| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Case Report
Volume 9, Number 3, March 2017, pages 225-228
Septic Shock of Unknown Origin: A Case Report of a Pseudoaneurysm of the Mitral-Aortic Intervalvular Fibrosa
Julio Gila, b, Hugo Antunesa, Bruno Marmeloa, Luis Abreua, Maria Luisa Goncalvesa, Luis Ferreira dos Santosa, Jose Costa Cabrala
aCardiology Department, Tondela-Viseu Hospital Centre, Viseu, Portugal
bCorresponding Author: Julio Gil Goncalves Pereira, Cardiology Department, Tondela-Viseu Hospital Centre, Av. Rei D. Duarte, Postal Code 3500 Viseu, Portugal
Manuscript accepted for publication January 10, 2017
Short title: P-MAIVF
doi: https://doi.org/10.14740/jocmr2903w
| Abstract | ▴Top |
Pseudoaneurysm of the mitral-aortic intervalvular fibrosa (P-MAIVF) is a rare complication of infective endocarditis and trauma, particularly of aortic valve surgery. Clinical symptoms are usually unspecific and generally due to complications. Transesophageal echocardiography (TEE) is the most commonly used exam to diagnose P-MAIVF. The main echocardiographic feature is the presence of a cavity communicating with the left ventricular outflow tract that expands during systole and collapses during diastole. Most frequent complications are formation of a fistulous tract and compression of adjacent structures. Surgical correction is usually the treatment of choice. The authors describe a case of a female patient with a septic shock of unclear origin. After antibiotic therapy and organ-supporting measures without apparent improvements, a TEE revealed infective endocarditis, complicated with P-MAIVF. Despite adequate treatment, the patient did not survive for long enough to be submitted to surgical repair.
Keywords: Pseudoaneurysm; Infective endocarditis; Mitral-aortic intervalvular fibrosa
| Introduction | ▴Top |
Pseudoaneurysm of the mitral-aortic intervalvular fibrosa (P-MAIVF) is an uncommon but possibly deadly condition. The mitral-aortic intervalvular fibrosa is a region of avascular nature and especially vulnerable to trauma or infection. Infective endocarditis and trauma, especially surgical trauma are the most frequent causes of P-MAIVF. P-MAIVF is usually clinically silent, unless it develops complications. Symptoms can range from signs of infection, chest pain, heart failure or stroke. The most common complications are fistula formation and compression of nearby structures.
Diagnosis is usually attained through echocardiographic imaging. Transesophageal echocardiography (TEE) has a higher sensitivity at diagnosing P-MAIVF and it is also more accurate at describing possible complications. The main echocardiographic feature of the P-MAIVF is the occurrence of an echo-free space with pulsatility that expands in systole and collapses in diastole. Coronary angiography may detect coronary systolic compression and cardiac magnetic resonance and computerized tomography may provide additional characterization of the P-MAIVF. Recommended treatment is surgery. Aortic valve replacement with P-MAIVF repair is the most commonly used procedure. There are a few reports of percutaneous closure with success.
The authors describe a case of a septic shock of unclear origin. There were no improvements despite optimal therapy with antibiotic and organ-supporting measures. Since diagnosis was not evident, a TEE was performed which revealed it to be a case of infective endocarditis complicated with P-MAIVF.
| Case Report | ▴Top |
An 81-year-old woman, with a past medical history of hypertension, dyslipidemia, asthma and degenerative valve disease, presented to the emergency department (ER) for acute pre-cordial pain and dyspnea. The patient reported nausea and vomiting, but denied aspiration. On physical exam, the patient was hemodynamically stable. However, she presented with a fever of 38.7 °C and signs of respiratory distress. Blood gas analysis revealed hypoxemia. Further blood work showed elevated inflammatory parameters and chest X-ray revealed left pleural effusion. The patient was admitted with a presumed diagnosis of aspiration pneumonia. She began antibiotic treatment with amoxicillin and clavulanate acid. Blood cultures were collected.
