| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Case Report
Volume 8, Number 6, June 2016, pages 475-477
Normal Pressure Hydrocephalus in a Human Immunodeficiency Virus Type 1 Patient
Kalyani Regetia, Rafay Khana, Waqas Jehangira, b, Shoaib Zafara, Abdalla Yousifa, Shuvendu Sena
aInternal Medicine Residency Program, Raritan Bay Medical Center, Perth Amboy, NJ, USA
bCorresponding Author: Waqas Jehangir, Internal Medicine Residency Program, Raritan Bay Medical Center, Perth Amboy, NJ, USA
Manuscript accepted for publication March 18, 2016
Short title: Normal Pressure Hydrocephalus
doi: http://dx.doi.org/10.14740/jocmr2528w
| Abstract | ▴Top |
Normal pressure hydrocephalus (NPH) is a relatively common disease of adulthood characterized by a typical combination of clinical and radiological findings. In this report, we discuss a 54-year-old female presenting with symptoms suggestive of NPH and found to have a history of human immunodeficiency virus (HIV) type 1. She was not treated as she was in denial state and developed NPH as a possible complication. In the literature, there has only been one reported case of HIV type 2 causing NPH; however, no relationship has been properly documented with HIV type 1. These findings bring about a question on whether NPH is associated or a complication of HIV with awareness of this association. Earlier screening of HIV can be done in patients presenting with such symptoms, thus to prevent further progression of its complications.
Keywords: Human immunodeficiency virus type 1; Ventriculomegaly; Normal pressure hydrocephalus
| Introduction | ▴Top |
Normal pressure hydrocephalus (NPH) can be a relatively common phenomenon which may present with pathologically enlarged ventricular size and normal opening pressure on lumbar puncture, and can be distinguished from obstructive or non-communicating hydrocephalus, in which there is a structural blockage of the cerebrospinal fluid (CSF) circulation within the ventricular system. It is characterized by a classic triad of dementia, gait disturbance, and urinary incontinence.
The most common secondary cause for NPH is suspected to be impaired absorption of CSF. However, the most common identified underlying causes are intraventricular and/or subarachnoid hemorrhage (either from aneurysm or trauma), and acute or ongoing chronic meningitis (from infection, cancer, or inflammatory disease). Cases like Paget’s disease at the skull base, mucopolysaccharidosis of the meninges, and achondroplasia are also rarely reported causes of NPH [1].
Only one prior case report has demonstrated a possible correlation between human immunodeficiency virus (HIV) type 2 and NPH; however, correlation has yet been made with HIV type 1. In this case report, we discuss the first ever reported presentation of a 54-year-old female with symptoms consistent with NPH, later discovered to also have untreated HIV type 1.
| Case Report | ▴Top |
A 54-year-old female with no significant past medical history presented to emergency room with complaints of nausea and dizziness. As per the family, the patient was in a normal state of health and had full functional ability 5 months prior. Thereafter, she gradually began to lose her balance and started developing short-term memory loss along with occasional episodes of urinary incontinence. The memory loss became progressively worse over the course of a few months to the point that she would rely on family members to answer questions and remind her of previous events. During questioning, it was evident that the patient would attempt to think or elaborate her thought process but was unable to recall and explain recent events. As per her family, the patient had also been increasingly losing her balance which had resulted in a progressively increased number of falls and injuries over the past 5 months. She was initially evaluated at different faculties at the initial onset of symptoms but was discharged after neurologic workup was otherwise unremarkable. The patient however continued to experience these symptoms which resulted in her losing her job and was unable to care for herself. Upon this presentation, the family elaborated that for the past 1 day she had been experiencing dizziness and episodes of vomiting.
On examination, her vital signs revealed a blood pressure of 143/80 mm Hg, pulse of 87/min, respiratory rate of 18/min, and temperature of 97.8 °F. On general examination, the patient was alert and oriented. Neurological examination showed a short-term memory loss (unable to repeat three simple words), lower extremity muscle wasting, and unsteady gait; however, there were normal power and normal reflexes, plantar responses were flexor bilaterally, and cranial nerves two to twelve were grossly intact. As mentioned, the patient had a wide based gait and relied on a cane for ambulation. Hematological, biochemical parameters, and chest radiography were within normal limits.
