| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Case Report
Volume 10, Number 1, January 2018, pages 63-65
Idiopathic Isolated Colonic Varices: An Extremely Rare Condition
Tagore Sunkaraa, d, Megan E. Caugheyb, Andrea Cullifordc, Vinaya Gaduputic
aDivision of Gastroenterology and Hepatology, The Brooklyn Hospital Center, Clinical Affiliate of The Mount Sinai Hospital, 121 Dekalb Ave, Brooklyn, NY 11201, USA
bNew York Institute of Technology College of Osteopathic Medicine, Old Westbury, NY, USA
cDivision of Gastroenterology and Hepatology, SBH Health System, 4422 Third Ave, Bronx, NY 10457, USA
dCorresponding Author: Tagore Sunkara, Division of Gastroenterology and Hepatology, The Brooklyn Hospital Center, Clinical Affiliate of The Mount Sinai Hospital, 121 Dekalb Avenue, Brooklyn, NY 11201, USA
Manuscript submitted October 20, 2017, accepted November 7, 2017
Short title: Idiopathic Isolated Colonic Varices
doi: https://doi.org/10.14740/jocmr3230w
| Abstract | ▴Top |
Colonic varices are an incredibly rare phenomenon to begin with; however, they are even more unusual when isolated and occurring in the absence of common comorbidities, like portal hypertension or portal vein thrombosis. We present a case of a 71-year-old female, who was asymptomatic and referred to gastroenterology for a routine colorectal cancer screening. The patient was ultimately found to have this anomalous condition when colonic varices were first identified on colonoscopy. Since these varices did not result from any obvious etiology, they were determined to be idiopathic colonic varices, an especially unusual presentation.
Keywords: Colonic varices; Idiopathic varices; Isolated varices; Ectopic varices; Colon; Hematochezia
| Introduction | ▴Top |
Ectopic varices are a term used to describe any portosystemic collateral veins that are dilated, circuitous, and located outside of the gastro-esophageal region. These varices are often caused by portal hypertension secondary to liver cirrhosis, but it is estimated that only 3.4% of patients with intrahepatic portal hypertension also have colonic varices [1]. This means that even within the context of liver cirrhosis or portal hypertension, colonic varices are an uncommon occurrence. It would reason then that idiopathic colonic varices, or those of no clear origin, represent a particularly rare condition, as described in the patient that we report here.
| Case Report | ▴Top |
A 71-year-old woman with a past medical history of obesity, hyperlipidemia, and type 2 diabetes mellitus, first presented to the gastroenterology clinic for a colorectal cancer screening. The patient stated that her last colonoscopy was 15 years ago and resulted in the removal of one polyp. No pertinent findings were observed on clinical examination, and the patient denied any abdominal pain, nausea, vomiting, diarrhea, or changes in weight. The patient cited regular bowel movements, and also denied any hematemesis or melena. She did though recall experiencing a few episodes of hematochezia 1 month earlier.
Colonoscopy revealed the presence of a 4 mm polyp in the transverse colon and a 3 mm polyp in the descending colon in addition to non-bleeding small internal hemorrhoids. Both polyps were removed with a biopsy forceps. In addition to these polyps, it was discovered on colonoscopy that the patient had multiple large colonic varices throughout the colon extending from ascending colon to the sigmoid colon (Fig. 1). In the absence of any underlying pathology, these prominent colonic varices are consistent with a diagnosis of idiopathic colonic varices. The pathology report revealed that both polyps were tubular adenomas, and the patient was instructed to increase dietary fiber consumption. A CT of the abdomen and pelvis with contrast was scheduled to better evaluate abdominal vasculature, and results from this imaging determined showed no abnormalities.