During hospitalization, blood work showed elevation of the troponin level (peak 6.88 ng/mL, reference level < 0.04 ng/mL). This was interpreted as a type 2 myocardial infarction. The patient underwent transthoracic echocardiography (TTE). The exam revealed a bad acoustic window and described degenerative valve disease with moderate to severe aortic disease and important mitral valve calcification with moderate insufficiency. At day 4 of hospitalization, there was worsening of the dyspnea and hypoxia alongside with chest pain. A chest computed tomography (CT) was performed that excluded acute pulmonary embolism, but revealed extensive parenchymal consolidation of the left lung. Antibiotic treatment was altered to meropenem, combined with azithromycin. However, the patient remained hypoxemic with worsening signs of respiratory distress. She was admitted to the intensive care unit (ICU) to be mechanically ventilated. New blood cultures were collected.
After intubation, the patient developed circulatory shock, requiring noradrenalin. On the eighth day after ICU admission, chest X-ray revealed bilateral infiltrates. The patient underwent bronchofibroscopy and a bronchial lavage. Sputum was collected for microbiology testing. Both blood and the lavage cultures were negative. Eventually a cycle of corticosteroids was initiated, considering the possibility of an excessive post-infectious inflammatory process versus interstitial lung disease. However, the patient continued to worsen. After 3 days of steroid medication, the patient continued febrile and chest X-ray revealed progressive lung infiltrates. Steroids were suspended.
Since TTE revealed exuberant valve calcification, a TEE was performed on day 16. The TEE confirmed important degenerative valve disease with severe aortic stenosis. The TEE also revealed P-MAIVF, with important expansibility (Fig. 1a, b). There was also evidence of a solution of continuity, which created a severe mitral regurgitation jet (Fig. 1d). Another mass in the tricuspid valve was found (Fig. 1c), probably due to infection.