As the patient had clinical picture of NPH, a head CT (Fig. 1) was done which demonstrated an increase in the size of ventricles with a possibility of either atrophy or non-obstructing hydrocephalus. Further investigations of infectious causes and etiologies were ruled out. Laboratory results revealed a positive HIV type 1 test, with CD4 count of 74 and viral load of 453,310. Once the patient and her family members were informed regarding her HIV status, it became clear that the patient was in fact diagnosed with HIV in the past. Although she was informed in the past, she had remained in a denial state and had refused therapy for several years. Brain MRI (Fig. 2) was conducted and demonstrated findings of ventriculomegaly and multiple supratentorial and infratentorial foci of abnormal T2 white matter hyperintensity. A lumbar puncture was done with an opening CSF pressure of 12 cm H2O. No white cell or red cells were present. Protein and glucose concentrations were 30 and 62 mg/dL, respectively. Syphilis serology in both blood and CSF was also negative. Molecular analysis (PCR) for infectious etiologies in CSF showed an absence of cytomegalovirus, varicella-zoster, herpes simplex type 1 and type 2, Epstein-Barr, human herpes 6 and JC viruses, cryptococcus and tuberculosis. The patient’s gait was reassessed 72 h after the lumbar puncture and showed mild improvement. She was assessed by an HIV specialist and decision was made by the patient’s caregivers to initiate highly active retroviral therapy (HARRT therapy). At this time, patient was stable for discharge with further workup and management as outpatient by the HIV specialist and neurologist.