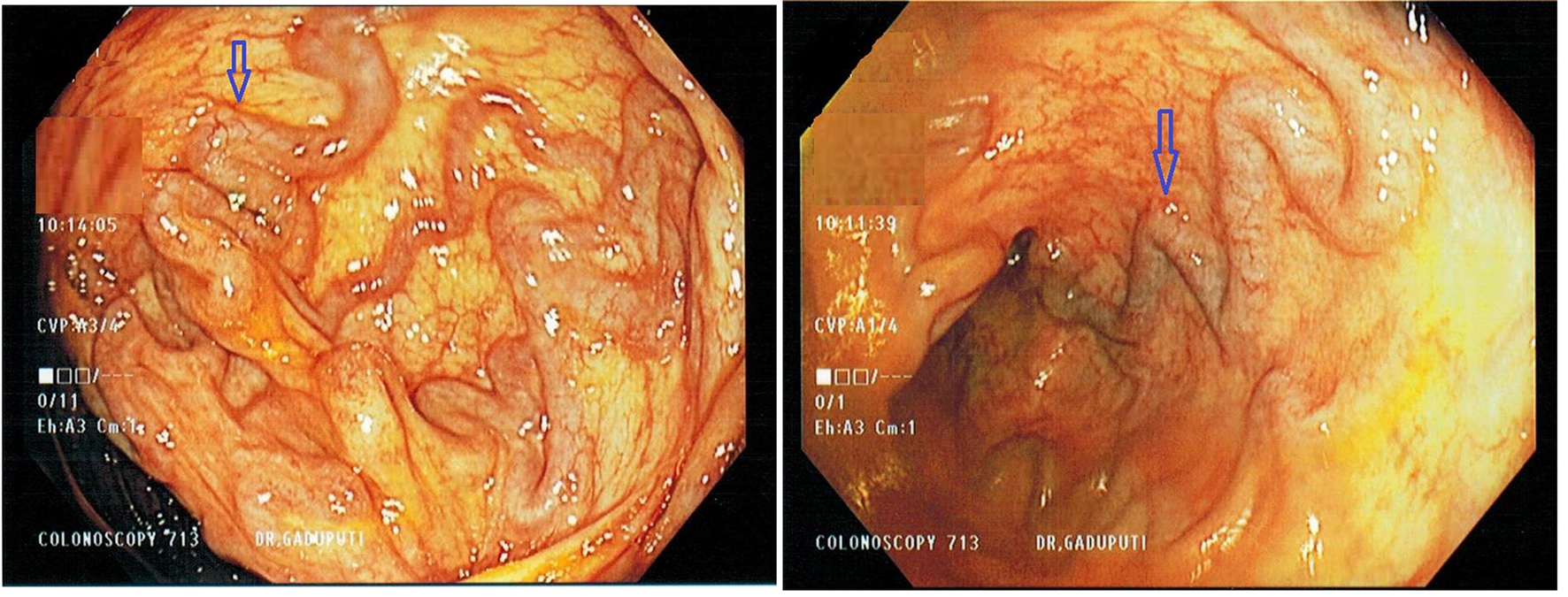 Click for large image | Figure 1. Colonoscopy showing colonic varices. |
| Discussion | ▴Top |
As previously explained, varices of the colon are an atypical cause of lower gastrointestinal bleeding. In the unlikely event that varices are identified within the colon, they are usually seen in association with liver cirrhosis, portal hypertension, or portal vein occlusion. Biliary atresia and mesenteric vein thrombosis are also seen in conjunction with colonic varices [1]. One study estimated that regardless of etiology, colonic varices have an incidence rate of only 0.07% [2]. Patients with colonic varices typically present with hematochezia or blood in the rectum, which may or may not be accompanied by pain. Idiopathic colonic varices, which cannot be explained by an underlying pathology, may also cause recurrent episodes of lower gastrointestinal bleeding [3]. It is not unusual for patients to first present with a massive gastrointestinal bleed, which is why practitioners must recognize the potential for varices within the colon, even in the absence of portal hypertension or varices elsewhere [4]. The patient in this case report had cited a few instances of hematochezia months earlier. However, aside from these instances, she was largely asymptomatic, which could mean that her colonic varices went undetected for a period of time.
It has been observed that non-idiopathic colonic varices occur equally in males and females and are usually diagnosed after age 50. Idiopathic colonic varices though are seen more often in males at a younger age, with a median age of diagnosis being 41.3 years [5]. The patient that we present here was not only female, but also diagnosed at the age of 71. Idiopathic colonic varices exhibit a much stronger familial association compared to non-idiopathic colonic varices and are more likely to be pan-colonic. A case report from 2013 found evidence of only 38 total documented instances of idiopathic colonic varices in the literature [3]. Aside from being identified as either idiopathic or non-idiopathic, colonic varices can also be described as isolated if they are identified in the absence of esophageal or other ectopic varices. It has been estimated that since 1954, there have only been around 100 reports of isolated colonic varices [6].