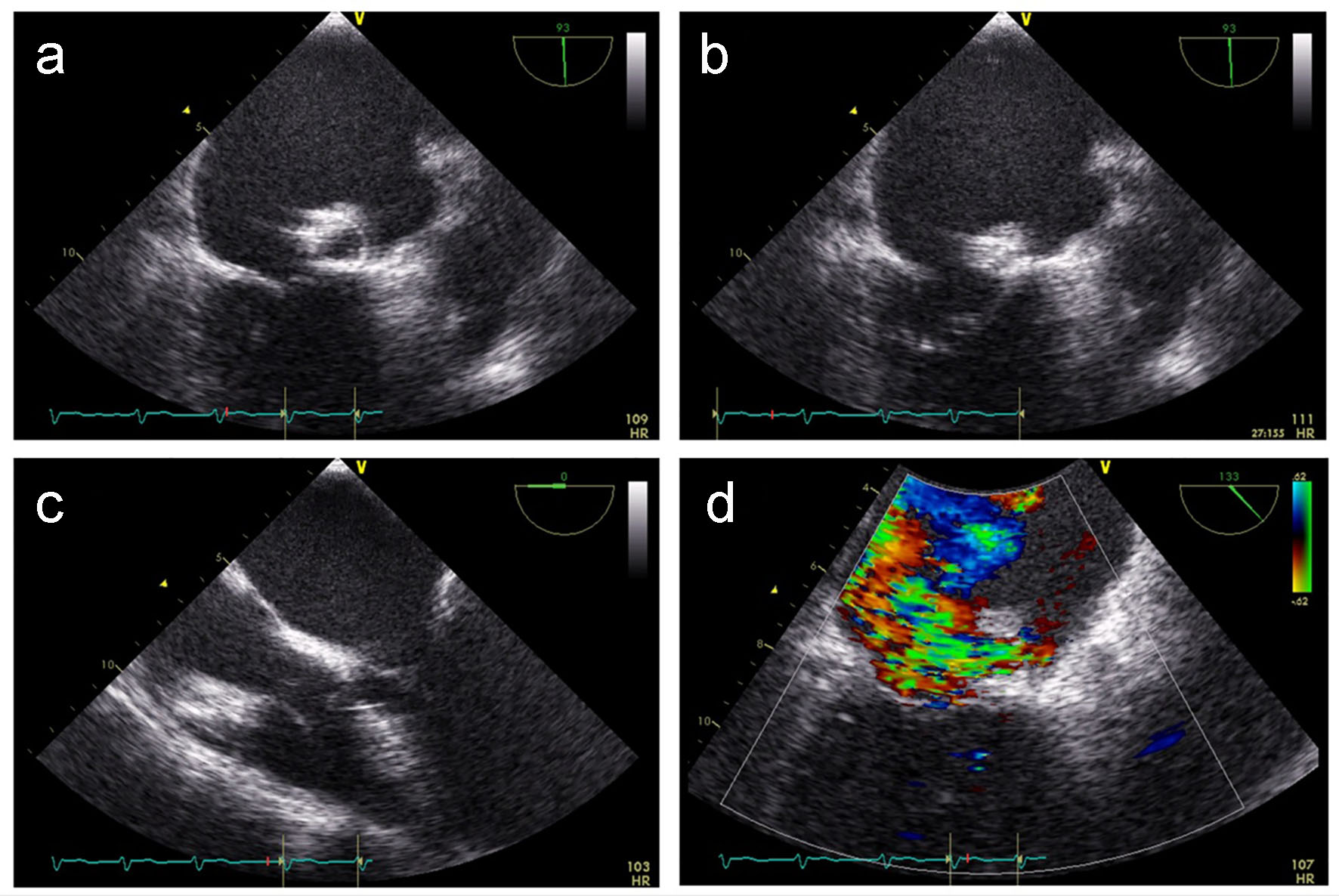 Click for large image | Figure 1. Transesophageal echocardiography. |
Despite antibiotic therapy and aminergic and ventilation support, there were no clinical improvements. The patient died at day 20 of hospitalization.
| Discussion | ▴Top |
P-MAIVF is an uncommon but possibly deadly complication of infective endocarditis [1-13].
The MAIVF pertains a fibrous area of the heart between the non-coronary and left coronary cusps of the aortic valve and the anterior mitral leaflet [1-2, 5]. The region has a relative avascular nature. Therefore, it is vulnerable to trauma or infection [1, 3, 5]. The P-MAIVF may extend through the left atrium, ascending aorta, the pulmonary artery and the pericardial space [1, 3].
Infection and trauma are the most frequent causes of P-MAIVF [1-5]. Infection leads to abscess and pseudoaneurysm formation in the MAIVF region and possible fistula development between the left ventricular outflow tract and the left atrium [1-4]. Both active and prior endocarditis can be the causative factor. The aortic valve is most frequently affected, followed by the mitral valve [1]. Endocarditis of the aortic valve may extend directly into the MAIVF area or it may be spread through the infected regurgitant jet [1, 3]. Bicuspid aortic valve appears to be more susceptible to P-MAIVF in probable relation to congenital weakness in the MAIVF area [1, 3]. The most frequent infectious agents are Staphylococcus aureus, Streptococci, Tubercle bacillus, Enterococcus, Brucella suis, Paecilomyces lilacinus, Monilia albicans and Bacillus spp [1].
Previous cardiac surgery is also a cause of P-MAIVF [1-4]. Aortic valve surgery is the most frequent condition, but other procedures have been associated with P-MAIVF, including ventricular septal defect repair, Ross/Konno procedure, cardiac catheterization, radio-frequency catheter ablation of atrial fibrillation, and mitral valve surgery with maze procedure [1]. Chest trauma has been described as the basis for the P-MAIVF formation [1-4, 12].