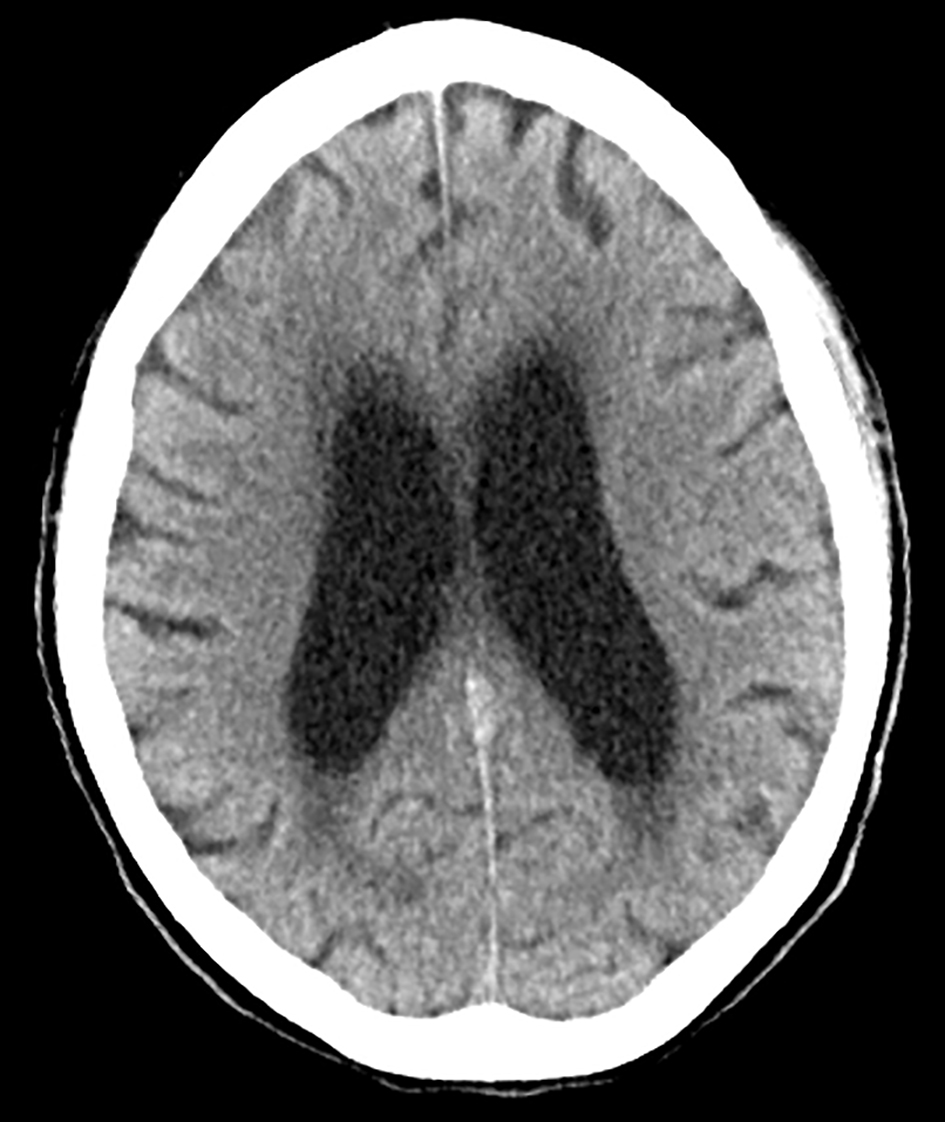 Click for large image | Figure 1. CT head showing ventriculomegaly. |
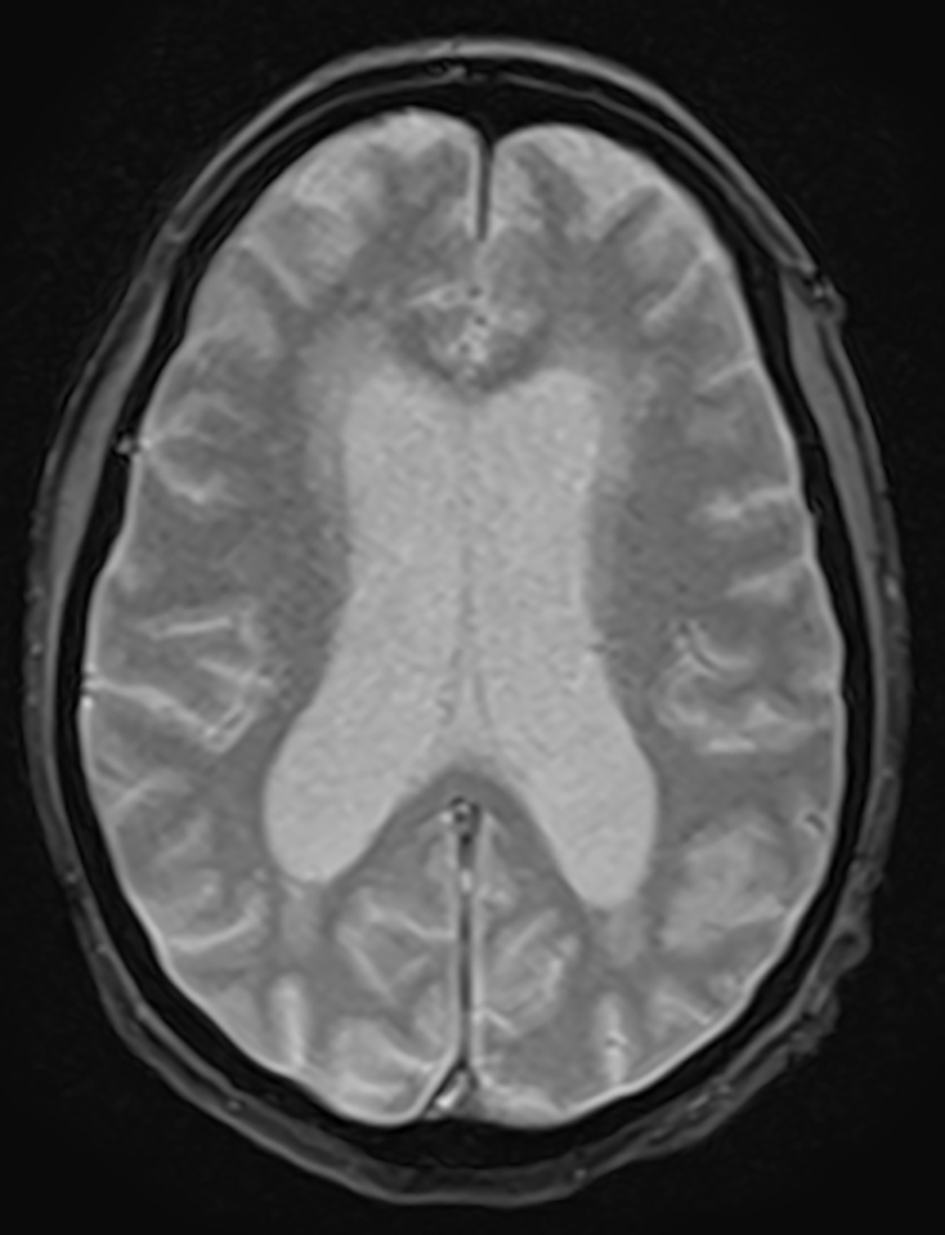 Click for large image | Figure 2. MRI of brain showing ventriculomegaly. |
| Discussion | ▴Top |
NPH is characterized by a combination of clinical and radiological findings arising in adulthood. The incidence of NPH has varied in different studies from 2 to 20 per million per year [2, 3]. The cardinal symptoms include gait impairment, dementia, and urinary incontinence.
NPH is separated into two categories: idiopathic or secondary. Idiopathic NPH is normally seen in the elderly population, while secondary NPH is seen in all age groups. Secondary causes of NPH include trauma, subarachnoid hemorrhage and meningitis. Hydrocephalus due to cerebral toxoplasmosis, cryptococcal and tuberculous meningitis in HIV patients is very rare and only few cases have been reported in the literature for HIV type 1 [4, 5]. These along with other infectious etiologies had been excluded in this patient during laboratory examination. The mechanism of hydrocephalus in central nervous system toxoplasmosis may be due to compression of CSF pathways by ring enhancing lesions, but even in their absence, hydrocephalus may be due to ventriculitis [6].