A variety of modalities can be used to diagnose colonic varices, some of which include routine and capsule endoscopy, barium enema, nuclear scintigraphy, CT and CT angiography, endoscopic ultrasound, and color Doppler-flow imaging (CDUS).Of these diagnostic options, CT angiography may exhibit the greatest potential because it locates varices in a manner that is both precise and minimally invasive [7]. Selective mesenteric angiography also allows for therapeutic intervention at the time of diagnosis [8]. Most often in practice, however, a colonoscopy is performed to identify colonic varices. Caution must be taken to ensure that the varices are not mistaken for a tumor or compressed during insufflation and missed [9].
The treatment for colonic varices is largely symptomatic management coupled with addressing the underlying pathology that may have caused the varices in the first place. To control episodes of active variceal bleeding, sclerotherapy, band ligation, and surgical resection can be performed. For those with less severe bleeding, adjustments like prescribing a laxative to soften stool in addition to an oral iron supplement have been shown to be effective. Patients who remain hemodynamically stable but are refractory to conservative treatment may respond well to sclerotherapy [10].
Author Contributions
Conception and design: Tagore Sunkara, Megan E. Caughey, Andrea Culliford, and Vinaya Gaduputi. Drafting of the article: Tagore Sunkara, Megan E. Caughey, Andrea Culliford, and Vinaya Gaduputi. Critical revision of the article for important intellectual content: Tagore Sunkara and Vinaya Gaduputi. Final approval of the article: Tagore Sunkara, Megan E. Caughey, Andrea Culliford, and Vinaya Gaduputi.
Disclosures
None.
Prior Presentation
It was presented as a poster at American College of Gastroenterology (ACG) in World Congress of Gastroenterology in Orlando, FL on October 16th, 2017.
Approval
This case report was approved by the institute’s Institutional Review Board as per its policy.
Consent
Informed consent for participation was obtained from this patient.
Conflict of Interest
None of the authors have any financial conflicts of interest.
| References | ▴Top |
- McCormack TT, Bailey HR, Simms JM, Johnson AG. Rectal varices are not piles. Br J Surg. 1984;71(2):163.
doi pubmed - Grasso E, Sciolli L, Ravetta F, Pelloni A. A rare case of idiopathic colonic varices: case report and review of the literature. Chirurgia. 2012;25(2):111-114.
- Speicher MV, Keegan MT, Kirk KE. A case of idiopathic colonic varices. J Am Osteopath Assoc. 2014;114(1):56-59.
doi pubmed - Krishna RP, Singh RK, Ghoshal UC. Recurrent lower gastrointestinal bleeding from idiopathic ileocolonic varices: a case report. J Med Case Rep. 2010;4:257.
doi pubmed - Francois F, Tadros C, Diehl D. Pan-colonic varices and idiopathic portal hypertension. J Gastrointestin Liver Dis. 2007;16(3):325-328.
pubmed - El-Masry M, Hu R. Cecal varices presenting as anemia: case report and review of the literature. Case Rep Gastroenterol. 2010;4(3):524-527.
doi pubmed - Haddad JD, Lacey BW. Isolated non-hemorrhagic cecal varices. Gastroenterol Rep (Oxf). 2014;2(4):316-319.
doi pubmed - Cherian MP, Mehta P, Kalyanpur TM, Hedgire SS, Narsinghpura KS. Arterial interventions in gastrointestinal bleeding. Semin Intervent Radiol. 2009;26(3):184-196.
doi pubmed - Feldman M, Sr., Smith VM, Warner CG. Varices of the colon. Report of three cases. JAMA. 1962;179:729-730.
doi pubmed - Chowdhury AMM, Yue Z, Ying C, Min L. Idiopathic colonic varices: a rare case report. Colorec Cancer. 2016;2(2):1-3.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.