Uncomplicated P-MAIVFs are usually asymptomatic [1, 3]. The most common clinical manifestations, such as infection, chest pain, heart failure and stroke, are due to complications [1, 3]. Frequent complications are fistula formation and compression of nearby structures [1, 3]. Compression of a coronary artery can lead to angina or infarction [1, 3]. Compression of pulmonary artery may lead to pulmonary hypertension and compression of mitral valve may result in mitral regurgitation [1]. Fistula formation into the left atrium may create an eccentric jet that can mimic mitral regurgitation [1]. Fistula with the aorta may result in a less visible pulsatility of the pseudoaneurysm, when compared to the unruptured P-MAIVF [1, 3]. There can also be rupture into pericardial space and pericardial tamponade [1, 3, 5]. Systemic embolism can arise from intra-aneurysms clots [1]. The complications are enlisted in Table 1. There is a higher risk of P-MAIVF progression and complication associated with active infectious endocarditis, P-MAIVF greater than 3 cm, bicuspid aortic valve, aortic regurgitation, fistula formation to cardiac chamber or aorta, thrombus formation in P-MAIVF, and compression of adjacent structures [3].
 Click to view | Table 1. Complications of P-MAIVF |
Echocardiography plays an important role in the diagnosis of P-MAIVF [1-13]. Whenever aortic valve endocarditis is suspected, a TEE should be performed to exclude P-MAIVF [2]. TTE has a diagnostic sensitivity of 43% to identify P-MAIVF and TEE a sensitivity of 90% [1, 2, 6]. TEE can also identify more precisely other complications, including the presence of fistula or abscess, eccentric regurgitant jets and mitral valve perforation [1, 2, 6]. The P-MAIVF is presented through an echo-free space with pulsatility, showing expansion during systole and collapse during diastole [1-7]. When there is fistula formation, pulsatility may be less prominent, since pressure variation within the P-MAIVF is reduced [1, 3]. Three-dimensional TEE can give information about the anatomical relationship of the P-MAIVF and the surrounding tissue [1, 2].
Other imaging methods can be used to help in the diagnosis. Left ventriculography has been used to diagnose P-MAIVF in previous studies [1]. Coronary angiography is a crucial preoperative exam, since it can exclude atherosclerotic disease and coronary systolic compression [1, 3]. Cardiac magnetic resonance imaging and multi-dimensional CT can also play a role in the characterization of the aneurysm [1, 3, 5, 12].
Surgery is the recommended treatment of P-MAIVF [1-13]. Multiple surgical procedures have been described in literature. Aortic valve replacement with P-MAIVF repair is the most commonly used surgical approach [1, 3]. P-MAIVF is achieved through closure of the aneurysmal neck with pericardial patch or synthetic graft [1, 3]. Isolated P-MAIVF repair or combined with mitral valve replacement or coronary artery bypass grafting has also been performed [1, 3]. Aortic root replacement, heart transplantation and aneurysm resection have also been achieved [1]. There are also two reported cases of percutaneous closure by Jimenez Valero et al in 2005 and Romaguera et al in 2010 [8, 9].
The natural history of P-MAIVF is uncertain [1, 3]. Without surgery, there is higher risk of thrombus formation, aneurysm growth, endocarditis development, and less commonly, rupture [3]. Sudhakar et al argued that a close follow-up may be an option in patients with high risk for surgery who present with P-MAIVF and no associated complications or high-risk features. P-MAIVF with thick fibrous and calcific walls may be at low risk for complication development [3]. Follow-up should employ TTE and TEE for better characterization of possible complications [3].
The authors describe a case of a patient with degenerative valve disease and infectious endocarditis that developed a P-MAIVF. Even though it is an uncommon complication, P-MAIVF is associated with a worse outcome, as was confirmed by this case. The patient did not present previous clinical symptoms suggestive of infectious endocarditis and all exams pointed to a respiratory infection. The patient developed septic shock, with negative blood cultures, refractive to broad-spectrum antibiotic and organ-support treatment. After multiple unsuccessful therapy approaches, a TEE was performed which revealed the definite diagnosis of infectious endocarditis, complicated with P-MAIVF. Despite antibiotic and organ-support therapy, the patient did not survive long enough to be submitted for surgical treatment. This case demonstrates how a high degree of suspicion can be necessary to diagnose endocarditis. Even though P-MAIVFs are rare, their outcome can be devastating. Thus, it is of utmost priority to adequately characterize infectious endocarditis with TEE in order to better evaluate the presence of possible complication. Timely surgical correction is often the only option.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
| References | ▴Top |
- Xie M, Li Y, Cheng TO, Wang X, Lu Q, He L, Fu M. Pseudoaneurysm of the mitral-aortic intervalvular fibrosa. Int J Cardiol. 2013;166(1):2-7.