Imaging studies of the brain reveal ventriculomegaly without any marked degree of cortical atrophy [7-9]. The role of CSF shunting for obstructive hydrocephalus in HIV patients is still unclear. In a series of 30 patients with post-tuberculous hydrocephalus, Nadvi et al did not find any improvement by the CSF shunting in the HIV type 1 positive group compared with the HIV negative group [10]. One potential contributor to shunt unresponsiveness is the presence of comorbid neurological conditions that are common in HIV patients. HIV positive patients with tuberculous meningitis may undergo an external CSF drainage and after significant improvement may be considered for shunt surgery irrespective of their CD4 count [10, 11]. Another study showed successful and safe shunting in HIV type 1 patients with hydrocephalus secondary to cryptococcal meningitis [12].
However in the above patient, the hydrocephalus was of non-obstructing type which may be attributed to either ventriculitis or plexitis with an inflammatory exudates. Thus, one possible explanation in our case could be the direct effect of inflammatory cells in the CSF, affecting CSF turnover or hemodynamics. Furthermore, the patient had also been ruled out for the secondary causes of the NPH like trauma, subarachnoid hemorrhage and meningitis. Another that needs to be addressed is whether NPH itself can be a direct complication of untreated HIV. Additionally no relation between medication and hydrocephalus has been proposed. Therefore, patients with untreated HIV complicated by NPH would most likely benefit with HAART therapy as an initial management versus shunt surgery.
Conclusion
As described in the above case report, early diagnosis and treatment of NPH and its underlying cause are important to prevent the development of cognitive impairment in such patients. So the physicians should consider ordering HIV test if no other etiology of NPH is found. Physicians should be aware of this association as it may improve the prognosis of HIV and NPH in the future as it may lead to an earlier diagnosis.
| References | ▴Top |
- Hebb AO, Cusimano MD. Idiopathic normal pressure hydrocephalus: a systematic review of diagnosis and outcome. Neurosurgery. 2001;49(5):1166-1184; discussion 1184-1166.
- Krauss JK, Halve B. Normal pressure hydrocephalus: survey on contemporary diagnostic algorithms and therapeutic decision-making in clinical practice. Acta Neurochir (Wien). 2004;146(4):379-388; discussion 388.
doi pubmed - Klassen BT, Ahlskog JE. Normal pressure hydrocephalus: how often does the diagnosis hold water? Neurology. 2011;77(12):1119-1125.
doi pubmed - Eggers C, Vortmeyer A, Emskotter T. Cerebral toxoplasmosis in a patient with the acquired immunodeficiency syndrome presenting as obstructive hydrocephalus. Clin Neuropathol. 1995;14(1):51-54.
pubmed - Graybill JR, Sobel J, Saag M, van Der Horst C, Powderly W, Cloud G, Riser L, et al. Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. The NIAID Mycoses Study Group and AIDS Cooperative Treatment Groups. Clin Infect Dis. 2000;30(1):47-54.
doi pubmed - Basavaprabhu A, Soundarya M, Deepak M, Satish R. CNS toxoplasmosis presenting with obstructive hydrocephalus in patients of retroviral disease - a case series. Med J Malaysia. 2012;67(2):214-216.
pubmed - Kiefer M, Eymann R. Clinical proof of the importance of compliance for hydrocephalus pathophysiology. Acta Neurochir Suppl. 2010;106:69-73.
doi pubmed - Kiefer M, Eymann R. Huge thrombosis as a consequence of VA-shunts. Acta Neurochir Suppl. 2010;106:95-99.
doi pubmed - Cage TA, Auguste KI, Wrensch M, Wu YW, Gupta N. Self-reported functional outcome after surgical intervention in patients with idiopathic normal pressure hydrocephalus. J Clin Neurosci. 2011;18(5):649-654.
doi pubmed - Nadvi SS, Nathoo N, Annamalai K, van Dellen JR, Bhigjee AI. Role of cerebrospinal fluid shunting for human immunodeficiency virus-positive patients with tuberculous meningitis and hydrocephalus. Neurosurgery. 2000;47(3):644-649; discussion 649-650.
pubmed - Palur R, Rajshekhar V, Chandy MJ, Joseph T, Abraham J. Shunt surgery for hydrocephalus in tuberculous meningitis: a long-term follow-up study. J Neurosurg. 1991;74(1):64-69.
doi pubmed - Liao CH, Chi CY, Wang YJ, Tseng SW, Chou CH, et al. Different presentations and outcomes between HIV-infected and HIV-uninfected patients with cryptocccal meningitis. J Microbiol Immunol Infect. 2012.
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.











