-year follow-up. Eur Spine J. 2016;25(7):2255-2262.
doi pubmed - Liu Y, Wang H, Li X, Chen J, Sun H, Wang G, Yang H, et al. Comparison of a zero-profile anchored spacer (ROI-C) and the polyetheretherketone (PEEK) cages with an anterior plate in anterior cervical discectomy and fusion for multilevel cervical spondylotic myelopathy. Eur Spine J. 2016;25(6):1881-1890.
doi pubmed - Zhang L, Wang J, Tao Y, Feng X, Yang J, Zhang S. Outcome evaluation of zero-profile implant compared with an anterior plate and cage used in anterior cervical discectomy and fusion: a two-year follow-up study. Turk Neurosurg. 2016;26(3):416-422.
pubmed - Lied B, Roenning PA, Sundseth J, Helseth E. Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage). BMC Surg. 2010;10:10.
doi pubmed - MacDermid JC, Walton DM, Avery S, Blanchard A, Etruw E, McAlpine C, Goldsmith CH. Measurement properties of the neck disability index: a systematic review. J Orthop Sports Phys Ther. 2009;39(5):400-417.
doi pubmed - Trouli MN, Vernon HT, Kakavelakis KN, Antonopoulou MD, Paganas AN, Lionis CD. Translation of the Neck Disability Index and validation of the Greek version in a sample of neck pain patients. BMC Musculoskelet Disord. 2008;9:106.
doi pubmed - Abbas SF, Spurgas MP, Szewczyk BS, Yim B, Ata A, German JW. A comparison of minimally invasive posterior cervical decompression and open anterior cervical decompression and instrumented fusion in the surgical management of degenerative cervical myelopathy. Neurosurg Focus. 2016;40(6):E7.
doi pubmed - Burkhardt BW, Brielmaier M, Schwerdtfeger K, Sharif S, Oertel JM. Smith-Robinson procedure with an autologous iliac crest for degenerative cervical disc disease: a 28-year follow-up of 95 patients. World Neurosurg. 2016;92:371-377.
doi pubmed - Hisey MS, Zigler JE, Jackson R, Nunley PD, Bae HW, Kim KD, Ohnmeiss DD. Prospective, randomized comparison of one-level Mobi-C cervical total disc replacement vs. anterior cervical discectomy and fusion: results at 5-year follow-up. Int J Spine Surg. 2016;10:10.
doi pubmed - McAviney J, Schulz D, Bock R, Harrison DE, Holland B. Determining the relationship between cervical lordosis and neck complaints. J Manipulative Physiol Ther. 2005;28(3):187-193.
doi pubmed - Wu WJ, Jiang LS, Liang Y, Dai LY. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J. 2012;21(7):1374-1382.
doi pubmed - Park MS, Kelly MP, Lee DH, Min WK, Rahman RK, Riew KD. Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J. 2014;14(7):1228-1234.
doi pubmed - Hwang SH, Kayanja M, Milks RA, Benzel EC. Biomechanical comparison of adjacent segmental motion after ventral cervical fixation with varying angles of lordosis. Spine J. 2007;7(2):216-221.
doi pubmed - Machino M, Yukawa Y, Imagama S, Ito K, Katayama Y, Matsumoto T, Inoue T, et al. Age-related and degenerative changes in the osseous anatomy, alignment, and range of motion of the cervical spine: a comparative study of radiographic data from 1016 patients with cervical spondylotic myelopathy and 1230 asymptomatic subjects. Spine (Phila Pa 1976). 2016;41(6):476-482.
doi pubmed - Chien A, Lai DM, Wang SF, Hsu WL, Cheng CH, Wang JL. Comparison of cervical kinematics, pain, and functional disability between single- and two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2016;41(15):E915-922.
doi pubmed - Seng C, Tow BP, Siddiqui MA, Srivastava A, Wang L, Yew AK, Yeo W, et al. Surgically treated cervical myelopathy: a functional outcome comparison study between multilevel anterior cervical decompression fusion with instrumentation and posterior laminoplasty. Spine J. 2013;13(7):723-731.
doi pubmed - Landers MR, Addis KA, Longhurst JK, Vom Steeg BL, Puentedura EJ, Daubs MD. Anterior cervical decompression and fusion on neck range of motion, pain, and function: a prospective analysis. Spine J. 2013;13(11):1650-1658.
doi pubmed - Hilibrand AS, Balasubramanian K, Eichenbaum M, Thinnes JH, Daffner S, Berta S, Albert TJ, et al. The effect of anterior cervical fusion on neck motion. Spine (Phila Pa 1976). 2006;31(15):1688-1692.
doi pubmed - Nordin M, Carragee EJ, Hogg-Johnson S, Weiner SS, Hurwitz EL, Peloso PM, Guzman J, et al. Assessment of neck pain and its associated disorders: results of the Bone and Joint Decade 2000-2010 Task Force on neck pain and its associated disorders. J Manipulative Physiol Ther. 2009;32(2 Suppl):S117-140.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.