doi pubmed - Kassim TA, Lowery RC, Nasur A, Corrielus S, Weissman G, Sears-Rogan P, Greenberg M, et al. Pseudoaneurysm of mitral-aortic intervalvular fibrosa: two case reports and review of literature. Eur J Echocardiogr. 2010;11(3):E7.
doi pubmed - Sudhakar S, Sewani A, Agrawal M, Uretsky BF. Pseudoaneurysm of the mitral-aortic intervalvular fibrosa (MAIVF): A comprehensive review. J Am Soc Echocardiogr. 2010;23(10):1009-1018; quiz 1112.
doi pubmed - Karalis DG, Bansal RC, Hauck AJ, Ross JJ, Jr., Applegate PM, Jutzy KR, Mintz GS, et al. Transesophageal echocardiographic recognition of subaortic complications in aortic valve endocarditis. Clinical and surgical implications. Circulation. 1992;86(2):353-362.
doi pubmed - Ghersin E, Litmanovich D, Agmon Y, Milo S. Pseudoaneurysm of the mitral-aortic intervalvular fibrosa following aortic valve replacement - diagnosis and dynamic evaluation with multidetector CT and transesophageal echocardiography. Interact Cardiovasc Thorac Surg. 2005;4(6):502-504.
doi pubmed - Espinosa-Caliani JS, Montijano A, Melero JM, Montiel A. Pseudoaneurysm in the mitral-aortic intervalvular fibrosa. A cause of mitral regurgitation. Eur J Cardiothorac Surg. 2000;17(6):757-759.
doi - Afridi I, Apostolidou MA, Saad RM, Zoghbi WA. Pseudoaneurysms of the mitral-aortic intervalvular fibrosa: dynamic characterization using transesophageal echocardiographic and Doppler techniques. J Am Coll Cardiol. 1995;25(1):137-145.
doi - Jimenez Valero S, Garcia E, Gonzalez Pinto A, Delcan JL. [Percutaneous closure of pseudoaneurysm of the mitral-aortic intervalvular fibrosa]. Rev Esp Cardiol. 2005;58(12):1473-1475.
doi - Romaguera R, Slack MC, Waksman R, Ben-Dor I, Satler LF, Kent KM, Goldstein S, et al. IMAGE CARDIO MED: Percutaneous closure of a left ventricular outflow tract pseudoaneurysm causing extrinsic left coronary artery compression by transseptal approach. Circulation. 2010;121(4):e20-22.
doi pubmed - Tak T. Pseudoaneurysm of mitral-aortic intervalvular fibrosa. Clin Med Res. 2003;1(1):49-52.
doi pubmed - Strauch JT, Wippermann J, Krep H, Wahlers T. Subannular perforation after long-lasting aortic valve replacement mimicking mitral insufficiency. Ann Thorac Surg. 2008;85(1):311-313.
doi pubmed - Barranhas AD, Dias MC, Dos Santos AA, Marchiori E, Nacif MS. Pseudoaneurysm of the mitral-aortic intervalvular fibrosa presenting after chest trauma and diagnosed by cardiac magnetic resonance: a case report. J Med Case Rep. 2012;6:357.
doi pubmed - Moorthy N, Kumar S, Tewari S, Kapoor A, Sinha N. Mitral-aortic Intervalvular Fibrosa Aneurysm with Rupture into Left Atrium: An Uncommon Cause of Acute Dyspnea. Heart Views. 2012;13(1):13-15.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.











